continuing education
Preventative Contact Lens Care: Part I
PAUL WHITE,
O.D., AND JOSEPH BARR, O.D., M.S., F.A.A.O.
February 2001
This first installment of a three-part series explores the preliminary evaluation of prospective contact lens patients.
The first stage of contact lens fitting is a comprehensive examination to determine the advisability of application and the probability of success with each patient. This evaluation has three goals, which constitute an operational definition of successful contact lens application: (1) objective evaluation showing that there is not and probably will not be significant ocular tissue disturbance; (2) subjective evaluation showing that there will be satisfactory visual performance, comfort and wearing time; and (3) cosmetic evaluation showing that the patient will look good while wearing the lenses.
Four related questions must be answered to determine whether these goals are attainable: Is the patient appropriate in terms of psychological, environmental, physiologic and visual factors? Are presently available contact lens materials and designs suitable for the patient? What are the best lens replacement cycles? What are the least toxic and most compliant lens care solution systems?
Advancements over the past decade have significantly improved the probability of success for most patients. Disposable and planned replacement soft contact lenses have decreased ocular tissue complications and unscheduled office visits while producing good visual performance, comfort and wearing time. Less toxic and easier to use solutions have contributed to patient success, as has the large available parameter range of well-designed spherical, toric, multifocal and tinted disposable and planned replacement soft contact lenses.
These watershed advancements are attested to by practitioners' and patients' preferences and satisfaction. Over 80 percent of new soft lens patients are fitted with disposables or planned replacement, which are used by over 70 percent of all soft lens wearers. Multi-purpose solutions (MPS) comprise over 80 percent of the sales of chemical disinfection systems for soft contact lenses. Disposable and planned replacement lens use and MPS increase biocompatibility to ocular tissues, ease of use and patient compliance.
Part I of this three-part series discusses the patient's psychology and pre-existing disease conditions related to preliminary evaluation. Proper preliminary evaluation of contact lens candidates does not ensure success, but it greatly reduces the probability of failure. All contact lens patients must be monitored not only during their first several months of wear, but also as long as they continue to wear contact lenses. Short-term and long-term problems are not always predictable.
Part II (May 2001) will discuss fitting, lens replacement cycles, reduction of ocular tissue complications and ongoing follow-up care. Part III (August 2001) is devoted to an overview of contact lens solutions from patient, in-office, Food and Drug Administration (FDA) and Center for Disease Control (CDC) perspectives.
Psychological Factors
Almost all contact lens practitioners agree that psychological factors are extremely important in contact lens applications. Although contact lens fitters are neither psychologists nor psychiatrists, practitioners must understand psychological factors relevant to their work. Such understanding assists them in evaluating a prospective wearer and managing an accepted wearer.
Motivation is directly related to the patient's true need to replace spectacles with contact lenses. As need and motivation increase, advisability of contact lens application increases. Three needs may motivate a person to acquire contact lenses: visual enhancement, cosmetic and ego enhancement and protection or therapy. Most contact lens patients are motivated by a desire for cosmetic and ego enhancement, as are patients who undergo corneal refractive surgery. Practitioners often have to compare and contrast contact lenses and corneal refractive surgery advantages and disadvantages.
Motivation in young people may be initiated by the parents' disapproval of the young person's appearance with spectacles. With younger patients, it is advisable to understand the desires of both patient and the parents and their opinions of contact lenses. To produce the desired result, contact lenses must be used and cared for properly. Evaluate the general maturity of the patient and the patient's ability to assume responsibility for obeying instructions, handling and maintaining the contact lenses properly. This is especially important for pre-teenaged candidates.
It is the practitioner's responsibility to provide accurate and complete information in each case concerning advantages and disadvantages of contact lenses. Both practitioners and patients must make decisions pertaining to the advisability of contact lens application. The practitioner must decide if the patient should be fitted and if there is a satisfactory probability of success. The patients must decide whether to be fitted after receiving information on the advantages, disadvantages and probability of success in their case. Discuss five key topics with each patient: safety; visual performance; annoyance and discomfort; cosmetic and ego enhancement; and economics.
Practitioners first must ascertain whether a patient has never worn contact lenses, is presently wearing lenses (and how successfully) or has discontinued lens wear (and the reasons for this). Patients in each of these groups have valid and invalid preconceptions based upon the alleged virtues of contact lens products, positive and negative stories related by friends and family or reported in the media, and their own experiences if they are present or past lens wearers. In effect, each patient has a specific psychological set.
Goals and Expectations
Patients with unreasonable goals for and expectations from contact lenses are more likely to fail. Therefore, it is essential to ask patients to verbalize their goals and expectations related to vision, annoyance and discomfort, cosmetic enhancement, convenience, wearing time, lens care and cost. The practitioner should discuss these to help the patient develop realistic goals and expectations.
Most patients assume that vision with contact lenses is equal to or better than vision with spectacles. This is often, but not always, true. After the examination, evaluate and discuss probable visual performance with each patient.
Visual performance with contact lens correction as compared to spectacle correction is aided by a slight increase in light transmission (assuming tinted contact lenses are not used), an increase in usable visual field and a better quality of retinal image. The quality of the retinal image is improved by reduction of aberrations and more consistent fixation through the optical center. With high refractive powers, all these benefits are increased. The highly myopic patient also obtains a considerably larger retinal image.
Some patients dislike the cosmetic effect of spectacles so much that they use them only when absolutely essential. In such cases, vision with contact lens correction should not be compared to vision with spectacle correction. Rather, the comparison should be between vision with contact lens correction and vision with limited or no use of spectacles.
Overall visual performance for most patients is quite satisfactory with contact lenses, and in some cases it is significantly better than visual performance with spectacles. However, there are three relatively common visual disadvantages arising from the use of contact lenses. First, an astigmatic error may be left uncorrected, although this is much less likely to occur today with the vast array of toric contact lens options. Second, contact lenses can become coated by transfer of materials from the fingers or precorneal fluid. Such a coating blurs vision, just as a coated spectacle lens blurs vision. Replacing lenses at shorter intervals denies protein and other deposits the opportunity to build up on the lens surface. Optical clarity depends upon clean contact lens surfaces and a stable pre-lens tear film. Lens deposits may cause lens surfaces to become more hydrophobic and to wet unevenly with a poor or quickly evaporated pre-lens tear film. Third, improper contact lens position or movement may produce vision problems.
Some patients have heard that contact lenses stop or retard the progression of myopia. Few practitioners believe this to be true with hydrogel lens wear, but some believe it to be true with rigid lens wear. Practitioners should discuss this with those patients who express it as an expectation from contact lens wear.
Patients should not be misled into believing that there will be no annoyance or discomfort during or after adaptation to contact lens wear. After adaptation, many patients are unaware of the lens, aside from the occasional instances when dust or wind cause brief discomfort. Many other patients are slightly aware of, but not annoyed by, the presence of the lens. A few patients are annoyed by seemingly well-fitted lenses to a degree that wear is discontinues or continued only on a part-time basis.
Because cosmetic enhancement is usually the prime motivating factor, the patient assumes his or her appearance will improve with contact lenses. Properly fitted contact lenses can fulfill this need. When cosmetic need is great enough and is fulfilled, patients usually are satisfied with contact lenses in spite of other disadvantages. When cosmetic need is slight or other disadvantages are great, patients may be dissatisfied.
Some structural or positional anomalies of the anterior segment of the eye such as strabismus, ptosis, pinguecula and coloboma of the lids, are more apparent with contact lenses than with spectacles because of the masking effect of spectacles. In such cases, the patient may mistakenly assume that the condition will be no more or even less apparent with contact lenses. To avoid subsequent disappointment in such cases, the patient should be properly informed that this may occur.
Patient goals for wear time may vary from a few hours several times a week for social or athletic purposes to a month of continuous wear. Disposable or programmed replacement soft lenses are often preferred by patients who want contact lenses for social or athletic pursuits. Most patients desire 12 to 14 hours of daily wear. The practitioner should discuss the probability of achieving the wear-time goal, as well as the safety issues involved. Present FDA approval for non-aphakic extended wear is a maximum of seven days and six nights.
Patients should expect to spend a few minutes each day to care for their daily-wear lenses. Replacing lenses more frequently simplifies lens care. Enzymatic cleaning may not be needed if replacement is frequent enough, and MPS can clean and disinfect the lenses between replacements. Daily disposable contact lenses require no care at all.
Simplicity of lens care increases patient compliance, which has historically been very poor with conventional soft contact lenses. They also should understand the costs involved in purchasing contact lenses and contact lens solution, as well as the costs of professional services. If they are unwilling to spend the time or money required, they are less likely to be successful and should be discouraged from contact lens wear.
Disease
Persons without present or past ocular disease conditions usually can safely wear contact lenses that are properly fitted, used and cared for. This fact is substantiated by the relatively few significant tissue disturbances compared to the relatively large number of wearers, especially with disposable and planned replacement soft lenses.
In some cases, contact lenses cannot safely be used in persons with present or past ocular disease conditions. A thorough case history and examination is necessary with every prospective contact lens patient to determine the disease status. The case history is directed toward obtaining information about past ocular disease conditions and symptoms suggesting current ones. The significance of any disease condition is evaluated in terms of the advisability of contact lens application. Each case must be considered on its individual merits and each practitioner's individual judgement. The following discussion is just a general guideline.
Any inflammatory or infectious ocular condition, and most degenerative conditions, generally should be cured before contact lenses are considered. Because degenerative conditions usually do not respond to treatment, the use of contact lenses often is contraindicated. Keratoconic and postsurgical patients are exceptions. Any injury should be cured and the tissues allowed to develop adequate strength before contact lenses are considered. There are two basic reasons for these generalizations: the contact lens may aggravate the disease condition or may cause misleading signs and symptoms that complicate diagnosis and treatment, and the disease condition may cause misleading signs and symptoms that complicate contact lens fitting.
Once a disease condition is cured, the advisability of contact lens application depends on the integration of five factors:
- The seriousness of the disease condition
- The possibility of spontaneous recurrence or the chronicity of the disease condition
- The possibility that the contact lens may cause activation of the disease condition
- The fitting complication
- The ability of spectacle lenses to correct the visual anomaly
The more significant any one of these factors becomes, the less advisable the application of contact lenses.
Consider the last factor in more detail. Even though the visual needs of many patients can be satisfied by spectacle lens correction, patients may desire contact lenses to satisfy psychological needs related to cosmetic enhancement. When such patients have a significant history of ocular disease based on the first four factors, it is often best to be more conservative with contact lens application. Conversely, some patients with a significant history of ocular disease are visually handicapped when corrected by spectacle lenses but not when corrected by contact lenses. Better fulfillment of visual needs may warrant a more liberal application of contact lenses for these patients, including therapeutic contact lens use. Complications occurring with therapeutic or bandage contact lenses are viewed quite differently from those occurring with cosmetic contact lens use. Even though the complications may take identical forms, the benefit-to-risk ratio is often very different.
For simplicity, ocular disorders may be considered in seven categories: inflammation and infection, degenerative disease, injuries, structural and positional anomalies, neoplasms, systemic disorders and symptomatic disorders. The disorders that are more important to contact lens application will be discussed in the categories of inflammations and infections, degenerations and structural and positional anomalies.
|
|
|
|
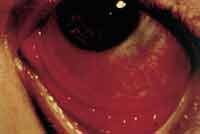
Figure 1. Chalazion. |
|
Inflammation and Infection
Blepharitis, chalazion, dermatitis, hordeolum and meibomitis are the most common eyelid inflammations (Figure 1). A contact lens may aggravate these conditions. The symptoms, signs, temporary tissue changes and at times the related exudates from these inflammations complicate contact lens wear. Eyelid inflammations should be cured before fitting is initiated. If there is a history of frequent recurrences, the advisability of contact lens application is decreased. Long-term antibiotic use, hot compress application and lid cleansing may be required. Any bacterial, viral or fungal conjunctivitis should be cured before contact lenses are applied (Figure 2). After trachoma is cured, contact lenses may be indicated to protect the cornea from the abrasive action of the residual lid scar tissue.
Allergic conjunctivitis associated with hay fever or vernal conjunctivitis is usually seasonal. Contact lenses should not be fitted during an episode. Because seasonal recurrences are typical, the patient should be informed that during an episode, contact lens wear may be less comfortable or may have to be temporarily discontinued. Daily treatment with ocular allergy medicines before and after contact lens wear may be helpful.
|
|
|
|
Figure 2. Acute follicular conjunctivitis. |
Chemical conjunctivitis generally should be cured prior to contact lens application. The exception to this recommendation is related to the fact that some chemically-caused cases of conjunctivitis are complicated by adhesions between the bulbar and palpebral conjunctiva (symblepharon). At times, a hydrogel or scleral contact lens is used to produce a physical barrier to the development of symblepharon. Whenever possible, the causative agent should be removed from the patient's environment to prevent recurrence. Often, the causative agent is related to the patient's occupation and cannot be eliminated. Under such conditions, contact lenses should not be worn at work.
Contact lenses should not be fitted on patients with severe giant papillary conjunctivitis (GPC) (Figure 3). GPC greater than Grade 1 will cause lens coating and subsequent discomfort and visual disturbances. The GPC should be greatly reduced prior to performing a fitting or refitting. Patients with a history of contact lens-induced GPC seem to have fewer recurrences when they are refitted with rigid gas permeable lenses or hydrogel lenses made of certain polymers or which are replaced frequently, including daily disposable lenses. Topical antihistamines, non-steroidal anti-inflammatory drugs (NSAIDs) and mast cell stabilizers may reduce symptoms, but it is necessary to eliminate the cause. Improved patient care of conventional soft lenses and reduced wearing time may help, but disposable and planned replacement lenses are often the best answer to prevent or remedy GPC because more frequent lens replacement reduces both the primary mechanical irritation and the secondary autoimmune reaction causes.
|
|
|
|
Figure 3. Giant papillary conjunctivitis. |
|
Metabolic conjunctivitis (keratoconjunctivitis sicca: Sjögren's syndrome) is a chronic condition marked by reduced lacrimal secretion. Usually, this reduced secretion contraindicates contact lens application. An exception involves treatment, usually by periodic introduction of artificial tears and saline irrigation, to supplement the reduced natural secretion, during which hydrogel lenses may be used to reduce evaporation of the normal secretion.
All keratitis must be cured completely before contact lenses are considered. If contact lenses are fitted, great care and close supervision must be used. Once a person has had keratitis, there may be susceptibility to recurrence. The contact lens may act as an exciting agent in the recurrence of keratitis.
Two excitatory causes of corneal ulcers are trauma and disturbances to corneal physiology, which may result from the use of contact lenses. Fitting a contact lens to an eye that has had a corneal ulcer should be approached with great caution. Conservative practitioners believe that usually such eyes should be fitted with contact lenses only if visual performance is significantly better with them than with spectacles. Contact lenses may produce superior vision because of the residual scar tissue or irregular astigmatism from the ulcer (Figure 4).
|
|
|
|
Figure 4. Neurotrophic corneal ulcer. |
Lagophthalmic keratitis is caused by excessive corneal exposure due to incomplete lid closure. Generally, contact lens fitting should not be attempted until proper lid closure is established. However, a hydrogel lens may be used as a therapeutic measure to retard dehydration.
Neuroparalytic keratitis is due to paralysis of the trigeminal nerve or disease or removal of the gasserian ganglion. The loss of corneal sensation decreases the patient's ability to detect undesired changes in the cornea. Because of this factor and the permanency of the condition, contact lens application usually is not advisable.
Contact lenses should not be fitted over corneal infiltrates. These gray or white patches in the stroma may be the result of an infectious or inflammatory process or they may be mechanically or chemically produced. In either case, they should be allowed to clear before fitting or refitting is done. Follow-up must be performed with care in these patients to avoid recurrence or complications (Figure 5).
|
|
|
|
Figure 5. Corneal infiltrates. |
After the infiltration of the cornea with new blood vessels in pannus or neovascularization, even though the primary disease condition is cured and the blood leaves the vessels, the vessels remain. A subsequent corneal disorder or irritation can result in the rapid recurrence of pannus through the old vessels.
Degenerations
Pinguecula and pterygia are conjunctival degenerative disorders. Presence of a pinguecula does not contraindicate contact lens application when the yellowish raised area is away from the limbus. When this area is near the limbus, fit the lens so that it does not touch the pinguecula, or the patient will experience discomfort.
Pterygia are considered to be caused by prolonged physical irritation, such as exposure to dust and wind. Contact lenses are contraindicated when an active pterygium is present because their use may contribute to such irritation. The growth area of the bulbar conjunctiva on the cornea vastly complicates contact lens fitting. Even after surgical removal, pterygia sometimes recur. The physical irritation of the contact lens may be an excitatory factor in recurrence. Apply lenses carefully after a pterygium has been surgically removed. Indications of recurrence usually suggest discontinuation of contact lens wear (Figure 6).
|
|
|
|
Figure 6. Pterygium. |
|
Corneal degenerative disorders may be divided into three groups: keratoconus, keratoglobus and others. Contact lens application often is advisable in keratoconus. Contact lenses may be contraindicated in any other corneal degenerative disorder. In such cases, the conditions usually are serious and progressive. Any tissue insult from a contact lens may complicate the condition considerably. If corneal degeneration progresses sufficiently, a corneal transplant may be necessary. Often, transplantation results in an irregular corneal surface. Contact lenses may be indicated to provide a regular surface and satisfactory visual acuity.
Structural and Positional Anomalies
Entropion often causes irritation to the cornea or conjunctiva. Entropion may be caused by irritation due to keratitis, conjunctivitis or loose skin (spastic entropion); it may also be caused by disease or injury to the tarsal and conjunctival portions of the lid (cicatricial entropion). Both entropion and its cause should be cured before contact lenses are applied. Carefully consider the advisability of contact lens fitting with the presence of entropion (Figure 7). Trichiasis often is associated with entropion. Trichiasis also may be caused by blepharitis or scars on the lid. The inverted lashes often irritate the eye, and they should be removed before contact lenses are applied. At times it may be inadvisable to operate or otherwise treat entropion or trichiasis. In these instances, a hydrogel contact lens may be used to protect the cornea and conjunctiva from irritation by the lids and lashes.
|
|
|
|
Figure 7. Entropion and trichiasis. |
Ectropion causes epiphora and chronic exposure conjunctivitis, which complicate contact lens fitting. Ectropion should be cured before contact lens application.
Blepharoptosis may complicate corneal contact lens fitting because of narrowing of the palpebral aperture and excessive pressure on the contact lens. Blepharoptosis may be relatively more apparent in contact lens wear than in spectacle wear. Spectacles mask blepharoptosis somewhat, and a ptosis crutch may be incorporated.
Coloboma usually occurs in the upper lid. It may complicate the fitting of corneal lenses because of poorer lens retention by the lid.
Epicanthus often gives the impression of a convergent squint. Spectacles tend to conceal this condition more than contact lenses; spectacles thus may be cosmetically preferable.
The undersurface of the upper lid may be scarred by trachoma, burns or injuries. In such cases, a contact lens may be applied to protect the cornea from the scarred lid.
Triangular or wedge-shaped white patches on the nasal and temporal bulbar conjunctiva may occur in xerosis. Xerosis may result from a general disease, such as vitamin A deficiency, or it may be a sequel of a local ocular problem, such as trachoma, burns or pemphigus. The primary disorder should be treated. Xerosis due to a vitamin deficiency, if not corrected early, can lead to corneal scarring and perforation. The residual effects in each case must be evaluated to determine the advisability of contact lens application. Because diphtheritic conjunctivitis and pemphigus are serious, contact lenses are contraindicated.
Visual acuity of a patient with an irregular or scarred cornea is often considerably better when contact lenses are applied, especially rigid lenses. Corneal irregularity and scarring often are a result of an ocular disease disorder. Advisability of contact lens fitting must be considered in terms of the causative disease disorder. Corneal irregularity and scarring may make it difficult to achieve a desired relationship between the posterior surface of the lens and the anterior corneal surfaces.
Examination
A comprehensive eye examination, including tests of vision and visual function, is performed prior to contact lens fitting as well as on an annual basis. Emphasis is placed on slit-lamp biomicroscopy of the eyelids, conjunctiva, cornea and especially precorneal fluid. Measurements of corneal topography, vertical palpebral aperture, horizontal iris diameter and pupil are taken. Eyelids, blinking and global and orbital characteristics are evaluated.