contact lens case reports
Check the Topography Following Corneal Trauma
BY PATRICK CAROLINE, COT, & ROBERT CAMPBELL, MD
FEBRUARY 1998
Contact lenses are often required to correct the astigmatism or anisometropia resulting from a corneal laceration. A thorough understanding of the altered corneal topography is essential in determining whether a rigid, soft or combination lens deciding whether a rigid, soft or combination design is indicated.
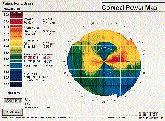
This month's case involves a 41-year-old man who suffered a perforating corneal laceration to his left eye from an iron projectile. The injury was surgically repaired with three interrupted 10-0 sutures. Postoperatively, the patient was left with a curved linear scar from 1:00 to 3:00 and a small traumatic iridectomy at 2:00 (Fig. 1). The uncorrected visual acuity of the right eye was 20/20. The left eye was 20/200. Manifest refraction of the left eye was +2.00 -5.50x97 with a visual acuity of 20/25. Corneal mapping of the left eye revealed simulated K readings of 47.50@ 004 / 41.87@ 094; or 5.62D of against-the-rule astigmatism (Fig. 2).
FIG. 1: Photokeratoscopy showing high, central against-the-rule astigmatism OS |
FIG. 2: Corneal map of patient's left eye |
Topographic Effects of Sutures
Unsutured incisions flatten the entire cornea due to wound gape and the subsequent addition of scar tissue. Sutured incisions, both radial and circumferential, flatten the cornea under the suture but steepen the cornea closer to the visual axis. Suture placement causes both localized and remote corneal topographic shifts, which must be considered when choosing the contact lens design. In this case, the patient's central keratometric reading indicated 5.62D of regular against-the-rule astigmatism. This might indicate that the patient is an excellent candidate for a toric RGP lens, but the corneal map provided a more complete picture.
All rigid contact lenses, regardless of their design, bear on the cornea about three or four millimeters from the center. Our patient's topography showed that midperipherally, the cornea was 44.75D superiorly and 45.50D temporally, indicating only 0.75D of midperipheral corneal astigmatism (Fig. 3). A back toric or bitoric RGP lens designed from the central keratometric reading would be grossly inappropriate for the midperipheral cornea, both horizontally and vertically.

FIG. 3: Midperipheral keratometric findings 4.0mm from center
We fit the patient with a Flexlens custom toric soft contact lens: 8.6mm base curve, +3.25 -6.00x97 power, 14.5mm diameter. Visual acuity was stable at 20/25 with a wearing time of 14 hours a day. This case illustrates the importance of photokeratoscopy and videokeratography following corneal trauma. The corneal changes induced by the injury and subsequent surgical repair greatly impact the lens that can be used postsurgically.
Patrick Caroline is an assistant professor of optometry at Pacific University and director of contact lens research at Oregon Health SCiences University. Dr. Campbell is medical director of the Park Nicollet Contact Lens Clinic & Research Center, Minnetonka, Minn.