LOW ASTIGMATS
Fitting Low Astigmats with a Soft Toric Contact Lens
Kurt J. Moody, OD,
FAAO, and Sheila Hickson-Curran, MCOptom, FAAO
November 2001
This study discovered that prescribing soft toric lenses to patients with low cylinder resulted in good visual acuity.
The low astigmatic patient (refractive astigmatism of 0.50D to 1.00D) has always been a contact lens prescribing challenge. Soft toric and rigid gas permeable contact lenses have been used extensively on higher astigmatic patients while low astigmats are often a dilemma to eyecare practitioners. Some low astigmats are visually satisfied when corrected with spherical soft contact lenses, whereas others require full cylindrical correction before they are happy. Although spherical soft contact lenses are purported to mask astigmatism, studies have shown that the current generation of soft contact lenses does not mask significant amounts of refractive astigmatism at all. A 1995 study reported that the average amount of astigmatism masked by three different spherical soft contact lenses was, at most, only about a quarter of a diopter.
Until recently, practitioners would choose not to correct a low astigmatic patient with soft toric contact lenses for many reasons. These have included prohibitive cost, additional chair time, poor product reproducibility, comfort inferior to spherical lenses, negligible visual improvement over soft spherical lenses and/or lack of availability of soft toric lenses in a disposable modality.
By not addressing the astigmatic correction of patients desiring soft contact lenses, eyecare practitioners may be denying them their full visual potential. To not include the refractive cylinder in spectacles is unthinkable to most practitioners, but it has been common practice when prescribing soft contact lenses for low astigmats. Now, with the increasing availability of soft toric lens options, there is no reason why practitioners should not choose to correct low astigmats with such lenses.
Acuvue Toric (Vistakon) is a contact lens that is designed to address the historical shortfalls of soft toric lens correction. Due to the availability of a 0.75D cylinder power, Acuvue Toric is designed to provide a viable option for eyecare practitioners faced with a low astigmatic patient who wants soft contact lenses.
In order to evaluate the feasibility of correcting low astigmatic patients with Acuvue Toric, we refit low astigmats who were wearing disposable or frequent replacement soft spherical lenses with the Acuvue Toric. In addition, a second group of low astigmats who habitually wore spectacles was also fit with the lens. The purpose of the study was to compare low astigmatic vision correction options (either spherical disposable/frequent replacement soft contact lenses or spectacles) to the performance of Acuvue Toric in the key areas of ease of fit, vision, comfort, handling and subjective preferences.

Materials and Method
Trial Design. The study was a multi-center trial, conducted at three independent practices in North America. An initial visit was conducted with subjects wearing their habitual disposable/frequent replacement soft contact lenses or spectacle correction. The subjects in the habitual soft contact lens group were evaluated for fit, visual acuity and subjective assessments of vision, handling, orientation (determining inside out) and comfort. For the spectacle-wearing group, only data relating to vision was collected, as handling and comfort were not considered appropriate comparisons for this population. The data generated from these responses were used to compare the performance of the Acuvue Toric test lenses to the subjects' habitual form of vision correction.
Subjects were then trial fit with Acuvue Toric soft contact lenses on both eyes. Subjects who achieved adequate visual acuity (specified in the study protocol as 20/25 or better) and satisfactory lens fit characteristics in both eyes were dispensed the test lenses. The protocol specified that lens rotation of less than or equal to 10 degrees was considered acceptable, if vision and other fit characteristics were also acceptable.
Subjects who were habitual contact lens wearers were instructed to continue use of their preexisting lens care systems and to continue with their usual wear schedule (daily, flexible or extended wear) to best mimic real-life conditions. Previous daily disposable lens wearers wore the study lenses on a two-week daily wear basis. Habitual spectacle wearers wore the lenses on a daily, flexible or extended wear modality as prescribed by their investigator, and were issued any FDA-approved multi-purpose contact lens solution as required for lens care and maintenance. Throughout the study, test lenses worn on an extended wear basis were discarded and replaced after six nights/seven days of wear, and those lenses worn on a daily wear basis were replaced every two weeks. Lenses worn on a flexible basis were replaced after a maximum of two weeks of wear.
Subjects were evaluated at scheduled follow-up visits after two and four weeks of wear. At each follow-up visit, they were questioned regarding the performance of the test lenses, and investigators evaluated fit, visual acuity and subjective ratings. At the two-week visit, after completing the evaluations and questionnaires concerning the lenses worn during the preceding period, new lenses were dispensed to each subject.
Subject Selection To be enrolled in the study, subjects were either habitual wearers of spherical soft frequent replacement or disposable contact lenses, or were habitual spectacle wearers.


Procedures
Objective Measures At the initial visit, visual acuity with each subjects' habitual correction was measured, and a spherocylindrical refraction, slit lamp examination and keratometry readings were recorded. At the two- and four-week visits, visual acuity and slit lamp examination (lens assessment and ocular health) were again recorded.
Subjective Measures At the initial visit, subjective questionnaires were completed grading overall comfort and vision, lens orientation and handling on a scale of 0-50 where 0 = very poor, 8 = poor, 17 = less than satisfactory, 25 = satisfactory, 33 = better than satisfactory, 42 = good and 50 = excellent. Ghosting or shadows, halos around lights, difficulty with glare and fluctuating vision were also graded on a scale of 0 50 where 0 = constant, 13 = frequent, 25 = occasionally, 38 = seldom, and 50 = not at all. For habitual contact lens wearers, all the above listed subjective data were collected. For habitual spectacle wearers, only subjective data relating to vision and visual symptoms were collected. The same subjective questionnaires were also answered at the two- and four-week visits, where subjects rated the study lenses.
In addition, subjects were asked whether they had a preference for Acuvue Toric test lenses or for their habitual vision correction. Habitual soft spherical contact lens wearers were asked for preferences in four categories: comfort, vision, handling and overall preference. Habitual spectacle wearers were asked for preferences in the vision category only.
Results
Subjects A total of 91 subjects were enrolled and 84 completed the study, giving a completion rate of 92 percent. These 84 subjects consisted of approximately one-third (n = 28) habitual spectacle wearers and two-thirds (n = 56) habitual wearers of a variety of disposable and frequent replacement soft spherical contact lenses. These subject proportions were in line with the requirements of the study protocol. Table summarizes subject demographics.
The breakdown of eyes by refractive cylinder was: 0.50D 27 percent, 0.75D 36 percent, 1.00D 37 percent. All 91 enrolled subjects were acceptably fit with Acuvue Toric soft contact lenses and were dispensed with these lenses. However, seven subjects did not complete the study. Two of these subjects were habitual spectacle wearers, one of whom discontinued due to discomfort and disinterest, and the other discontinued due to inadequate vision. Five habitual contact lens wearers did not complete the study: one due to inadequate vision, three due to discomfort with the test lenses and an additional subject stated discomfort and disinterest as reasons for discontinuing the study.
Ease of Fit For all 91 enrolled subjects, the fits achieved with the Acuvue Toric test lenses were considered to be acceptable per the criteria established in the clinical protocol and were judged, by the investigator, to be satisfactory enough to warrant dispensing the lenses. Ninety-six percent (n = 174) of eyes achieved an acceptable fit with the first lens selected, based on refraction. The remaining eight eyes required rotational compensation of the lenses. With the second lens selected, the fit was determined to be acceptable on these eyes.
Objective Findings
Visual Acuity Snellen visual acuity was measured and compared for the study lenses and the subjects' own form of vision correction (either spherical soft contact lens or spectacles). For these comparisons, no effort was made to update or optimize habitual refractive corrections during this study. A total of 153 of the 168 eligible eyes were used to evaluate the results of the study. Ten eyes were not included as five subjects did not wear the study lenses into one of their follow-up visits, and another five eyes were not included because they were corrected for near vision (monovision subjects). The Cochran-Mantel-Haenszel Test was used to statistically compare the subjects' own correction (baseline) to the performance of Acuvue Toric at the two- and four-week follow-up visits.
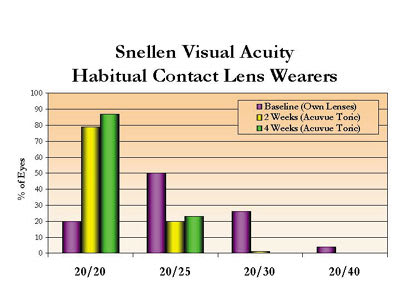
Table 2 summarizes Snellen visual acuity results for the entire subject group and indicates that at baseline, only 35 percent of all eyes achieved 20/20 vision with their habitual correction. At the two- and four-week follow-up visits, 78 percent and 84 percent respectively of eyes corrected with Acuvue Toric lenses achieved 20/20 vision. Acuvue Toric lenses provided a statistically significant (p<0.001) improvement in Snellen visual acuity at both the two and four week study visits, when compared to the subjects' habitual vision correction.
Figure 1 summarizes Snellen visual acuity for the subgroup of habitual spherical soft contact lens wearers. The results show that, of the subjects who habitually wore spherical soft contact lenses, only 21 percent of eyes attained 20/20 vision at baseline with their own lenses. When fit with the Acuvue Toric lens however, this figure jumped to 79 percent at the two-week follow-up visit and was even higher (88 percent) at the four-week follow-up visit. In the spectacle-wearing group, the percentage of eyes that attained 20/20 Snellen visual acuity with their habitual correction at baseline was similar to the percentage achieving 20/20 with the lenses at both the two- and four-week follow-up visits.
These findings confirm that Acuvue Toric contact lenses worn by low astigmatic subjects can often provide better visual acuity than spherical soft contact lenses and similar visual acuity to spectacles.
Visual Symptoms Mean scores attained for visual symptoms such as fluctuating vision, ghosting, glare and halos were calculated. Scores received at each follow-up visit were compared to baseline ratings using the Wilcoxon Signed Rank Test. Considering the subgroup of habitual contact lens wearers only, comparisons of all four visual symptoms were statistically significant (p¾0.001). The results indicate that a statistically significant reduction in all visual symptoms was experienced with Acuvue Toric when compared to the subject's habitual spherical soft contact lens correction. Figure 2 summarizes these findings.
When considering the spectacle-wearing subgroup, no significant difference was noted in visual symptoms of ghosting and glare. However, fluctuating vision was significantly different with this symptom reported more often with the study lenses than the subject's habitual spectacles (p=0.01). The symptom of halos was also noted more often with contact lenses, although this difference was significant only at the four-week follow-up visit.

Subjective Findings
Data for comfort, handling and orientation were available for all subjects previously wearing contact lenses. Vision data was available for all subjects who completed the study and was sub-categorized into either previous spectacle wearers or previous contact lens wearers. The Wilcoxon Signed Rank Test was used for statistical evaluation.
Vision and comfort were both statistically significantly better for the Acuvue Toric contact lenses compared to the subjects' habitual spherical soft contact lenses (p<0.0001 and p<0.03 respectively) at both the two- and four-week follow-up visits. No statistically significant difference was shown for lens handling or orientation.
For the habitual spectacle wearers, no statistical difference was shown between their vision ratings with spectacles at baseline and vision ratings with the Acuvue Toric lenses at the two- and four-week visits. Mean ratings were "good" to "excellent" for spectacles at baseline and Acuvue Toric contact lenses at each follow-up visit.

Subjective Preferences
Figures 3 and 4 summarize key results for subjective preference ratings assessed at the final four-week visit. The data in these figures includes subjects who discontinued from the study, with the assumption that if they discontinued for either poor vision or discomfort reasons, their preference would be for their habitual form of vision correction in these categories. The Sign Test was used to statistically compare the preferences for Acuvue Toric test lenses to the preferences for the subject's habitual method of vision correction.
More habitual contact lens-wearing subjects (Figure 3) preferred the Acuvue Toric lens for vision and overall preference at each follow-up visit, when compared to their own soft spherical contact lenses. In the category of handling, there was no statistically significant preference at either visit, and in the category of comfort, a statistically significant preference was present only at the four-week follow-up visit. More habitual spectacle wearers (Figure 4) stated a preference for the vision provided by Acuvue Toric when compared to their own spectacle correction, but this difference was statistically significant only at the two-week follow-up visit.
Discussion
The purpose of this study was to determine if Acuvue Toric contact lenses would provide visual benefit and preference by low astigmatic patients when compared to their habitual spherical soft contact lenses or spectacles. Key areas of interest included Snellen visual acuity, visual symptoms, subjective assessments, subjective preferences and fit rates.
The study results revealed that Acuvue Toric lenses provided improved visual acuity over habitually-worn spherical contact lens correction and similar acuity to spectacle lens wear. Subjectively, habitual spherical soft contact lens wearers found Acuvue Toric lenses provided superior vision and reduced visual symptoms such as ghosting, halos, fluctuating vision and glare. Such symptoms are often very troublesome to patients but do not necessarily show up in a standard eye examination where the general measure of vision is Snellen visual acuity. However, subjects may attain a good level of visual acuity in the examination room but experience uncomfortable visual disturbances in other conditions such as driving at night, using a computer, etc. The reduction in visual symptoms, accompanied by improved acuity experienced by subjects when fit with Acuvue Toric, is a good indication of the visual improvement this lens provides for low astigmatic subjects.
Historically, soft toric lenses have been less comfortable than their spherical counterparts, primarily due to areas of increased lens thickness and overall bulk required to provide rotational stability on the eye. An interesting finding in this study was that at least one-third of subjects rated Acuvue Toric lenses as providing better comfort than their previous spherical soft contact lens correction.
When asked to make a choice between their own correction and Acuvue Toric lenses, more subjects preferred Acuvue Toric. Further examination of this finding reveals that these preferences were influenced by the amount of refractive astigmatism each subject had. More than 80 percent of subjects who had 1.00D of refractive astigmatism in both eyes stated a preference for Acuvue Toric, but less than half of the subjects who had 0.50D of refractive astigmatism in both eyes chose this option.
The study results reveal that with Acuvue Toric lenses, eyecare practitioners can provide low astigmatic patients with a comfortable contact lens, which combines the convenience of a disposable lens with the vision of a spectacle lens. Based on these results, when a patient presents with low amounts of astigmatism and a desire to wear contact lenses, the Acuvue Toric lens is an excellent choice. CLS
The authors acknowledge the contributions of Elaine Anderson for monitoring the study and of Shawn Meadows for conducting the statistical analysis.
Clinical investigators for this study were: Dr. Kurt J. Moody and Dr. Jay B. Tanner, Kingston, Pennsylvania; Dr. Edward Boshnick, Miami, Florida and Dr. Moe Gross, Toronto, Canada.
This study was organized and funded by Vistakon.
To receive references via fax, call (800) 239-4684 and request document #76. (Have a fax number ready.)





