ALLERGY
Allergy, Eyedrops and Contact Lenses
By Arthur B. Epstein, OD, FAAO
April 2001
Better manage seasonal allergic conjunctivitis by learning the mechan-isms behind it and which medications best treat the disease.
Spring is in the air, and allergy season is warming up. While this may be bad news for allergy sufferers, a strong allergy season is usually a busy time for eyecare practitioners. Unlike the respiratory system, the eyes lack protective filters, leaving them in direct contact with potential allergens. Consequently, eyecare practitioners are often the first healthcare providers to be consulted about allergy.
Thanks to an abundance of recent research and improved medications, practitioners are better able to manage patients' allergic complaints. This is especially true in the contact lens wearer, where in the past ocular allergy often interfered and sometimes totally precluded contact lens wear.
Atopy and Allergy
Although sometimes used interchangeably, atopy and allergy mean different things. Atopy refers to a genetic predisposition to respond with an unusual and heightened immune response to a normal environmental substance such as dust, plant pollens, or animal dander. An individual may be atopic but will not necessarily manifest allergy. The word "atopy" derives from the Greek a topos, meaning out of place or out of the ordinary. Atopy generally refers to classic allergic conditions such as allergic rhinitis, asthma and atopic dermatitis.
For most individuals, exposure to the many potential allergens in our environment produces no effect. However, for the approximately 50 million Americans the 20 percent of the U.S. population that suffers from seasonal or perennial allergies even brief re-exposure to an allergen can produce a profound allergic response. Allergy describes the hypersensitivity reaction that occurs upon re-exposure to a sensitizing allergen.
A patient's allergic potential is determined by genetic predisposition. If one parent is atopic, a child is four times more likely to manifest allergic disease. If both parents are atopic, the child's chances increase tenfold. Allergy typically presents in childhood; however, a second group of individuals develops allergies later in life, typically between 18 to 35 years.
Allergy has significant social impact. Treating allergy is among the most common reasons for doctor visits, with the cost to the healthcare system exceeding $18 billion annually.
Clinical Allergy
The most common forms of allergic disease seen by eyecare professionals are seasonal (SAC) and perennial (PAC) allergic conjunctivitis. Both SAC and PAC present with the classic red, itchy eyes and a watery discharge. Initial sensitization requires both an atopic predisposition and the presence of allergen in the tears.
Seasonal allergy peaks in the spring and early fall as environmental allergen levels rise. Pollen, ragweed and molds are the most common causes. Perennial allergy occurs year round, and with more time spent indoors and the growing use of cosmetics and medications, it has become increasingly common. Animal dander and dust mite feces are common causes. In general, perennial allergy tends to be milder. However, it is often exacerbated by locale-dependent seasonal allergy spikes. In both conditions, involvement of the nasal and nasopharyngeal mucosa is common.
The prevalence of both SAC and PAC continues to rise, suggesting environmental conditions that favor increasing exposure to naturally-occurring antigens or heightened individual sensitivity. In either case, more patients than ever suffer from SAC and PAC.
Giant papillary conjunctivitis (GPC) is a chronic yet still poorly understood allergic and irritative response. Associated with contact lenses, exposed sutures and other foreign objects within the eye, the genesis of GPC is clearly multifactorial part allergic and part mechanical. Protein normally present in the ocular environment coats the foreign object and becomes antigenic. Prolonged antigen contact with concomitant mechanical irritation produces the large papillae on the superior tarsal conjunctiva characteristic of the disorder.
Although GPC is often associated with or exacerbated by other allergy, it is not associated with an increase in mast cells, eosinophils or histamine in the tears. However, chronic inflammatory cells are found in greater numbers.
Vernal keratoconjunctivitis (VKC) and atopic keratoconjunctivitis (AKC) are relatively rare but serious forms of ocular allergy. AKC is classically associated with atopic dermatitis and can be extremely destructive and difficult to manage. VKC typically presents in the early spring and persists though the summer. Affecting young males, it can be disabling. It is associated with large cobblestone papillae that can be florid, a ropy mucous discharge and intense, almost painful itching. Both AKC and VKC may be sight threatening.
Mast Cells
Mast cells are responsible for mediating allergic response in the conjunctiva as well as in other tissues throughout the body. Approximately 50 million mast cells exist within the human eye. They remain deep within the substantia propria until an active allergic state increases their presence in superficial tissues. Histologically and functionally, mast cells are largely indistinguishable from circulating basophils, particularly in regard to cellular contents.
A concept of growing importance, especially in the context of understanding how medications work, is mast cell heterogeneity. Tryptase and chymase are neutral proteases that are stored pre-formed in mast cell granules. Based on neutral protease composition, there appear to be at least two subtypes of mast cells. MCt type cells contain only tryptase. They are commonly found in mucosal tissue. Mast cells containing both tryptase and chymase (MCtc type) are normally found in connective tissue such as the skin and within areas where the mucosa interfaces with the environment like the conjunctiva. Mast cell types also differ by species, making animal studies potentially misleading.
The ultrastructural characteristics of MCt and MCtc types may differ, but functionally, both mediate allergic response in similar ways. Granules within the mast cell's cytoplasm contain histamine, the principal mediator of allergy, a variety of other preformed mediators including heparin, tryptase and/or chymase as well as other inflammatory, tissue destructive, chemotactic and vasoactive substances. Other potent mediators are synthesized upon activation of the mast cell including prostaglandins and leukotrienes.
Actual degranulation occurs when specific immunoglobulin E (IgE) molecules, bound to mast cell surface receptors, are cross-linked by antigens. Although the actual mechanism remains poorly understood, an inrush of calcium ions is believed to precipitate mast cell degranulation. Microtubules form, linking granules with the mast cell membrane allowing their contents to spill out into the extracellular space.
The Allergic Response
Allergy is a type I hypersensitivity reaction which is mediated by immunoglobulin type E (IgE). It occurs in three distinct phases: sensitization, early and late.
Sensitization. Sensitization to an allergen occurs on initial exposure and is a background process that produces no signs or symptoms. In the eye, sensitization begins with the allergen entering the tears and contacting the conjunctival surface. The allergen is rapidly identified by macrophages or langerhans cells which function as antigen-presenting cells (APCs). The APC phagocytizes, processes and alters the APC surface. The newly formed allergen/APC complex interacts with helper T-lymphocytes to produce cytokines, which facilitate direct interaction with naïve B cells. The B cells proliferate and differentiate into mature plasma cells. They ultimately secrete allergen specific IgE, which binds to high affinity receptors on sensitized mast cells (MC) and basophils. This prepares them to respond to subsequent antigen exposure.
Early phase. Subsequent exposure of a sensitized mast cell to a previously-encountered allergen precipitates mast cell degranulation, resulting in the release of a wide array of inflammatory mediators. Degranulation produces rapid changes in the local environment through the release of preformed mediators like histamine.
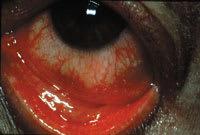
Papillary reaction associated with SAC
Three distinct types of histamine receptors have been identified: H1, H2 and H3. Of these, H1 and H2 receptors are present in the eye. Histamine binds to receptors located on adjacent tissues within the conjunctiva. H1 receptors are primarily responsible for itching. Vasodilatation and increased vascular permeability cause focal edema and conjunctival chemosis secondary to H1 and H2 receptor binding.
Degranulation begins within seconds of allergen contact, resulting in the rapid release of preformed mediators, the most important being histamine. Synthesized mediators are also released by the mast cell. These include prostaglandins, leukotrienes, cytokines and platelet activating factor (PAF). The newly-formed mediators contribute to the inflammatory reaction and incite recruitment of additional inflammatory cells, leading to the late-phase reaction.
Late Phase. The late phase reaction is cell mediated, with eosinophils being the chief inflammatory leukocyte involved. Cytokines and other inflammatory mediators released by mast cells activate local inflammation and act as chemo-attractants to recruit cells from the circulation. Increased vascular permeability and a complex process of adhesion facilitate infiltration of circulating eosinophils, neutrophils and basophils. The presence of inflammatory cells is associated with greater chronicity, increased inflammation and tissue damage.
The late phase of the allergic reaction begins four to 12 hours after the initial activation and release of mediators from the mast cell in more severe allergic states, conditions such as VKC or AKC. There is evidence that late-phase reactions do not occur in SAC, especially when appropriately treated. No increase in eosinophils occurs in SAC. Eosinophils migrate to the site of chronic allergic reaction following a gradient of mediators released by mast cells. This is a relatively slower process, requiring several hours before the inflammatory cells move to the site of the allergic reaction and begin to release their own pro-inflammatory mediators. This additional damage to existing mast cells boosts IgE production through cytokine release, which increases mast cell population. In addition, attraction of other inflammatory cells prolongs and exacerbates early-phase symptoms and ultimately leads to greater tissue damage.
Some mediators like eosinophillic major basic protein (EMBP) are particularly destructive. In severe conditions like VKC, EMBP-induced shield ulcers may lead to corneal scarring and subsequent vision loss. The late phase is more typically associated with chronic allergy. With the advent of more effective anti-allergy medications that prevent mast cell degranulation and effectively block inflammatory mediators, late phase reactions generally occur only in chronically untreated or more severe allergic conditions.
Allergy and The Contact Lens Wearer
With 20 percent of the U.S. population suffering from allergies, many contact lens wearers are also allergy sufferers. Not that many years ago, allergy was a relative contraindication to lens wear. Today, improvements in lens care products, single-use disposable lenses and better medications have allowed all but the most severely affected to wear contact lenses through the worst of allergy season.

Seasonal allergic conjunctivitis
Soft contact lenses in particular have always been a double-edged sword for allergy sufferers. While they serve as an effective barrier for the sensitive limbal area and surrounding conjunctiva, they also tend to bind allergens to the surface and biofilm coating. With the advent of single-use disposable lenses, sensitizing contaminants are discarded daily, allowing even highly allergic patients problem-free lens wear. Breaking new ground, CIBA Vision's Focus Dailies disposable lens was recently granted an indication for the relief of itching by the FDA.
Since daily disposable lenses are available only in limited parameters, lenses that are less frequently replaced may be required for allergic patients. Allergic patients wearing lenses for longer periods are prone to greater discomfort, increased protein build-up and deposits, inflammation and, ultimately, GPC. Several strategies can increase wearing time, decrease discomfort and reduce dropouts among these patients.
- Increase the frequency of replacement during peak allergy season. This removes bound allergens, protein build-up and lens debris. The decreased antigenic load is less likely to exacerbate allergy-related symptoms. Patients who have low toric prescriptions may be able to temporarily wear spherical disposable lenses, which are usually less expensive and can be replaced more frequently.
- Select care systems properly. Preservatives used in early care products were often inherently sensitizing. For example, thimerosal was notorious for causing red eyes. Modern care products rarely cause reactions and are unlikely to sensitize patients or exacerbate existing allergy.
The newer one-step, "no rub" multi-purpose disinfecting solutions appear particularly helpful in managing allergy patients. Allergic patients are as non-compliant as normal patients are. Making lens care easier improves the likelihood that lenses will be properly cleaned. Alcon's Opti-Free has no-rub approval and has excellent protein removal properties. Allergan's Complete and Bausch & Lomb's ReNu MultiPlus solutions recently received no-rub approval as well. Sensitive patients may benefit from hydrogen peroxide-based systems which lack preservatives that can add to antigen load. - Don't be afraid to add adjunctive cleaners during allergy peaks. Alcon's SupraClens is easy to use and effectively removes protein and bound debris from lens surfaces. Conventional enzymes are less helpful due to increased complexity but may be useful with some patients. Daily cleaners have largely fallen by the wayside, but CIBA's Miraflow is an excellent adjunct for heavy depositors, especially during allergy season.
- The tear film dilutes and washes away allergens. Because contact lenses act as moisture sinks that reduce tear volume through evaporation, contact lens wearers are more prone to allergy attacks. Care should be used in identifying and treating meibomian gland dysfunction since it results in evaporative dry eye. Warm compresses and lid massage will often reduce allergic symptoms in lens wearers. Lens wearers with dry eye should use tear supplements in addition to any medication. Lens rewetting and non-preserved drops can be used to help increase tear volume. Recently, Alcon introduced Clerz Plus, a lens drop with in-eye protein removal capability. This added capability might benefit allergy patients in particular.
- Treat ocular allergy using one of the newer broad-spectrum products that can be applied twice daily. BID dosing encourages compliance and is especially helpful for contact lens wearers. Commence treatment several weeks prior to the start of allergy season since mast cell stabilizers take a while to "kick in." Early treatment minimizes the risk of allergy interfering with contact lens wear as allergy season heats up. State-of-the-art products like Patanol (olopatadine, Alcon) do not require pretreatment or loading doses because the onset of effect is extremely rapid.
GPC has traditionally been managed medically with cromolyn sodium drops; however, newer combination products like Patanol and Zaditor appear to have superior effectiveness. Lotemax (loteprednol etabonate 0.5%, Bausch & Lomb), a new generation topical steroid, has FDA approval for treatment of GPC.
Patient Management
With a bewildering array of new medications, it is important to evaluate manufacturers' claims cautiously. Mast cell heterogeneity makes direct comparison between respiratory mucosal studies and ocular performance conjunctiva impossible.
Selection of appropriate treatment is very much a function of experience. There is substantial geographic and individual variation among allergy sufferers in terms of prevalence, causation and most effective treatment. No single medication will work for all patients, and communication is an important element in a successful management plan.
Treating ocular allergy is one of the surest ways to build a successful ophthalmic practice. It is an essential requirement in the contact lens practice. Allergy is acutely uncomfortable and disruptive. Modern medications make treatment convenient and effective and bind patients to the practice.

|
Medical Management of Ocular Allergy |
The number of medications available to treat ocular allergy has recently grown. Although a variety of OTC anti-allergy products are available, they are less effective than current prescription medications. OTC products combined with unsupervised patient self-administration is also more likely to cause ocular irritation and rebound. Key anti-allergy medications include: Antihistamines. These drugs are a mainstay of systemic allergy treatment but tend to dry the ocular surface and exacerbate allergy due to diminished tear film volume. They are inadvisable for patients who primarily suffer from ocular manifestations of allergy. Topical antihistamines are particularly effective at reducing itching and redness during acute allergy attacks. Because these drugs work by blocking histamine receptors, patients should be advised to administer topical antihistamines at the first sign of itching to minimize subsequent allergic response. Emadine (emadastine, Alcon) and Livostin (levocabastine, CIBA) are effective and relatively inexpensive examples of topical antihistamine medications; however, QID dosing and a short duration of action reduces their usefulness with contact lens wearers. Emadine has up to QID approval and may be effective at lower doses. Recent research evidence suggests that over application of antihistamines may actually precipitate increased allergic response due to mast cell degranulation caused by damage to cell membranes. This dose-dependent effect appears to occur with all currently available medications having antihistamine effects with the exception of multi-action Patanol (olopatadine, Alcon), which balances both antihistamine and mast cell properties. Topical Steroids. Because of their potential for serious side effects, topical steroids have previously been reserved to treat severe ocular allergy. However, the introduction of new generation products with improved side effect profiles like Alrex (loteprednol etabonate 0.2%, Bausch & Lomb), has spurred increased steroid use for allergic conjunctivitis. Earlier generation steroids like FML (fluoromethalone, Allergan) and Vexol (rimexolone, Alcon) are less frequently used. Topical steroids are helpful for initial pulse treatment until other medications like mast cell stabilizers can take effect. Typical dosing is QID. Until proven safe for chronic use, topical steroids should be reserved for severe allergies that are unresponsive to other treatments. Topical NSAIDs. These drugs inhibit the production of prostaglandins and thromboxane by blocking the activity of cyclo-oxygenase. They relieve itching associated with allergic conjunctivitis; however, they are less frequently used since better and more effective options have become available. Acular (ketorolac tromethamine, Allergan) and Voltaren (diclofenac sodium, CIBA) are examples of topical NSAIDs. Mast cell stabilizers. These medications have been a mainstay of allergy treatment for many years. Safe and effective, they are used for asthma and allergic rhinitis in addition to allergic conjunctivitis. Mast cell stabilizers include: Alomide (lodoxamide tromethamine, Alcon), Opticrom (cromolyn sodium, Allergan), Crolom (cromolyn sodium, Bausch & Lomb), and Alamast (pemirolast potassium, Santen). Multi-action medications. Patanol was the first and remains the market leader in this class of multi-action allergy medications. Good comfort, combined antihistamine and mast cell stabilization with additional anti-inflammatory capability make this drug an excellent choice. Zaditor (ketotifen, CIBA Vision) also combines mast cell stabilizing and antihistamine effects along with inhibition of eosinophil recruitment, which may be beneficial in chronic allergic states such as VKC. Alocril (nedocromil sodium, Allergan) is a new class of ophthalmic mast stabilizer, has similar multiple actions; however, a high rate of headaches as a side effect limits its use in some patients. BID dosing and excellent efficacy make these medications ideal for contact lens wearers and cost effective for all allergy-suffering patients. |



