readers' forum
Compliance to Wear and Care: What Are the Recommendations?
BY PETER C. DONSHIK, MD
December 2001
Patient satisfaction and compliance with contact lens replacement schedules depend on many factors, including the patient's desire for good vision, comfortable lens wear, absence of complications and with a minimal investment of time in contact lens care. Prior to the introduction of disposable and frequent replacement contact lenses, our concept was to try to do everything possible to keep the contact lens as clean as possible and to replace them annually. However, with the introduction of frequent replacement and disposable contact lenses, a variety of studies have shown that replacing contact lenses at more frequent intervals results in a decrease in complications associated with contact lens wear. With the variety of wearing schedules and choice of solutions now available, the chance of a patient confusing their contact lens regimen instructions is higher. Compliance, or the lack of compliance, could affect a patient's success in wearing contact lenses and affect the occurrence of complications.
Non-compliance Studies
Patient compliance to a wearing and replacement schedule, contact lens care and follow-up exam need to be reviewed. Studies by Ky and co-workers revealed that a significant number of contact lens wearers do not adhere to the recommended lens care guidelines and probably have an inadequate understanding of these guidelines. Turner and co-workers reported that 91 percent of patients in their study were non-compliant with one or more steps in the care regimen. This is clinically significant regarding the safety of contact lens wear. They reported that those factors affecting comfort were less likely to be areas where the patient is non-compliant. Only 34 percent of patients failed to follow one or more of the steps judged to affect comfort.
This was further supported by a study by Turner and co-workers who found non-compliance which significantly affects safety was more common than non-compliance affecting comfort. On the other hand, according to Asbell and co-workers, 90 percent of patients in their study were compliant with replacement schedules. Phillips and Prevade found that while only 32 percent of their patients were compliant with their lens care regimen, 97 percent were compliant with their replacement schedule. However, these studies were conducted early in the disposable/frequent replacement experience. Today, patients often admit to stretching replacement cycles.
|
|
|
|
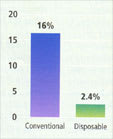
Figure 1. Incidence of GPC with extended wear hydrogel contact
lenses. |
|
Replacing Lenses
Studies by Poggio and Abelson, as well as Boswell and co-workers, have shown that, with extended wear, the introduction of disposable contact lenses significantly reduced complication rates and decreased the number of patients dropping out of lens wear (but had no effect on the incidence of ulcerative keratitis). The incidence of giant papillary conjunctivitis (GPC) with conventional extended wear lenses was 16 percent; the incidence with disposable extended wear lenses (replaced at one or two weeks) was 2.4 percent (Figure 1). Considering extended wear and GPC, replacing contact lenses every one to two weeks was significantly better than replacing lenses annually.
With daily wear, the introduction of frequent replacement lenses has also decreased the incidence of complications. Poggio and Abelson have shown that patients replacing lenses on a two-week interval, compared to a six-month to one-year interval, had fewer complications. A study by Suchecki, Ehlers and Donshik evaluated the incidence of contact lens-related complications in daily wear with various replacement schedules. They found that the complication rate was significantly lower for daily disposable lens wearers. This supports the concept that the more frequently patients replace their lenses, the fewer episodes of complications associated with ocular surface disease and inflammation will occur.
|
|
|
|
Figure 2. Incidence of GPC in daily wear frequent replacement contact
lenses. |
This was further supported by a study by Porazinski and Donshik that reviewed the incidence of GPC in frequent replacement contact lenses. They found that in patients who replaced their lenses every three weeks or less, the incidence of GPC was 4.5 percent (Figure 2), while those who replaced their lenses every four weeks or more had an incidence of 36 percent.
GPC and 30-day Wear
This significant difference in the incidence of GPC, as determined by contact lens replacement, is of concern as we look toward the new high-Dk silicone hydrogel contact lenses for 30-day continuous wear. Studies by Ren and co-workers suggest that these lenses will reduce infectious keratitis in extended wear. High-Dk silicone hydrogel lenses cause less hypoxia and bacterial binding than conventional hydrogels.
However, what is the effect of the surface and edge design of these contact lenses on both the cornea and conjunctiva when they are worn for 30 days continuously or even worn for seven days and replaced monthly? Will these lenses create problems which result in more side effects chairtime for the practitioner and more inconvenience for the patient?
The preliminary results of high-Dk silicone hydrogels are promising. In a one-year study of 504 patients wearing Bausch & Lomb PureVision lenses, Nilsson reported a relatively low complication rate. While there were no sight-threatening events and no incidence of ulcerative keratitis reported, inflammatory reactions were observed. Corneal staining was noted in approximately 10 percent of the cases. Corneal infiltrates occurred in 2 percent to 5 percent of the cases. Tarsal conjunctival abnormalities (GPC changes) were present in 2 percent to 3 percent of the cases. It was interesting to note no significant difference in complication rates for high-Dk silicone hydrogel contact lenses worn continuously for 30 days and then replaced as compared to the same lenses worn for seven-day intervals and replaced after 30 days.
|
|
|
|
Figure 3. Incidence of contact lens-related
GPC. |
|
It is difficult to compare the results of this study with studies on frequent replacement or daily disposable lenses regarding conjunctival complications. Data submitted to the FDA (Figure 3) indicates that the incidence of GPC is higher with 30-day silicone hydrogel (CIBA Vision Focus Night & Day) lenses (3.88 percent) compared to etafilcon A control lenses (Vistakon Acuvue) worn for one-week extended wear and replaced weekly (0.81 percent). With conventional hydrogels, greater patient satisfaction and less ocular inflammatory responses occur when lenses are replaced frequently.
In my opinion, contact lenses are more comfortable when patients replace them every day, followed by weekly replacement and monthly. As high-Dk silicone hydrogel lenses are introduced, it remains to be seen whether lenses replaced on monthly are as comfortable and free of ocular inflammatory events as lenses replaced on a seven-day or daily basis. High-Dk silicone hydrogel lenses have addressed corneal hypoxia and may have resolved infectious keratitis associated with extended wear. The FDA is requiring a large, post-approval clinical study to determine the incidence of microbial keratitis. The development of high-Dk silicone hydrogel lenses has been a significant achievement in the contact lens field. However, we must study the effect of these lenses on the ocular surface.
To receive references via fax, call (800) 239-4684 and request document #77. (Have a fax number ready.)
Dr. Donshik is a clinical professor at the University of Connecticut Health Center. He received a grant from Vistakon for writing this article.