RGPs for the Post-LASIK Patient: A Case Study
BY BUDDY RUSSELL, F.C.L.S.A.
OCT. 1997
RGPs and a little creativity restored functional vision to this presbyopic astigmat who experienced polyopia following laser in situ keratomileusis.
A 46-year-old engineer was referred to the Emory Contact Lens Service for management of monocular polyopia in each eye. He had undergone excimer laser in situ keratomileusis (LASIK) four months earlier to achieve a six-diopter spherical reduction of myopia. The ablation was performed within the central 6.0mm zone, following a 160 microns deep, 8.5mm diameter flap pass using the microkeratome. The patient felt that both his unaided and spectacle corrected visual acuities were inadequate to the extent that he could not return to work following the surgeries.
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||
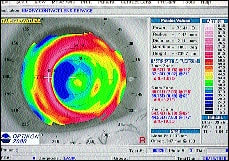
Postoperative manifest refraction provided only a marginal improvement over his unaided vision and did not eliminate the polyopia (Table 1). The patient was fitted with RGP lenses in attempt to neutralize the irregular corneal astigmatism (Fig. 1).
| ||||
Diagnostic lenses were used to determine the parameters necessary to achieve the best lens-to-cornea relationship. Spherocylindrical overrefraction revealed residual astigmatism, but lens flexure was not the cause. Without the cylindrical correction over the RGP lenses, the multiple images remained, but now were in focus and created greater distraction. However, with the spherocylindrical correction over the RGP lenses, the multiple images were eliminated. A spectacle correction with a progressive add was prescribed to correct the lenticular component and the presbyopia (Table 2). This RGP-spectacle combination provided the patient with 20/20 vision in each eye and eliminated the multiple images.
|
PREOP VERSUS POSTOP
The patient had lenticular astigmatism prior to surgery, so we could expect it to be present following surgery, unless the surgeon had added astigmatic correction to supplement the spherical correction. In this case, the procedure addressed the spherical equivalent of the optical system only. It seemed that the irregular corneal astigmatism was the reason the patient experienced monocular polyopia. By neutralizing the irregular corneal astigmatism with RGP lenses, the multiple images were easier to distinguish. The lenses provided a new anterior surface and yielded what the surgery did not. The residual refractive error, presumably the lenticular component, was interpreted by the patient as polyopia. If the patient's surgical outcome using spherical equivalents had resulted in plano postoperatively, would he complain of monocular polyopia?
TOPOGRAPHY ANALYSIS
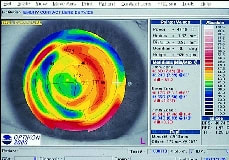
The temporal paracentral elbow (shoulder) is steeper in these corneas (Fig. 2). We see this via videokeratoscopy and fluorescein evaluation with an RGP lens on the eye. The temporal quadrant is the entrance wound site made by the microkeratome. The nasal quadrant may show less steepening as a result of the corneal hinge remaining intact.
|
|
| FIG. 2: STEEPENING IN THE TEMPORAL QUADRANT OF A POST-LASIK CORNEA. | |
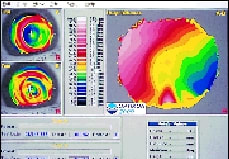
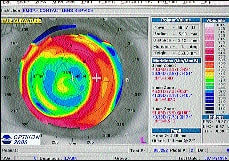
A height differential map (Fig. 3) enables us to analyze the effect of an RGP lens on the corneal surface. The map in the lower left was taken after full-time (16 hours/day) RGP lens wear for nine months without discomfort or vision problems. The map in the upper left was taken after the lenses had been discontinued for two weeks to allow corneal surgeons to evaluate and consider further surgery. The larger map on the right represents the elevation change in microns between the two maps. The temporal elbow rebounded steeper after the contact lenses were discontinued. Notice that there were essentially no elevation changes over the pupil area.
FIG. 3: HEIGHT DIFFERENTIAL MAP SHOWING CHANGE BETWEEN TOPOGRAPHY TAKEN IMMEDIATELY AFTER CONTACT LENS REMOVAL AND THAT TAKEN TWO WEEKS AFTER DISCONTINUING CONTACT LENS WEAR. |
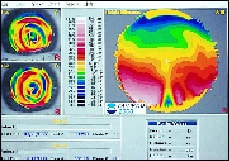
These corneas seem to be quite malleable. The map in the lower left of Figure 4 shows the baseline topography. The map in the upper left shows the topography the day the contact lens was removed after nine months of wear. Attaching the lens to the upper lid provided a comfortable, well-positioned lens. This resulted in the power of the superior cornea being pushed inferiorly. The symmetrical pattern demonstrates how well the lens centered. Does the preoperative eccentricity of the cornea play a role in this effect? Are these corneas softer? What would be the effect on the cornea if the lens were fit flatter? Steeper? Smaller? Reverse-curve? Research is in progress to answer these and other questions.
FIG. 4: HEIGHT DIFFERENTIAL MAP SHOWING CHANGE BETWEEN BASELINE TOPOGRAPHY AND TOPOGRAPHY TAKEN IMMEDIATELY AFTER CONTACT LENS REMOVAL. |
GAIN INSIGHT WITH A PREOP DEMONSTRATION
Part of the process of fitting contact lenses involves demonstrating the vision the patient can expect with contact lenses compared to spectacles. This helps the practitioner and the patient determine which lens design will provide optimum vision. Some patients can cope with soft or RGP lenses that leave small amounts of astigmatism uncorrected, while other patients cannot. The ability to accept less-than-perfect vision depends upon the individual's visual demands. Would this patient have reported monocular polyopia with the preoperative demonstration of only spherical spectacle correction? A pre-fit/presurgical demonstration determines which patients are sensitive to these small visual anomalies.
Contact lenses, including soft lenses, can be worn following LASIK. However, soft contact lenses won't neutralize irregular corneal astigmatism. RGP lenses not only neutralize irregular corneal astigmatism, but provide higher oxygen transmissibility. High Dk materials will minimize any additional inflammatory response.
Refractive surgeons continue to offer improved procedures and techniques
to their patients. For example, the newest generation Nidex laser is capable
of correcting spherical and astigmatic refractive errors in any meridian.
The public seems to be aware of the surgeon's increased armamentarium. Contact
lenses remain the most reversible, adjustable and accurate vision correction
modality available. CLS