SILICONE-HYDROGEL LENSES
Boost Oxygen Transmission with Silicone-Hydrogel Lenses
By William J.
Lahners, MD,
Michael A. Ward, MMSc, FAAO, and Buddy Russell, FCLSA
June 2001
Since the first hydrogel material was described for use as a soft contact lens in the early 1960s, soft contact lenses have become an extremely popular and successful method of correcting refractive errors. Advances in the design of hydrogel lenses have created soft contact lenses that are comfortable, highly reproducible, inexpensive and require only minimal adaptation.
In the early 1970s, clinicians began using soft contact lenses as therapeutic bandage lenses. The bandage lens effectively treats surface disorders via its mechanical properties. The lens provides protection to an injured or unstable ocular surface by reducing lid trauma, increasing wetting and dispersing an unstable tear film. Contact lenses create a smoother refractive interface, providing better visual acuity by reducing irregular astigmatism for patients with certain surface problems. In addition, hydrogel lenses are effective adjuncts to pain relief in many types of surface pathology by reducing trauma to exposed corneal nerves. Bandage lenses have also demonstrated utility as drug delivery systems. Advances in lens design and clinical experience have broadened the therapeutic indication for hydrogel lenses to include surface disorders such as persistent epithelial defect, shield ulcer in vernal conjunctivitis, recurrent corneal erosion, chemical injury, filamentary keratitis, bullous keratopathy, application of adhesives, exposed sutures and drug delivery.
One of the chief limitations in the use of hydrogel lenses as bandage lenses has been limited gas exchange due to the properties of hydroxymethylmethacrylate (HEMA)-based hydrogel materials. Treatment of surface disorders with a bandage lens usually requires extended wearing schedules, sometimes for up to several months. This has previously exposed patients to potentially serious hypoxic stresses.
Contact lens-induced hypoxia has many deleterious effects on the cornea. Some of these include the release of inflammatory mediators, limbal hyperemia, corneal vascularization, midperipheral infiltrates, formation of a pannus, endothelial poly-
megathism, acidosis, corneal edema and damage to the corneal glycocalyx layer which may result in increased bacterial binding. In addition, contact lens-induced hypoxia with common hydrogel materials is detrimental to corneal wound healing. It has also been suggested that corneal hypoxia may increase the risk of bacterial keratitis from soft lenses.
You can decrease hypoxic stresses by decreasing wearing time or improving the oxygen transmissibility of the contact lens. Decreased wearing time is not a reasonable option when using the lens for therapeutic purposes due to extended wear schedules. In addition, other applications may require long wearing times (spectacle intolerance due to large anisometropias) that can induce hypoxia with many current hydrogel lenses even in the open eye state.
Oxygen transmissibility is the amount of oxygen that will diffuse through a lens per unit time for a given oxygen tension. It is expressed as Dk/L, which is the oxygen permeability of the contact lens material (Dk), divided by the lens thickness (L). Dk/t describes the oxygen transmissibility of a given contact lens at a specified thickness.
Three methods increase oxygen transmission through hydrogel lenses. First, increasing the water content of a hydrogel lens increases its material oxygen permeability. Second, decreasing the thickness of the lens will increase its oxygen transmission. Third, you can combine the two previous methods.
It has been suggested that the minimal Dk/t required to limit corneal hypoxia-induced edema to four percent (the amount of edema seen in the closed eye without a contact lens) is 87 (+/- 3.3X10(-9) (cm X ml O2)/(sec X ml X mmHg)). More recently, Harvitt and Bonanno reported that, based on their model, the minimum Dk/t for oxygen delivery to the basal epithelial cells is 23 in the open eye and 89 for the closed eye. These values agree with the values required to prevent corneal edema. No commercially available hydrogel lens in the United States provides a high enough Dk/t to meet the hypothetical corneal oxygen demands in the closed eye state.
Recently silicone-hydrogel contact lenses have entered the U.S. market for the treatment of up to 9.00D of myopia. These lenses combine the oxygen transmission of silicone with the wettability and comfort of soft hydrogels. For its PureVision (balafilcon A) silicone-hydrogel material, Bausch & Lomb combined a 36 percent water hydrogel with a silicone matrix, then treated the surface with a hydrophilic silicate (plasma) surface to enhance wettability. The lens has a center thickness of 0.09mm at 3.00D and a modulus of 120 g/mm2. It is currently available in a single base curve of 8.6mm with a 14.0mm diameter. It has a material Dk of 99 and a Dk/t of 110 (with a thickness of 0.09mm at 3.00D).
CIBA Vision also has a silicone-hydrogel contact lens, Focus Night & Day (lotafilcon A), with a material Dk of 140. It is currently awaiting FDA approval for the U.S. market.
The high Dk/t of the silicone-hydrogel polymer lenses is a great theoretical advantage over previous hydrogel polymers, both in extended wear and therapeutic bandage lens applications. We present three cases in which we successfully used the PureVision lens in applications demanding high oxygen transmissibility.
Case 1
|
|
|
|
Figure 1. Penetrating keratoplasty with vessles to wound. |
A 38-year-old computer programmer presented to our service complaining of visual difficulties at work. Her ocular history included myopia that had been treated with radial keratotomy (RK) in both eyes in the early 1990s, photorefractive keratectomy (PRK) OU in 1994 and laser in-situ keratomileusis (LASIK) OU in 1998. Her post-
operative course in her right eye was complicated, and she underwent penetrating keratoplasty in 1999. Her uncorrected post-operative visual acuity was 20/400 OD and 20/30 OS. Her manifest refraction was 10.00 +1.50 X 90 giving 20/25 visual acuity OD, and 1.75 +0.75 X 92 giving 20/20 OS. Slit lamp examination showed corneal neovascularization up to the donor-host interface, with a few vessels entering the graft (Figure 1). There was no evidence of anterior chamber inflammation or graft rejection. She could not achieve satisfactory results with spectacle correction due to severe anisometropia and a lesser degree of irregular astigmatism. Because of her high wearing time demands, history of recent penetrating keratoplasty and slit lamp findings, we wanted to minimize hypoxic stresses. RGP lenses were not an option due to the patient's history of rigid lens intolerance. We fitted her with PureVision lenses 8.6/-8.00/14.0 OD and 8.6/-1.50/14.0 OS and achieved visual acuities of 20/25 OD and 20/20- OS. Long-term (nine month) follow-up confirmed high patient satisfaction and no evidence of graft rejection or progression of vascularization.
Case 2
|
|
|
|
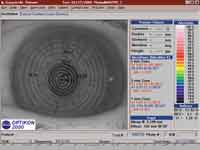
Figure 2. Photokeratoscope showing irregular surface over hexagonal incisions. |
A retired 61-year-old executive, who had undergone hexagonal keratotomy (Hex-K) in both eyes in 1992 complained of spectacle intolerance and visual difficulties while playing golf. His uncorrected visual acuities were 20/50 OD and finger counting OS. Manifest refraction showed 1.50 +0.75 X 135 OD and 6.00 sphere OS, giving acuities of 20/20 and 20/30, respectively. Topography show-ed central corneal ectasia in the left eye with irregular astigmatism (Figure 2). The patient could not tolerate the anisometropia in spectacle correction and was previously unhappy with the comfort of RGP lenses. We fit him with a standard daily wear hydrogel (42.5 percent water) contact lens OS, but in follow-up he complained of limited wearing time. We noted mild corneal epithelial edema, bulbar and limbal injection and early peripheral corneal epithelial neovascularization (Figure 3). We suspected that he was suffering from hypoxia-related effects and switched the patient into a silicone-hydrogel lens (8.6/-5.50/14.0). In follow-up, the patient reported improvement in comfort and wearing time, and the slit lamp signs resolved.
Case 3
A 53-year-old building contractor who had suffered severe alkali burns to both eyes 15 years prior presented with complaints of decreased vision, photophobia and foreign body sensation. He has a history of multiple surgeries and most recently had undergone repeat bilateral penetrating keratoplasty, lens extraction with posterior chamber intraocular lens implants and partial tarsorrhaphies approximately two years prior. Due to severe dryness, his lubrication schedule consisted of preservative-free tears every hour and Lacrilube ointment at bedtime.
|
|
|
|
Figure 3. Central cornea edema caused by low Dk hydrogel lens. |
|
His best spectacle corrected visual acuity was 20/400 OD and 20/200 OS. Keratometry was unobtainable. Slit-lamp biomicroscopy revealed an irregular surface with moderate to severe punctate epithelial erosions and superficial peripheral vascularization into the grafts in both eyes (Figure 4). There was no evidence of anterior chamber cell or flare, and there were no keratic precipitates.
We elected to use the PureVision lens (8.60/ -0.50/14.0) as a therapeutic bandage lens in each eye. We discontinued the Lacrilube ointment, but the artificial tears were continued as previously prescribed.
|
|
|
|
Figure 4. PureVision lens over graft in patient with tarsorraphy following alkali burn. |
One week later, the epithelium showed significant improvement and visual acuity had improved to 20/100 in the right eye and 20/80 in the left eye. The patient reported considerable relief from photophobia and irritation. At the three month follow-up, the corneal epithelium continued to show improvements, including minimal punctate staining and decreased edema and limbal injection.
Conclusion
Soft contact lenses are useful in cosmetic correction of refractive errors and as therapeutic devices. However, the shortcoming in all hydrogel materials to date has been limited oxygen transmission. Now there is a soft lens on the U.S. market that has a sufficient Dk/t to potentially prevent hypoxic-related events in the closed eye state. We believe that this makes silicone-hydrogel lenses uniquely qualified as long-term bandage lenses. In addition, they are easy to fit, easy to handle and comfortable.
Medically-indicated lens use does not necessarily mean extended wear. In two of the above-mentioned cases, the lenses are used on a daily wear basis. When being worn on an extended wear basis, we recommend removal once a week for cleaning and disinfection with a multi-purpose solution. Replace lenses every two weeks for extended wear and every four weeks for daily wear use.
This lens has become our lens of choice with patients requiring bandage lenses and/or experiencing wearing time difficulties, piggyback lens systems, post-surgical epithelial injury and evidence of corneal hypoxia from lens systems.
The Bausch & Lomb PureVision lens is not approved for therapeutic purposes and is currently approved only for seven days of continuous wear.
This work was supported by Research to Prevent Blindness, Inc., New York, NY, and a National Institute of Health CORE grant #P30-EY06360.
To receive references via fax, call (800) 239-4684 and request document #72. (Have a fax number ready.)
Dr. Lahners is a cornea and refractive surgery specialist and is the Director of Laser Vision Services at the Center for Sight, Sarasota, Florida.
Mr. Ward is an instructor at Emory University School of Medicine and Director of Contact Lens Service.
Mr. Russell, a certified ophthalmic technician and licensed dispensing optician, is an associate staff member with the Contact Lens Service at Emory University Eye Center