Practicing Preventive Eye Care With UV-Blocking Eye Wear
With the right tools at your disposal, you can help your patients avert the link between exposure to ultraviolet radiation and the development of ocular and dermatologic conditions.
BY JAN P.G. BERGMANSON, OD, PHD, FC OPTOM, & TODD M. SHELDON, OD
FEBRUARY 1998
An increased life expectancy, a thinning ozone layer and greater participation in outdoor activities today has increased the incidence of ocular and dermatologic pathologies related to ultraviolet radiation (UVR). Although we see fewer patients with acute photokeratitis (Table 1) than those with signs of chronic UVR exposure, both types of ocular insult are on the rise. Therefore, we should be particularly alert for early chronic UVR damage in our patients and attempt to limit further insult.
|
UVR and the Ozone
The sun is the earth's primary source of UVR. It enters the atmosphere in the form of solar radiation. The location, altitude, sky cover, time of day and time of year all contribute to the amount of solar radiation reaching the earth's surface and, therefore, the eye. For instance, Atlanta, Georgia, and El Paso, Texas, are at approximately the same latitude, yet El Paso receives approximately 38 percent more UVR because it is at a higher altitude and in a drier region. Alaska receives approximately 10 times less UVR than Hawaii because Hawaii is closer to the equator.
UVR is located adjacent to but below visible light on the electromagnetic spectrum. It encompasses wavelengths between 100 and 400 nanometers. Long wavelength UVA exists at wavelengths between 315 and 400nm. UVB is the waveband between 280 and 315nm. UVC includes wavelengths from 200 to 280 nm. The wavelengths between 100 and 200nm are termed Vacuum UV or UVVacuum. UVC and UVVacuum are the most toxic UVR wavebands. Fortunately, the ozone in the stratosphere blocks the UVVacuum and UVC as solar radiation travels toward the earth's surface. (Fig. 1) However, the incidence of serious integumentary and ocular insult secondary to UVR has increased dramatically over the past few decades, and this is believed to be due at least in part to the temporary loss or thinning of the protective ozone shield in some regions of the world.
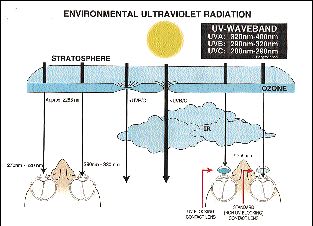
FIG. 1: Environmental UV radiation. The UV filter of the earth, the ozone,
blocks radiation of approximately 288nm or less. Clouds absorb infrared radiation, but
have little or no UV-filtering capability. The corneal action spectrum peaks in the
270-310nm waveband while that of the crystalline lens peaks in the 295-320nm waveband.
Less than one percent of the ambient UVR is believed to be incident on the retina. An
effective UV-blocking hydrogel lens would keep UVR out of the eye
The highest UV intensities on earth have been recorded at the Mauna Loa Observatory (MLO) in Hawaii, probably due to its location near the equator and at an altitude of 3,400 meters. Its unique location has also allowed the MLO to study the health of the earth's protective UV filter, the ozone. Holes in the ozone were confirmed in the 1980s, and a strong correlation between UV irradiance and the thickness of the ozone has been established. Although most of the extreme thinning and holes of the ozone have been recorded over Antarctica, the ozone dropped to below 200 Dobson units (DU), which is the unit for measuring the thickness of the ozone, over Hawaii in late December of 1994. The mean value for the month of December from 1964 through 1981 was 249 DU. The amount of UVR at 295nm reaching the earth's surface through this "ozone hole" tripled during this time.
Of further concern is the prediction that ozone depletion will continue at least until the year 2000. After this time, assuming all nations comply with the international rules laid out by the Montreal Protocol controlling atmospheric chlorine, there will be a very slow recovery as the ozone rebuilds, but it may not reach original levels until the year 2050. Expecting all nations, especially the underdeveloped countries, to strictly adhere to the Montreal Protocol may not be entirely realistic, though, due to large-scale CFC (Chlorofluorocarbon 12-CFC-12) contraband activities in India and other countries where CFC is still manufactured legally for internal use. In the United States, CFC cannot be legally manufactured, but heavily taxed CFC may be used for older cooling systems, such as those found in some automobiles. This tax burden has encouraged huge quantities of the toxic gas to be smuggled into the United States, making it second in magnitude only to the smuggling of illicit drugs. Assuming current levels of CFC production are maintained, it is estimated that there will be at least a six percent decrease in the ozone concentration over the next several decades. This would result in a huge rise in the incidence of UV-related ocular pathologies and skin cancer.
UVR and Tissue Changes
There's an abundance of evidence linking UVR and dermatologic pathologies. Although there's less evidence linking ocular pathology and UVR, recent studies indicate that UVR is harmful to the eye (Table 2).
|
Conjunctival Pathologies-- The conjunctiva has long been overlooked in UVR-related research, but a recent study showed that it is injured by UVR as easily as the cornea. There is also epidemiologic evidence for an association between the time spent outdoors and the prevalence of pterygium and perhaps pinguecula (Fig. 2). Another study found a weak association between UVA and the development of pinguecula in fishermen from the Chesapeake Bay in Maryland. The current evidence for a link between UVR and pterygium is stronger than the link between UVR and pinguecula.
.

FIG. 2: Pinguecula may be an early warning sign of excessive chronic UVR
exposure.
One study has offered a reasonable explanation for the formation and specific orientation of pterygia. It demonstrated that tangentially incident light at the temporal limbus travels across the anterior chamber and comes to a concentrated focus on the opposing corneal side near the nasal limbus. This unintended refracting power of the peripheral cornea may allow for an up to 20-fold concentration of scattered incident light or UVR, and may explain why pterygia are most common in the horizontal meridian on the nasal aspect of the cornea. However, it does not explain why pterygia are occasionally observed temporally. This same model may also provide an explanation for the appearance of some cortical cataracts, which is also supported in a ray tracing study.
Corneal Changes-- Although the damaged nerve endings in the corneal epithelium are the main source of the symptomology in photokeratitis, the stroma and the endothelium are also traumatized by UV exposure (Fig. 3).

FIG. 3: Acute photokeratitis following exposure to UVR (300nm, 0.225 j/cm2)
at an energy level found in high-intensity ambient environments. (left) Full thickness
epithelial trauma with only severely traumatized basal cells still remaining. As these
remaining and presumably nonvital cells desquamate, the cornea becomes denuded. (right)
Advanced endothelial and stromal edema. Fluid surrounds a keratocyte and numerous
endothelial bleb-like, edematous pockets are present. Both transmission
electron-micrographs (x3500 magnification) are from the same primate cornea, which was
harvested 24 hours after exposure.
There is considerable evidence that chronic UVR exposure leads to degenerative corneal changes known as climatic droplet keratopathy or spheroidal degeneration. Climatic droplet keratopathy may develop more rapidly than previously thought. A recent report showed a recurrence of the condition within three and a half years in two different cases after corneal transplantation. Another study found a relationship between ambient UVR and an increase in corneal endothelial polymegethism and pleomorphism when comparing a group of outdoor workers with a control group. Similarly, it was reported that a group of welders averaging 17 years of welding experience had developed more endothelial polymegethism than a control group of age-matched subjects who lacked a background in welding. Thus, artificial UV sources should not be overlooked as a potential hazard.
Cataracts-- The link between changes in the crystalline lens and UVR is widely accepted. Contrary to previous notions, the chronic effect of UVR on the crystalline lens is the formation of cortical cataracts, not brunescent nuclear cataracts (Fig. 4).

FIG. 4: Premature cortical cataractous changes may be an early warning sign
of excessive chronic UVR exposure.
The Beaver Dam Eye Study assessed the prevalence and severity of lenticular opacities in a rural community in the United States. It found that cortical and nuclear cataracts, but not posterior subcapsular cataracts, were more common in women. In Gothenburg, Sweden, all cataract extractions performed over a two-year period were recorded. It was determined that after the age of 70, the incidence of cataract was significantly higher in women than in men, and that the relative risk of developing cataracts severe enough to require cataract surgery was 1.71 (95% confidence interval 1.51-1.94) for women compared to men. The first eye cataract extraction on women over 70 years of age outnumbered those of the men by a factor of three. The Framingham Eye Study revealed a similar gender-linked trend, although the authors did not place significance on this finding. The study found that cataracts were more common in women than men for all age groups and this difference increased with age. The more recent Gothenburg study seems to confirm this finding.
The gender-linked difference in cataract formation may be of considerable importance and warrants further investigation. A possible explanation of the increased prevalence of cataracts in elderly women might be the change in lifestyle women have undergone in this century, which may increase their lifetime UVR dose.
Debated Retinal Effects-- Opacities of the crystalline lens, which reduce the transmission of light and UVR through the eye, become more prevalent with age. The cornea and crystalline lens of the eye filter the majority of UVR. Therefore, extremely small amounts of UVR reach the retina. Nonetheless, UVA has been shown to elicit a visual evoked potential response in the young human eye.
Controversy exists about whether UVR reaches the retina in sufficient quantities to cause acute or chronic trauma. One report indicated an association between age-related macular degeneration and outdoor leisure time, but the cause may have been ambient blue and visible light rather than UVR. An interesting finding of both the Beaver Dam Eye Study and Framingham Eye Study was that women over the age of 75 were more likely than men to develop age-related maculopathy.
Experimental studies on primates have demonstrated that high intensity light may cause temporary and, in some cases, permanent retinal damage. The aphakic eye lacks its natural UVR filter for the 300 to 400nm range and is therefore more easily traumatized by UVR in this waveband. Both animal and human studies demonstrate the retinal vulnerability to UVR. Therefore, after extraction of the crystalline lens, the need for ocular UVR protection becomes even more critical. This is why most intraocular lens implants have a built-in UV blocker.
Skin Cancer-- A link between solar radiation and skin cancer has long been suspected. In the late 1800s, it was noted that sailors chronically exposed to the sun developed "Seemannshaut" or "sailor's skin." In the early 1900s, a higher prevalence of skin cancer among farmers and among Caucasians was noted.
The effects of UVR on the skin -- erythema, blistering, exfoliation (sunburn), and eventual tanning -- have become increasingly obvious over the past several decades. Although humans can tolerate low doses of UVR, the cutaneous immune system responsible for this tolerance is traumatized in the process. It is thought that these immunogenetic factors also increase the risk for UVR-related skin cancer.
The effects of chronic UVB exposure tend to be cumulative. This means that the increasing life expectancy also increases the risk for skin cancer. The types of skin cancer linked to chronic UVB exposure are basal cell and squamous cell carcinomas. Non-melanoma skin cancer, primarily basal cell carcinoma, accounts for 90 percent of adnexal cancers, and the number of basal cell carcinomas reported annually in the United States is rising rapidly. Between the years of 1983 and 1994 there was a 50 to 100 percent increase in the number of basal cell carcinomas reported in the United States.
Skin melanoma represents only about five percent of all skin cancers but is responsible for approximately 75 percent of all skin cancer deaths. The incidence of malignant melanoma is also increasing rapidly. In the 30 years between 1961 and 1991, the lifetime risk of developing a malignant melanoma increased by 600 percent and is still on the rise. These highly malignant and deadly cutaneous melanomas seem to be more related to acute high intensity exposure, such as intense sunburns and/or exposure to excessive sunlight at a young age, than to chronic UVB exposure over a lifetime.
Some people are more at risk for developing skin cancers than others. Lightly pigmented individuals and those utilizing photosensitizing chemicals and medications are more susceptible to the harmful effects of UVR (Table 3).
|
*Source: Pharmacology and Nursing. 17th Edition, McKenry and Salerno, 1989
Protective options
There are many ways to protect the eyes from UVR (Table 4).
|
UV Blocking Contact Lenses-- The majority of contact lenses marketed today are transparent to UVR. Fortunately, some hydrogel and RGP contact lens manufacturers are adding UV blockers to their materials. It's useful to evaluate the transmission curves for the various UV-filtering materials because all lenses do not absorb the UV waveband equally well.
According to Class II of the American National Standards Institute (ANSI), a contact lens must absorb a minimum of 95 percent of UVB and 70 percent of UVA to be classified as UV-blocking. Since the UV-blocking component of these contact lenses is integrated into the material, the percentage of UVR absorbed or transmitted through the lens is a function of the thickness of that lens. Therefore, the contact lens with the least average thickness of a particular brand is used to ascertain whether or not that brand of contact lens meets the ANSI standard. The ANSI standard further dictates that the entire contact lens, not just particular regions, must block UVR.
Most RGP lenses have an overall diameter less than the diameter of the cornea. Therefore, RGP lenses with a UV-blocker offer less protection than hydrogel lenses. For instance, if a UVR-filtering RGP that is 9.0mm in overall diameter is fit on a 11.5mm cornea, only 60 percent of the cornea receives UV protection at any given time, and the critical stem cells at the limbus receive little or none of this protection. Although the UV-filtering RGP is not 100 percent effective and has a less-than-perfect UVR absorption curve, it is better than fitting a contact lens that doesn't contain a UVR filter.
Hydrogel lenses, on the other hand, are designed to overlap onto the limbus, so a well-fitted, UVR-blocking hydrogel lens protects the entire cornea as well as the internal structures of the eye. It also gives vital protection to the epithelial stem cells located in the limbus and palisades of Vogt.
The corneal epithelium is a dynamic layer. It requires a steady influx of epithelial cells from the limbus and the conjunctival palisades of Vogt to maintain normal epithelial thickness and health. This concept is known as the XYZ theory. The epithelium, including the stem cells, is the corneal layer most sensitive to UV-induced trauma. Therefore, a lens that shields the vital conjunctival and limbal regions is beneficial.
Spectacle Lens Options
Spectacle lenses can be prescribed with an effective UV-filtering coating. However, the spectacle lens doesn't offer a complete protection of the eye and its internal structures since obliquely incident UVR still reaches the eye, either directly or by reflection off of the back surface of the spectacle lens.
Without a UVR-blocking coating, the CR-39 common plastic lens filters UVR less than 350nm but still transmits a portion of the UVA. Crown glass begins transmitting radiant energy at 290nm, and therefore doesn't block UVR reaching the earth's surface. UV-filtering coatings are inexpensive and can be added to both glass and plastic lenses. These coatings begin transmitting radiant energy at approximately 400nm. Interestingly, there's no official standard on what radiation clear ophthalmic lenses must filter to carry UV-blocking labeling.
Polycarbonate lenses are gaining wider popularity among practitioners and patients due to their favorable impact-resistant properties. Polycarbonate is a unique material that filters radiant energy below 380nm. Thus, clear polycarbonate spectacle lenses block the majority of UVR radiation.
Sunglasses
For outdoor enthusiasts, sunglasses or tinted spectacle lenses may provide superior comfort and UVR-blocking capabilities to clear spectacle lenses in bright environments. This may explain in part the ballooning of the sunglass industry over the past few decades. In 1988, the non-prescription sunglass industry sold over $1.3 billion in products.
The FDA recommends that all sunglasses, prescription and non-prescription alike, block 99 percent of UVB and 95 percent of the UVA. Most of the sunglasses available on the market today meet this criteria.
The ideal choice of sunglasses for UVR protection is not necessarily the most
fashionable choice. Today's popular sunglasses typically have dainty metal frames with a
small eye size. These trendy models with small eye sizes may not offer protection against
direct, reflected or scattered UVR that enters the eye obliquely. Hydrogel contact lenses
which
adequately block UVR may protect the eye against the effects of such radiation. The
aviator and newer wrap-around styles of sunglasses offer much better protection from UVR
than their smaller eye size counterparts. The wrap-around style sunglasses popular among
sports enthusiasts filter out the direct as well as the obliquely incident UVR.
Additional Options
UV-filtering contact lenses, sunglasses and ophthalmic lenses offer the best ocular
protection against UVR, but other devices used in conjunction can enhance protection.
These secondary options include wearing wide-brimmed hats or baseball caps, applying
sunscreen lotion greater than SPF
15 and avoiding outdoor activities in UV-intense environments between the hours of 10 a.m.
and 2 p.m. The earth receives 80 percent of its daily UVR dose between these hours, and
direct UVR exposures during this time period have been shown to induce a keratitis in only
30 minutes in some regions. UVR-intense environments are found at both high and low
altitudes and latitudes. At high altitudes, the combination of reduced atmospheric UV
filtering and the high reflectance of snow produces acute UV responses in a relatively
short time frame while also adding a large UV dose to the lifetime exposure. At lower
altitudes, time spent at the beach, tennis courts, etc., can effectively produce the same
traumatic effect.
Unfortunately, peak hours for outdoor activities are also peak hours for UVR reaching the earth, and the number of people enjoying outdoor recreation has been increasing steadily. In Vail, Colorado, the number of skiers has increased by 60 percent over the past 15 years. Protection from the UVR is particularly important while snow skiing because snow has the highest UVR reflectance of a natural surface. Water, wet sand, boat docks, tennis courts and concrete roadways also reflect a significant amount of UVR.
Conclusion
The majority of UVR-induced ocular trauma is preventable. Our role, therefore, should be to educate patients on the hazards of UVR exposure. In addition, we should offer them prevention options in the form of contact lenses, spectacles and sunglasses.
Dr. Bergmanson is a professor of optometry and director of the Laser Laboratory, the Anatomy and Pathology Laboratory and the Eye Research Clinic at the University of Houston College of Optometry. He is also a Foundation Fellow of the College of Optometry in the United Kingdom, a fellow of the AAO and a diplomate in the Cornea and Contact Lens Section of the AAO.
Dr. Sheldon, valedictorian of his 1997 graduating class at the University of Houston College of Optometry, is a staff optometrist at the Beaufort Naval Hospital, South Carolina.
Special thanks to Dr. Russ Schnell of the Mauna Loa Observatory for generously providing pertinent information, to Mrs. Yvonne Blocker for preparing micrographs, and to Mr. Curg Click and Patrick Ladage for graphics support.
References and reprints are available from: Paul White, O.D., New England College of Optometry, 424 Beacon St.,



