RGP insights
Fitting MDF DystrophyWith RGP Lenses
BY LORETTA B. SZCZOTKA, OD, MS, FAAO
June 2001
Epithelial basement membrane dystrophy (also called Cogan's microcystic epithelial dystrophy or map-dot-fingerprint [MDF] dystrophy) is a common bilateral disorder which presents with focal epithelial and/or stromal areas
focal epithelial and/or stromal areas of corneal irregularity. It compromises spectacle-corrected visual acuity if the affected area is within the visual axis or if the topographic effects extend into the visual axis.
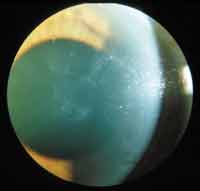
Epithelial basement membrane dystrophy can present with either focal or diffuse corneal irregularity. The classic patterns of epithelial and basement membrane abnormalities vary among patients. They may appear as dots (gray intra-epithelial opacities), fingerprints (clusters of concentric contoured lines), maps (geographic shaped circumscribed areas often combined with dots), blebs (fine, clear, round, bubble-like formations) and nets (refractile rows of blebs) (Figure 1). Nets and blebs do not result in epithelial erosions, but maps and fingerprints often do.
|
|
|
|
Figure 1. Epithelial basement membrane dystrophy |
|
In MDF dystrophy, patients often encounter epithelial erosions exacerbated by the mechanical friction of an RGP lens. Fitters fear this and often try soft contact lenses as the first line of contact lens therapy. Firm hydrogel, silicone-hydrogel or thick lenses are required to improve vision by masking the irregular corneal contour. MDF dystrophy patients that have 20/30 or better spectacle acuity are reasonable candidates for soft lens treatment. However, if the spectacle-corrected acuity is 20/40 or worse or if monocular diplopia is encountered secondary to the epithelial irregularity, the potential for improvement with soft lenses is minimal and RGP lenses should be tried.
RGP lenses not only improve visual acuity by correcting the corneal irregularity, but some believe they reduce the severity of the basement membrane changes. When fitting RGP lenses, the goal is to avoid harsh lens bearing over the areas of maps and fingerprints to prevent mechanical friction and potential corneal erosions. An apical clearance lens-to-cornea fitting relationship is usually recommended if the area of irregularity is centrally or paracentrally located (which is typically the case if the patient is seeking improved vision with RGP correction). A moderate to high Dk RGP material works well to preserve the integrity of the corneal epithelium and stroma. Additionally, meticulous lens cleaning, routine protein removal or the use of a strong emulsifying surfactant to solubilize deposits is recommended to remove back surface lens deposits which can increase the friction of higher Dk RGP lenses. I often recommend digital cleaning of the inside surface of the RGP with the little finger or a Q-tip, or emulsifying overnight soaking agents (such as the Claris system by Menicon, or Optimum by Lobob) to keep the inside lens surface scrupulously clean.
Dr. Szczotka is an assistant professor at Case Western Reserve University Dept. of Ophthalmology and Director of the Contact Lens Service at University Hospitals of Cleveland.