A Closer Look at Ocular Allergy
Carla J. Mack, O.D.
April 1999
Treating the itchy-burnies requires proper diagnosis.
Ocular allergies are among the most common external eye diseases that the contact lens practitioner diagnoses. Before effective hygienic or pharmacologic management of allergy is instituted, the mechanisms of the allergic response must be understood. The eyelids, conjunctiva, corneal limbus and precorneal tear film are the structures that house the mediators involved in producing the ocular immune response. The allergic reaction is responsible for a number of common ocular disease processes, such as seasonal and perennial allergies, and giant papillary conjunctivitis (GPC). Itching, conjunctival injection and chemosis, tearing and mucous discharge, papillary reaction, burning, lid edema and erythema may all present with the classic ocular allergy.
The Allergic Response
Acquired immunity begins with the production of B and T lymphocytes in the bone marrow. The B cell matures in the bone marrow and is responsible for humoral immunity. After encountering a specific antigen in the blood or lymphatic vessels, the B cell produces plasma cells that make millions of antigen-specific soluble antibodies.
Once the T cell has matured in the thymus, it contributes to cellular immunity by directly killing infected body cells and by producing lymphokines that damage tissue, attract other immune cells and help to regulate the immune response.
The allergic reaction begins with the primary exposure of an allergen, which causes B cells to produce allergen-specific IgE antibodies, which attach to circulating mast cells or basophils. There are approximately 50 million mast cells in each human eye, with tens of thousands of IgE antibodies on the outer cell membrane of each sensitized mast cell. With subsequent exposure and binding of the specific allergen to the arms of two adjacent IgE antibodies, the cell membrane permeability changes, releasing preformed mediators and an allergic reaction results within seconds. The mediators found in ocular allergic disease are histamine, platelet-activating factor and eosinophil chemotactic factors. Histamine produces itching, vasodilation and edema. Elevated levels of major basic protein released by eosinophils causes further degranulation of mast cells and is associated with vernal keratoconjunctivitis (VKC), as well as GPC.
Increased levels of intercellular calcium ions, associated with mast cell degranulation, stimulate the inflammatory cascade with the production of phospholipase A2 and the conversion of arachidonic acid. Subsequently, the influx of eosinophils, neutrophils, basophils, lymphocytes and macrophages causes a prolonged, more damaging reaction (Fig. 1). Type I anaphylactic and Type IV cell-mediated, or delayed hypersensitivity reactions, are responsible for ocular allergic disease. Seasonal and perennial allergic reactions are examples of the Type I response, which occur when an allergen attaches to a mast cell or basophil with membrane-bound IgE and causes degranulation. Drug hypersensitivity, VKC and GPC display components of the delayed Type IV reaction, where sensitized T cells release tissue-damaging lymphokines.
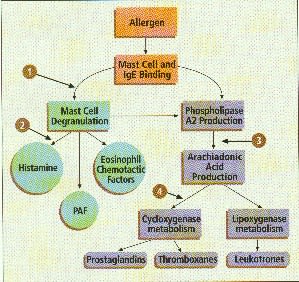
FIG 1: The Allergic Cascade - 1) Mast cell stabilizer, 2)
Antihistamine, 3) Steroidal anti-inflammatory agent and 4) Nonsteroidal anti-inflammatory
agent
Pharmacologic Intervention
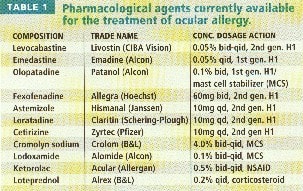
When treating ocular allergies, both pharmacologic (Table 1) and non-pharmacologic management strategies need to be considered, depending on the severity of the symptoms. The first, although often not the simplest approach for treatment, is avoidance or removal of the allergen. If this isn't possible, nonprescription therapy, such as cool compresses and artificial tears, are recommended for mild symptoms. Eye rubbing can cause mechanical activation of mast cells and should be discouraged.
Similason's Eye Drops #2 is an over-the-counter homeopathic formulation recommended for the relief of symptoms caused by seasonal and perennial allergens. It has no contraindications or reported adverse reactions and may be used in conjunction with contact lens wear.
Ocular decongestants stimulate alpha 2 receptors on blood vessels, counteracting the vasodilation effects caused by preformed mediators. They have limited use because of their local and systemic side effects, but occasional use is safe.
Phenylephrine-containing compounds have been replaced by the imidazole derivatives, which don't cause rebound vasodilation or contact lens discoloration with chronic use. Concurrent use with contact lenses should be avoided, as the vasoconstriction can mask contact lens induced conjunctival injection.
Topically or orally administered antihistamines work by blocking histamine from one of the three receptor sites (H1, H2 and H3), which have been identified in ocular tissue. Anticholinergic side effects, such as sedation, dry eyes and decreased accommodation are common with the first generation H1-specific antihistamines because of their high lipid solubility. When used chronically, topical H1 antihistamines may also produce a secondary hypersensitivity reaction in susceptible individuals.
Several topical antihistamines are currently available. Pheniramine and antazoline are first-generation H1 blockers available over-the-counter and only in combination with a decongestant. Emedastine is the newest H1 topical antihistamine with FDA approval. Olopatadine hydrochloride is another H1 antagonist with the added property of mast cell stabilization. Levocabastine is the only second-generation H1 antihistamine available.
Despite their anticholinergic side effects, first generation oral H1 antagonists are widely used because they are available over the counter, they provide relief and are relatively inexpensive. The oral non-sedating second-generation H1 antihistamines exhibit some mast cell stabilization properties in addition to blocking H1 receptors. Terfenadine, which was linked to serious drug interactions, was recently taken off of the market and replaced with it's safer metabolic derivative, fexofenadine. Astemizole, loratadine and cetirizine are all second-generation oral H1 blockers available with once-a-day dosage.
Topical mast cell stabilizers, such as cromolyn sodium and lodoxamide tromethamine, prevent the degranulation and subsequent release of preformed mediators from sensitized mast cells, thus inhibiting the Type I hypersensitivity response. These drugs have no affect on any histamine already in circulation, so their full therapeutic potential is often not seen for up to a week. They may be used chronically, as long as their action is contributing to symptomatic relief. Currently, mast cell stabilizers are approved for the treatment of vernal keratitis, vernal conjunctivitis and VKC, although they're widely used to treat GPC and chronic allergic conjunctivitis. Studies have indicated that cromolyn sodium does not accumulate in soft lenses, but neither cromolyn sodium or lodoxamide tromethamine are currently FDA-approved for use with lens wear. Many patients may benefit from the short-term use of these drugs concurrently with disposable contact lenses, but their use must be advised as off-label.
Ketorolac tromethamine is a topical nonsteroidal anti-inflammatory drug (NSAID), which affects the inflammatory cascade of the allergic response by inhibiting cyclooxygenase and diminishing the production of prostaglandin E2 in the aqueous humor, which is chemotactic for other inflammatory mediators. It is currently the only approved NSAID to treat ocular itching associated with seasonal allergic conjunctivitis. Stinging can be minimized by refrigerating it before instillation.
Corticosteroids also affect the inflammatory pathway of the allergic response by inhibiting phospholipase A2, and thereby the production of prostaglandins, thromboxane and leukotrienes. Topical corticosteroids have been used to rapidly decrease the signs and symptoms of moderate to severe allergic conjunctivitis on a short-term basis. Loteprednol etabonate 0.2% is the first topical corticosteroid specifically approved for treating ocular allergy. Because it is rapidly changed to an inactive metabolite after entering the target tissue and contributing therapeutically, the risk of unwanted side effects is decreased. Oral corticosteroids are rarely needed for ocular allergic disease except in the most severe reactions.
Any solution that comes in contact with the ocular surface, whether it is a contact lens solution or pharmacologic agent, has the ability to produce a delayed hypersensitivity reaction. Preservatives such as thimerosal and chlorhexidine have been the most recognized allergens. Hypersensitivity reactions to contact lens solutions containing thimerosal were once common, but are now almost obsolete due to the many thimerosal-free products available. Thimerosal is known to cause conjunctival injection, corneal edema and limbal infiltrates. It is also associated with contact lens induced superior limbic keratoconjunctivitis (SLK), which must be differentiated from SLK of Theodore. Both present with superior conjunctival injection, superior corneal punctate staining and superior corneal vascularization. Theodore's SLK is associated with thyroid disease, is typically found in middle-aged women and often improves with soft contact lens wear.
Benzalkonium chloride is not used in contact lens solutions but is common to many topical ocular medications. Unlike RGPs, soft lenses can absorb benzalkonium chloride, which produces a red, painful eye with diffuse corneal superficial punctate keratitis. This rapid toxic effect is seen when a soft lens has been rinsed and soaked in the solution. The concentration of a single drop of medication containing benzalkonium chloride as a preservative onto a soft lens is not significant enough to produce the ill effect. Although not approved by the FDA, it has been my experience that some topical ocular medications containing benzalkonium chloride may be safely used for short durations with soft contact lenses.
Clinical Presentations
Acute atopic conjunctivitis is a Type I hypersensitivity reaction to allergens such as pollens and mold spores. The most notable symptom is itching, accompanied by tearing and complaints of pressure behind the eyes. The external ocular exam shows eyelid edema, conjunctival injection and chemosis, and papillae. Some eosinophils may be found from conjunctival scraping, but numerous eosinophils are more indicative of VKC. Mild symptoms may be relieved by non-pharmacologic means, while a number of therapeutic paths exist for moderate to severe symptoms. I generally prescribe a topical antihistamine for one week to work on the acute symptoms as well as a mast cell stabilizer to provide chronic relief for as long as the offending allergen is present. Severe signs and symptoms may respond quicker to a topical steroid of moderate strength. Second generation oral H1 antihistamines will also benefit patients with systemic symptoms like allergic rhinitis. For those who present with a history of seasonal allergies, I like to begin a topical mast cell stabilizer prophylactically several weeks before the beginning of the allergic season.
Chronic atopic keratoconjunctivitis often occurs in adults with a history of systemic atopy. Perennial-type allergens, like animal dander and dust mites, can give rise to a chronic atopic conjunctivitis. A type IV cell mediated response is partially responsible, although the pathogenic factors are not known. Patients present with intense itching and no seasonal preference and have vision-threatening signs like conjunctival scarring, corneal neovascularization and anterior subcapsular cataracts. Treatment should consist of pulsed doses of topical corticosteroids to decrease corneal inflammation and provide symptomatic relief with the addition of a topical mast cell stabilizer for maintenance therapy.
Vernal keratoconjunctivitis is a combination of the Type I and Type IV hypersensitivity responses exhibiting increased tear IgE and numerous eosinophils on conjunctival scraping. It is a self-limited bilateral disease more common in young males with a history of atopy. Intense itching begins in the spring accompanied by a ropy mucous discharge and giant cobblestone papillae on the superior tarsus. Horner trantas dots appear at the corneal limbus and are pathognomonic for VKC. These white deposits are an accumulation of eosinophils found at the corneal limbus. Cold compresses or a topical NSAID may reduce itching, but I have found that short doses of a topical steroid may better alleviate symptoms. These patients must be placed on a topical mast cell stabilizer for maintenance therapy.
Giant papillary conjunctivitis is characterized by newly-formed large papillae that displace normal papillae, hyperemia, mucus secretions, itching and contact lens intolerance. Suspected triggers for GPC include contact lens induced mechanical trauma to the upper eyelid and antigens on the surface of contact lenses. Both the Type I and Type IV hypersensitivity responses play an immunologic role that is not clearly understood. Treatments include: improving contact lens hygiene and altering the contact lens design, using a deposit-resistant material and recommending a shorter wearing schedule. Pharmacologic management is best obtained with a mast cell stabilizer with or without continued lens wear, depending on the severity of the symptoms.
Microbial allergies occur when bacteria produce exotoxins, causing a type I hypersensitivity response with symptoms of itching, tearing and burning. The lid margin will show signs of blepharitis including hyperemia, telangietic blood vessels and scales at the base of the eyelashes. A slit lamp examination may reveal catarrhal corneal infiltrates commonly found at the 10, two, four and eight o'clock positions where the lid margin comes in contact with the limbus. A characteristic clear zone exists between the infiltrate and limbal blood vessels, suggesting removal of the offending antigen by the blood vessels. Treatment requires improved lid hygiene, as well as an antibiotic ointment applied to the lid margin. Although the marginal infiltrates will dissipate on their own, topical corticosteroid drops applied several times a day for three or four days will speed the healing process.
An immunologic response that is normally protective can be responsible for considerable tissue damage and patient discomfort. It's our responsibility to understand the pathophysiology of a presenting disorder, as well as the pharmacology of the newest medications, so that the best therapeutic program can be instituted.
To receive references via fax, call (800) 239-4684 and request document #47.




