contact lens case reports
Tilt Adds Complexity to Graft Fit
BY PATRICK J. CAROLINE, FAAO, & MARK P. ANDRÉ, FAAO
February 2001
Patient EW presented with a longstanding history of keratoconus OU. He had undergone an epikeratophakia procedure on the right eye in 1988, which today is correctable to 20-50 with a spectacle Rx of 2.75 2.25 x 47, VA 20/50. He subsequently underwent a penetrating keratoplasty to the left eye in 1999 (Figure 1)

Figure 1. Patient EM
six month post-op.
Postoperatively, his left cornea stabilized with K readings of 44.25 @ 144 / 47.12 @ 54. Computerized corneal mapping showed an asymmetrical distribution to the topography with significant mid-peripheral nasal steeping from 7 o'clock to 11 o'clock and temporal flattening from 1 o'clock to 6 o'clock (Figure 2).

Figure 2. Corneal mapping one year post-op, note the temporal graft tilt from 7 o'clock to 11
o'clock.
An asymmetrical corneal topography, or graft tilt, is a common postoperative complication in penetrating keratoplasty. The mechanisms for the tilting include improper suture placement, unequal suture tension, uneven trephination of the donor button or recipient bed and pre-existing corneal topography (Figure 3).
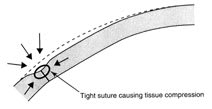
Figure 3. Suture compression resulting in a localized corneal
steepening
The presence of graft tilt may complicate the fitting of rigid contact lenses depending on the location of the tilt (steepest portion). If the tilt is inferior, design an RGP to align the flatter superior cornea, which allows the lens to lift off inferiority (similar to a keratoconus pattern). However, if the tilt is nasal or temporal, the lens will exhibit significant edge lift over the steepest area of the mid-peripheral cornea. This can result in excessive lens decentration and inconsistent VA.
The lens we selected was the Post-Graft Design from Lens Dynamics in Denver. The design incorporates a large overall diameter of 10.4mm to aid in centration on these often asymmetrical or irregular corneal topographies. The design also incorporates a large 9.0 mm optical zone which can be adjusted (made smaller) especially in cases in which the central portion of the graft has steepened.
Our fitting objective was to select a diagnostic lens with a base curve that would be steep enough to clear the apex of the cornea and land on the flatter temporal mid-peripheral cornea from 1 o'clock to 6 o'clock (Figure 4). Ultimately, the patient was fit with a lens of 46.00 diopters, 3.25D, 10.4mm, visual acuity 20/25, with a comfortable wearing schedule of 14 to 16 hours a day.
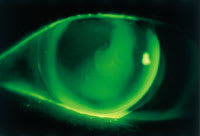
Figure 4. Fluorescein pattern of with mid-peripheral bearing along the temporal (right side).
Patrick Caroline is an associate professor of optometry at Pacific University and an assistant professor of ophthalmology at the Oregon Health Sciences University.
Mark André is director of contact lens services at the Oregon Health Sciences University.



