Corneal Topography
An Important Clinical Tool
BY LOUIS A. FRANK, OD, FAAO, & WILLIAM PRENTISS, OD
MARCH 1998
Seeing the improvements in patient satisfaction, revenue and diagnostic ability, these practitioners know that purchasing a corneal topographer was the right decision.
One of our colleagues recently remarked that "The corneal topography market is dead." In the next breath, however, he stated that his topography unit generates $1,800 per month profit for his practice. Practitioners do not appear to appreciate the clinical importance of corneal topography or of the revenue potential in the primary care practice.
Whether or not new technology is meaningful depends on criteria such as:
- Does the incorporation of new technology allow you to enhance your diagnostic capabilities, further ensuring that you gain meaningful information about the health and welfare of your patients?
- Is the new technology available at a cost that is affordable for your office as well as for your patients?
- Are practitioners who advocate purchasing the new technology representative of you and the size, location and overall characteristics of your practice? In other words, are the corneal topography proponents in the trenches with you, dealing day-to-day with the pressures of reduced reimbursement for eyecare services and the need to find ways to control practice costs?
- Will the benefit of the technology convince your patients to accept the increased professional fees required to cover the cost of incorporating it into your practice?
Clinical Scenarios
We leased a corneal topography unit for our practice (Table 1) about two years ago in anticipation of the predicted volcanic explosion of the PRK industry. We currently use the unit for this purpose three or four times per year. We've found the value in corneal topography to exist outside of refractive surgery, recognizing that the application of this technology will become even more valuable when laser vision correction comes of age.
We perform corneal topography as a standard clinical test in a variety of scenarios including the following:
During a new contact lens evaluation to screen for irregular corneal toricity and to serve as a baseline to evaluate the long-term corneal response to contact lens wear. Figure 1 shows the corneal maps of a patient, A.S., who was previously diagnosed at another facility with keratoconus. A.S., who suffered for years with the anxiety of having a potentially progressive ocular disorder, actually had a refractive amblyopia secondary to significant against-the-rule astigmatism.
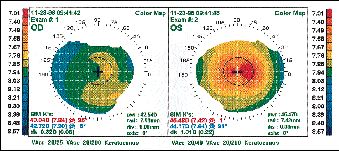
FIG. 1: A.S., 53-year-old woman previously diagnosed with keratoconus.
Topography confirms diagnosis of bilateral refractive amblyopia secondary to
against-the-rule astigmatism.
During each annual contact lens examination to determine stability of corneal curvature in response to contact lens wear, and to rule out lens-to-cornea relationship problems that may manifest in patient complaints. Figure 2 includes maps of an extended wear hydrogel lens patient complaining of reduced vision. In the top two maps, note the visual acuities with refraction and the corneal maps which show possible steepening of corneal curvature secondary to corneal edema, particularly in the left eye. In the bottom two maps, note the reduced steepening of the left corneal map and the results of the refraction on the second visit, after discontinuation of contact lens wear.
|
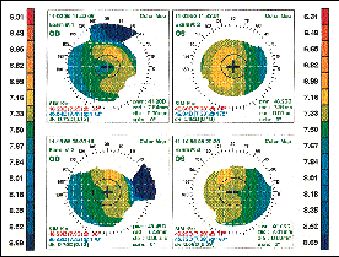
FIG 2: (top) J.H., 28-year-old man with edema from extended wear contact
lens overwear. (bottom) J.H., corneal map taken two weeks after discontinuation of lens
wear.
In any instance when a primary care patient's vision is not correctable to 20/20 or thereabouts in order to rule out irregular corneal toricity and particularly to rule out keratoconus. Figure 3 illustrates how only corneal topography identified this keratoconus case which appeared normal in all respects: K readings, refraction, visual acuities and absence of patient complaints. All of the corneal activity was below the visual axis.
In low vision examinations to rule out or to confirm a corneal toricity component to the reduced vision, i.e., uncorrected or undercorrected significant astigmatic refractive errors or in cases where no retinoscopic reflex is observed during the examination. Figure 4 shows a 16-year-old girl with tyrosinase negative albinism. Pendular nystagmus makes examination difficult in these cases, and the corneal map confirms the often observed presence of significant uncorrected corneal astigmatism. This then allows the practitioner to consider both spectacle and contact lens options for the patient. While the corneal map in this case is less precise than usual, it indeed serves as a gross screening tool.

FIG. 3: S.C., 43-year-old man. Note the bilateral inferior keratoconus maps
which spare the visual axis in this asymptomatic patient
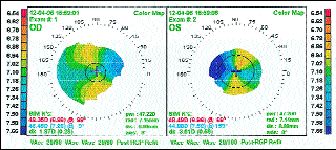
FIG. 4: A.B., 16-year-old girl with tyrosinase negative albinism and
nystagmus. Note the confirmation of potential corneal toricity.
Responsibilities To Your Patients
The use of corneal topography in the practice is an added expense to the patient, regardless of which vision care program the patient is enrolled in. Eyecare practitioners, especially optometrists, must accept the responsibility of ordering tests which are necessary and in the best interests of their patients. Most patients will understand your recommendation if you explain it to them. Leaving this duty to your staff or your receptionist is asking for misunderstanding and a misrepresentation of your fees. The idea of handing the patient a pre-printed form explaining the corneal topography procedure and asking him to sign in acceptance of the increased fee seems like your office is making excuses for the testing and suggesting that the testing is arbitrary.
An Evolving Technology
On a more global level, corneal topography is evolving in terms of its utility for the novice contact lens fitter or for the practitioner who still fits contact lenses empirically. Insufficient expertise in fluorescein pattern interpretation, insufficient information concerning the topography of the periphery of the cornea and incomplete understanding of peripheral curve contact lens design ultimately result in increased costs to practitioners in contact lens fitting adjustments and increased chair time. Several of the currently available corneal topography units have software programs that enable you to select initial contact lens prescriptions after the instrument has recommended a contact lens option and you have viewed and adjusted the fluorescein patterns.
There's no doubt that the cost of corneal topographers must be affordable to all varieties of practitioners. This is challenged by the need to maintain or even improve instrument capabilities. In other words, manufacturers must not strip their systems of important features in order to accommodate price. Give us a comprehensive corneal topography system at a reasonable price!
One thing is for certain -- our corneal topographer has paid for itself from almost day one and has done so without refractive surgery, which will only further enhance the value of this technology in our practice and in yours.





