Keratoconus Suspect or Pseudokeratoconus?
BY FARID EGHBALI, O.D., F.A.A.O.
DEC. 1997
Under a standard corneal topography color scale, contact lens induced corneal warpage can resemble keratoconus. Here's a new method to help you make the differential diagnosis.
Videokeratography has become an indispensable tool for the diagnosis of early, or forme fruste, keratoconus. Practitioners use this tool to rule out keratoconus and possible corneal warpage from contact lens wear (pseudokeratoconus) as a routine element of the qualifying clinical test for keratorefractive surgery. However, the differential diagnosis between pseudokeratoconus and preclinical keratoconus based on the standard color scale is somewhat difficult. This paper will demonstrate a new way of differentiating between the two using an elevation map from Humphrey Instruments' Atlas corneal topography system (version A6).
CATEGORIZING KERATOCONUS
Keratoconus can be defined as a noninflammatory thinning disorder that can lead to anterior protrusion of the cornea and visual impairment through irregular astigmatism. The protrusion of the cornea causes steepening of the central cornea which can readily be seen via videokeratography. The condition can be divided into two groups: keratoconus suspect (a local area of mild corneal steepening), and clinical keratoconus (an area of corneal steepening and one or more classic signs of Vogt's striae, corneal thinning, Fleischer's ring or retinoscopy scissors motion). Clinical keratoconus can further be divided into mild, moderate and advance stages.
TRADITIONAL METHODS OF DIFFERENTIAL DIAGNOSIS
Rabinowitz et al. (1992) suggest that videokeratography is the most sensitive means by which practitioners can diagnose keratoconus suspect, and the controversy on this issue is diminishing. Wilson et al. (1990) explain that contact lens induced corneal warpage can resemble keratoconus and that it can topographically be indistinguishable.
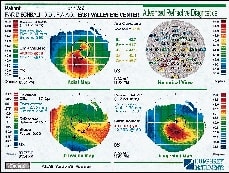
To differentiate a case of keratoconus suspect from pseudokeratoconus, the clinician customarily repeats the videokeratography at the same visit to assure repeatability and/or repeats the videokeratography after instructing the patient to discontinue contact lens wear for a set period of time. A change in the curvature of the suspected area indicates a case of pseudokeratoconus (Fig. 1 ). If there's no change, the level of suspicion for keratoconus increases. To the best of my knowledge, there's no reported way of differentiating these two similar cases without having the patient discontinue contact lens wear.
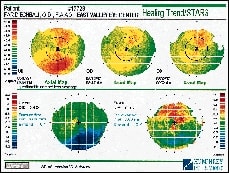
FIG. 1: TOPOGRAPHIC MAP SHOWN OVER TIME OF AN EXTENDED WEAR SOFT TORIC CONTACT LENS PATIENT. BEST CORRECTED SPECTACLE REFRACTION VISUAL ACUITY WAS SLIGHTLY REDUCED IN EACH EYE ON MAY 7, 1997 (OD>OS). AFTER DISCONTINUING THE LENSES AND REPEATING TOPOGRAPHY, THE AREA OF INFERIOR STEEPENING SHOWED A MARKED IMPROVEMENT, AND BEST CORRECTED SPECTACLE REFRACTION WAS 20/20 IN EACH EYE. |

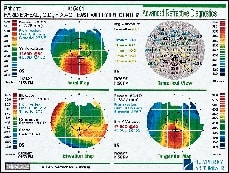
FIG. 2a: PSEUDOKERATOCONUS OR INFERIOR STEEPENING RESULTING FROM CONTACT LENS WARPAGE IN AN EXTENDED WEAR SOFT CONTACT LENS PATIENT. NOTE THE NEGATIVE VALUE IN THE ELEVATION MAP WHERE THE CROSS IS LOCATED, INDICATING A DEPRESSED AREA. AS YOU MOVE THE CURSOR AROUND IN THE STEEPENED AREA OF THE AXIAL MAP (IN DIOPTERS), THE NUMERICAL VALUE OF THE CORRESPONDING AREA IN THE ELEVATION MAP (IN MICRONS) WILL ALWAYS SHOW A NEGATIVE NUMBER. |

FIG. 2b: THE SAME PATIENT AS IN FIG. 1 SHOWING CONTACT LENS WARPAGE OR PSEUDOKERATOCONUS. NOTE THE NEGATIVE VALUE (-10.9 MICRONS) IN THE ELEVATION MAP WHERE THE CROSS IS LOCATED. |

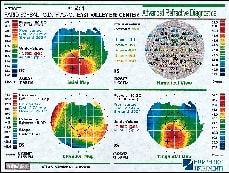
FIG. 2c: THE SAME EYE OF THE PATIENT IN FIG. 2b ONE WEEK AFTER DISCONTINUING CONTACT LENS WEAR. THE SAME POINT ON THE ELEVATION MAP NOW SHOWS A LOWER NEGATIVE VALUE (-4.4 MICRONS), AND THE AXIAL MAP SHOWS A 2.30D FLATTENING IN CURVATURE. |
PROPOSED METHOD OF DIFFERENTIATION
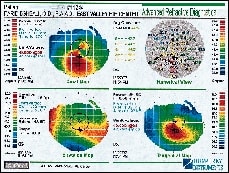
Historically, most clinicians use videokeratography to see the curvature of a patient's cornea, thus determining the flatness or the steepness of each point on the cornea. The inferior portion of a keratoconus suspect cornea and a contact lens induced warped cornea look very similar in curvature. They are both steeper than the adjacent point, resulting in a higher dioptric value which is displayed in warmer (i.e., orange, red) topographic colors (Compare Figs. 2a through 3d).
Humphrey Instruments' Atlas corneal topography system creates an elevation map by matching a best fit sphere to the cornea and identifying the points on the cornea that are higher or lower than this best fit sphere. The positive values (warmer colors) represent points on the cornea that are elevated, or higher than the best fit sphere; negative values (cooler colors) represent points on the cornea that are depressed, or lower than the best fit sphere. The following procedure will reveal whether the inferior steepening area seen on the axial map contains a point that has an elevated value (keratoconic contour) in comparison to its adjacent areas.
|
|
| FIGS. 3a & 3b: (3a) AN ISLAND OF POSITIVE VALUE (+11.9 MICRONS) IN THE ELEVATION MAP OF A KERATOCONUS PATIENT. (3b) THIS IS THE SAME EYE OF THE SAME PATIENT SHOWING AN ADJACENT POINT ON THE ELEVATION MAP WHICH HAS A NEGATIVE (DEPRESSED) VALUE (-19.2 MICRONS). | |
|
|
| FIGS. 3c & 3d: (3c) KERATOCONUS PATIENT'S EYE SHOWING AN AREA OF POSITIVE VALUE (+15.0 MICRONS) SURROUNDED BY (3d) AREAS OF NEGATIVE NUMBERS (-17.2 MICRONS). | |
PROCEDURE
Begin by moving the mouse cursor around in the steepened area of the axial map. Then look at the numerical value shown in the corresponding area of the elevation map for either of the following possibilities:
a) Pseudokeratoconus: The numerical value (in microns) in the elevation map corresponding to the steepened area of the axial map (in diopters) will always show negative numbers or depressed areas (Figs. 2a, 2b & 2c).
b) Keratoconus: The numerical value in the elevation map (in microns) corresponding to the steepened area of the axial map (in diopters) will show an island of positive values surrounded by areas of negative numbers (Figs. 3a, 3b, 3c & 3d).
*Note: Lid attachment rigid contact lenses sometimes produce an elevated inferior portion, and only after discontinuing lens wear and repeating topography can the differentiation between keratoconus and corneal warpage be made. CLS
References are available upon request. To receive them via fax, call (800) 239-4684 and request document #31.
Dr. Eghbali is a clinical instructor in ophthalmology at Jules Stein Eye Institute, UCLA School of Medicine, and in optometry at Southern California College of Optometry. He is also director of the contact lens department at Harbor-UCLA Medical Center and is in private practice in Burbank, Calif.



