RGPS AND MYOPIA
Rigid Contact Lenses And Myopia Progression
By Jeffrey J.
Walline, OD, MS
November 2001
This article reviews the findings and flaws of significant research into the effects of RGPs on myopia progression in children.
Myopia is such a common disorder in optometric practice that practitioners often focus on optical correction and fail to consider treatment options that may prevent or slow the progression of myopia. The increasing popularity of refractive surgery illustrates the fact that patients are disturbed by myopia and wish to pursue a cure.
Since 1990, the number of studies regarding myopia funded by the National Eye Institute, a division of the National Institutes of Health, has doubled from 13 to 26. Various treatment options to slow the progression of myopia in children, such as rigid gas permeable (RGP) contact lenses and bifocal spectacles, are currently undergoing more rigorous examination in federally funded studies. New management alternatives for myopia prevention, such as Pirenzepine, (anticholinergic, Valley Forge Pharmaceuticals), are on the horizon.
RGP lenses provide clear, comfortable vision with relatively few ocular health risks and are a standard management option for correcting myopia. While RGPs are used to correct myopia, they may also provide a therapeutic effect and retard the progression of myopia.
Do Rigid Contact Lenses Slow Myopia Progression?
Previous review papers have suggested that rigid contact lenses slow the progression of myopia in children, and several studies have attempted to substantiate this effect.
The first report was by Morrison in 1956. He fitted over 1,000 myopes between the ages of 7 and 19 with polymethylmethacrylate (PMMA) contact lenses and claimed that none of them progressed in myopia after two years. The contact lenses were fitted 1.50D to 2.50D flatter than the flattest keratometry reading, therefore an orthokeratologic effect may have influenced the halt of myopic progression. In 1959, Morrison reported to an audience at the annual American Academy of Optometry meeting that he attempted to fit children with alignment-fitted rigid lenses. He said, "Now and then, an increase in minus is noted, usually slight in amount." Other anecdotal clinical reports with similar results soon followed.
In 1975, Kelly et al reported that only 62 percent of 57 patients younger than 15 years progressed at least 0.25D over a four-year period. Of the 84 spectacle wearers who were examined at 10 years of age and four years later, 73 (85 percent) progressed in myopia. Although a greater proportion of subjects who wore spectacles progressed in myopia, the subjects were not randomly assigned to treatment groups and the contact lens wearers were more likely to have reached the age of cessation for myopia progression during the study.
Stone (1976) fitted 80 children with PMMA contact lenses that were just steeper than the flattest keratometer reading and 40 children with spectacles. She found that the average rate of progression was 0.10D per year for contact lens wearers compared to 0.35D per year for the spectacle wearers. Although axial length was not measured, she concluded that the effects of the contact lenses on the progression of myopia could not be entirely due to corneal flattening and was the first to suggest that contact lenses may influence the axial growth of the eye.
Grosvenor et al (1989) conducted the first study of the effects of rigid--as opposed to PMMA--contact lenses on myopia progression. After three years, the contact lens wearers progressed 0.48D and the spectacle wearers progressed 1.53D, indicating a significant effect of rigid lens wear. Of the original 100 children fitted with rigid contact lenses, only 56 were able to complete the three-year study and corneal curvature and axial length were not available for the control group of single vision spectacle wearers. Although valid ocular component comparisons using the three-year data were not available, the two-year data illustrate the potential effects of rigid lens wear on axial elongation of the eye.
A rigid contact lens myopia control study was recently conducted in Singapore by Khoo et al (1999). Subjects were randomly assigned to wear rigid contact lenses or spectacles. Some 105 children were fitted with rigid lenses, but only 45 children (42.9 percent) wore their lenses regularly through the end of the study. After three years, the spectacle wearers progressed an average of 0.78D per year and the contact lens wearers progressed 0.42D per year, a clinically and statistically significant difference. The investigators measured the axial length and found a significant difference in annual axial growth between the contact lens wearers (0.22mm) and the spectacle wearers (0.31mm). Previous hypotheses regarding slowed axial growth in rigid contact lens wearers were finally validated. However, the significance of this study's conclusions are limited because the study suffers from differential loss to follow-up and incomplete ocular component measurement.
The largest study that failed to find an effect of RGPs on myopia progression was conducted by Baldwin (1969). A group of 7- to 13-year-old myopic children were fitted with rigid lenses or spectacles and followed for slightly less than one year. The mean rate of myopia progression extrapolated to one year was 0.53D for the RGP wearers and 0.45D for the spectacle wearers. The study may have failed to find a positive effect for rigid lenses because the subjects were followed for less than one year and because the patients were not randomly assigned to treatment groups. The patients chose the treatment best suited to their needs, so the rigid lens group initially had more females, greater myopia, steeper corneas and longer axial lengths. These factors are related to higher amounts of myopia and/or greater progression of myopia, so the RGP group would be expected to experience a greater change in myopia.
Why Can't We Say Rigid Contact Lenses Slow Myopia Progression?
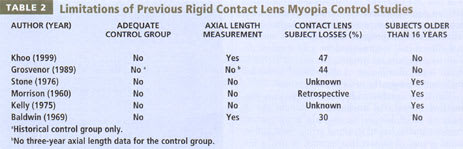
Many previous studies have shown that rigid lenses slow the annual progression of myopia (Table 1). Three of the four studies show that rigid contact lenses slow the progression of myopia by about 50 percent. However, all of the studies failed to provide proper attention to important confounding variables (Table 2). While earlier work produced intriguing results for scientists and clinicians, they contain many problems that challenge the significance of the studies' findings. The faults of the previous studies can be summarized in four categories: differential loss to follow-up; inadequate control group; incomplete ocular component measurements; and inadequate or poorly-selected entry criteria.

Differential loss to follow-up Many RGP lens myopia control studies have suffered from differential loss to follow-up. For the vast majority of people, adaptation to the initial discomfort of rigid contact lenses is more difficult than adjusting to spectacle wear. Many subjects drop out of the rigid contact lens group due to an inability to adapt to rigid lenses. The absence of data from these subjects compromises the validity of the results. For example, the inability to adapt to RGP lenses may be associated with a higher rate of myopia progression. Eliminating subjects who were not able to adapt to rigid lenses would then also eliminate subjects whose myopia progresses faster, resulting in a false impression that rigid lenses slow the progression of myopia. These subjects, lost to follow-up, have an impact on the implications of study results.
Inadequate control group In order to make valid conclusions regarding the effect of rigid contact lenses on myopia progression in children, two treatments should be compared. These treatment groups must be equal with respect to known and unknown confounding variables that may alter myopia progression. For example, the two treatment groups must have an equal distribution of initial refractive error because you would expect a group with higher initial refractive error to progress more rapidly. A randomized clinical trial is considered the gold standard design to compare treatments because it helps to ensure equal distribution of all potential confounding factors between the two treatment groups.
The study conducted by Khoo is the only randomized clinical trial conducted to examine the effects of RGP lenses on myopia progression. Previous studies lacked a control group, used self-selected groups of contact lens wearers, or used a historical control group. Although the study conducted by Khoo has been the only randomized clinical trial, the differential loss to follow-up mitigates the effects of randomization. The study by Grosvenor et al used a historical control group of single vision spectacle wearers participating in a bifocal myopia control study. Matching the spectacle wearers to the contact lens subjects based on age, gender and initial refractive error limited the number of control subjects, and complete ocular data were not available for the control subjects after three years. The lack of an adequate control group makes comparisons difficult, thereby reducing the impact of the conclusions.
Incomplete ocular component measurements Positive results in many studies fail to exclude alternate possibilities which may explain the effect. For example, both the Houston Contact Lens Myopia Control Study and Stone's study found that RGPs slow the progression of myopia and that corneal flattening measured by keratometry does not explain all of the effect. However, neither study was able to definitively identify other mechanisms that may retard myopia advancement. They hypothesized that slowed axial growth may explain part of the treatment effect, but did not rule out a change of the central corneal curvature that was not measured by keratometry. Thorough measurements of the ocular components in a controlled trial will allow better understanding of the effects of rigid contact lenses on myopia progression.
Poorly-selected entry criteria Inadequate or poorly-selected entry criteria may also affect the results of the study. Goss and Winkler (1983) showed that myopic children tend to progress in myopia until age 15 years for females and age 16 years for males. Previous studies have included subjects who may be expected to cease myopic progression, which limits the ability to detect a potential treatment effect. None of the studies limited the participants to subjects who were able to adapt to rigid contact lens wear, therefore leading to differential loss to follow-up. Generalizability to a large population is not affected by eliminating children who cannot adapt to rigid lenses because only children who can adapt to rigid lenses are able to benefit from the potential treatment effect. Choosing appropriate entry criteria for a study is critical to the validity significance, and generalizability of the conclusions.
While we have anecdotal evidence and clinical results demonstrating that rigid contact lenses slow myopia progression in children, problems with these previous studies limit the significance of their outcomes.
Should All Myopic Children Be Fitted With RGP Contact Lenses?
Given the limitations of previous rigid lens myopia control studies, a thorough explanation of the treatment options available for myopic children should be discussed with the parents. The practitioner should have knowledge about the potential treatment effect of the various modalities, as well as financial considerations and possible side effects. RGPs may impact myopia progression by approximately 50 percent, but we don't know which individuals will benefit the most, and we don't know if the effects are permanent. Rigid contact lenses are cosmetically appealing for myopic children, and they provide excellent vision with few side effects. Approximately 80 percent of 8- to 11-year-old children are able to adapt to rigid lenses, but they may not be the most appropriate option for children who plan to wear contact lenses only occasionally. Educate the parents of all your young, myopic patients about the visual advantages and the potential benefits of myopia control offered by RGPs to help them make the appropriate treatment decision for their children.
To receive references via fax, call (800) 239-4684 and request document #76. (Have a fax number ready.)




