BITORIC FITTING GUIDE
Putting a Bitoric RGP Lens Fitting Guide to The Test
By Kirby Pitts,
OD, Latricia Pack, OD,
William Edmondson, OD, FAAO, Charles E. Pack II, M.S.
October 2001
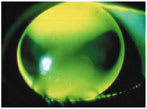
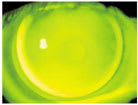
Some practitioners find fitting bitoric rigid gas permeable (RGP) contact lenses both time-consuming and difficult. Bitoric lenses, however, are indicated for certain patients to obtain acceptable lens fit and performance. Bitoric candidates possess a high amount of corneal cylinder, which necessitates a toric back surface. Mandell suggests using a bitoric lens when a spherical lens exhibits decentration, excessive movement or an unacceptable fluorescein pattern (Figures 1 and 2).
|
|
|
|
Figure 1. Spherical lens on toric cornea. |
|
The astigmatic refractive error and corneal toricity are the key components in determining the most appropriate lens design for a patient, but opinions vary as to how much corneal toricity necessitates a bitoric RGP lens. Mandell recommends that you use a toric base curve to maintain lens stability on the eye when corneal toricity reaches 2.00D. Bennett notes that a bitoric lens is essential when there is regular astigmatism of greater than or equal to 3.00D corneal toricity. In assessing the stability of an RGP lens, Edrington, Stewart and Woodfield reported that lens rotation is minimized when the ratio of lens toricity to corneal toricity of with-the-rule astigmatism is between two-thirds and one. For a patient with 3.00D of corneal toricity, the most stable RGP lens will have between 2.00D and 3.00D of base curve toricity.
|
|
|
|
Figure 2. Bitoric lens on toric
cornea. |
Fitting Guides vs. Optical Cross Calculations
Many guidelines and philosophies for fitting bitoric RGP lenses base the relation of the corneal toricity and RGP base curves on the perceived ideal spherical lens fit. This ideal spherical lens fit occurs on a cornea with approximately 0.75D of with-the-rule corneal toricity. Fitting the lens slightly flat to alignment in the flat meridian allows for tear pumping in the space of the steeper meridian. In addition, the 0.75D difference in curvature prevents undue bearing on the cornea. A good bitoric lens design uses a similar relationship in the base curve radii to promote the tear exchange in the steeper meridian without unwanted mechanical bearing.
While several guidelines exist to help determine base curve radii for bitoric RGP lenses, the one created by Mel Remba became one of the most commonly utilized guides through the 1970s and 1980s. Using keratometer readings, a practitioner can use Remba's table to select the base curves for a bitoric lens (Table 1). The recommended radii are flatter in both meridians to prevent a tight fit. The overall corneal toricity, which is easily read off the table, determines the amount of flattening in each meridian. The power in each meridian, however, you must calculate separately.
Using the principles employed when fitting an ideal spherical RGP lens, some practitioners prefer to use an optical cross calculation method to determine bitoric lens parameters. You can calculate each meridian as a separate, spherical lens, with the flatter meridian corresponding to the more plus power. Make specified base curve modifications to allow for tear exchange. Opinions of contact lens professionals vary on the perfect amount of change (flattening or steepening) in each meridian. As you alter the base curve radii, you must modify the powers to compensate for induced lacrimal lens effects. For example, if you deem the flat meridian to be 0.50D flatter than K, make the power in that meridian 0.50D more plus to compensate for the tear lens induced (SAM-FAP). You must, of course, apply this philosophy to each meridian in determining all final bitoric contact lens parameters.
The Mandell-Moore Guide
Most of these fitting guides or optical cross calculations provide a good starting point for patient lenses. Problems arise when a practitioner attempts to design a lens between patient examinations in a busy office. It is easy to overlook a step or make a simple arithmetic error, such as subtracting a tear lens power instead of adding it. Robert Mandell, OD, and Carl Moore of Con-Cise Contact Lens Company published a method for determining the parameters of a bitoric RGP contact lens by using the patient's spectacle refraction and keratometry readings. They developed the Mandell-Moore Bitoric Lens Guide to minimize the risk of errors while performing tear layer calculations that determine base curve radii and powers for a bitoric lens.
The Mandell-Moore Bitoric Lens Guide resembles the optical cross method in that it treats each meridian as a separate RGP lens. The guide, however, has a specified fitting relationship between the steep and flat meridia based on the amount of corneal cylinder present. Labeled as the "fit factor" on the guide, this relationship maintains the "ideal" spherical lens-cornea relationship. Mandell and Moore also incorporated the necessary power changes in their guide to compensate for the lacrimal lens effects induced by the base curve changes. A vertex distance correction table also included on the guide allows quick conversion of power to the contact lens plane. Practitioners have widely used this self-contained guide because they can quickly and easily determine the fit of the base curves and the resultant powers with minimum error.
Practitioners are becoming busier than ever; we must search for opportunities which allow us to save chair time while still minimizing errors involved in treating our patients. The Mandell-Moore RGP Bitoric Lens Guide can alleviate the need for complicated calculations of base curves and respective powers before empirically ordering lenses. This does save the practitioner time, but how closely does the guide predict the parameters of a successful fit?
Testing the Mandell-Moore Method
We selected records of 33 successful bitoric RGP lens wearers at the Northeastern State University College of Optometry Contact Lens Clinic for review. There were 24 females and nine males included in the research (61 eyes total) with ages ranging from 6 to 53 years old. We defined success as a clinically acceptable fluorescein pattern and a visual acuity within one line of the patient's best-corrected visual acuity with spectacles. We excluded patients with ocular disease, monovision correction or corneal cylinder greater than 5.50D (due to corneal cylinder amounts included in the Mandell-Moore fit factor). For those with a corneal cylinder of < 2.00D, we used the 2.00D fit factor for calculations.
We acquired the spectacle prescription and keratometric values used in the Mandell-Moore calculations from the clinical records at the time of fitting the lenses. All lenses in the study had been made in the Polycon II SPE/CPE design or a similar generic design. A slight majority of the lens diameters (38 of 61) were 9.0mm, but the lenses ranged from 9.0mm to 9.6mm. We calculated the base curves and powers for each meridian using the Mandell-Moore RGP Bitoric Lens Guide. We then compared these results to the base curves and powers of the actual RGP bitoric lenses prescribed and successfully worn.
Results
We conducted four paired t-tests on 61 eyes to determine whether the Mandell-Moore RGP Bitoric Lens Guide accurately predicts the contact lens base curves and powers of RGP lenses currently worn successfully in our clinic. The four tests compared the calculated power and base curve radius (BCR) to actual power and BCR for both the steep and flat meridians. We set the probability of a Type I error at 0.10 for these two-tailed tests.
First, we compared the calculated BCR to the actual BCR for the flat meridian. We found a statistically significant difference of 0.183D steeper.
Second, we compared the calculated BCR to the actual BCR for the steep meridian. This test showed no statistically significant differences.
Third, we compared the calculated power to the actual power for the flat meridian. This test showed no statistically significant differences.
Fourth, we compared the calculated power to the actual power for the steep meridian. We found a statistically significant difference of 0.297D more plus.
We did not consider the statistically significant differences listed above as clinically significant since both are within 0.37D.
Discussion
The original Mandell-Moore article explained their concept of the "ideal fit" RGP lens which they incorporated into their fitting guide for bitoric lenses. They note that when a spherical lens is fit on flat K, 0.50D to 0.75D of corneal toricity is ideal in providing good tear exchange behind the lens. This same fitting relationship also works well when fitting a bitoric lens.
Mandell and Moore did not recommend a specific overall lens diameter when they developed their bitoric lens guide; therefore, our data was not diameter-specific. Mandell has indicated that lens parameters depend upon usual considerations, but most importantly you should consider keeping the lens diameter small enough to prevent the lids from inhibiting rotation so that the lens will not orient on the axis of the toricity. Make lenses closer to 9.0mm than 9.5mm in diameter. Moore reports that the average diameter Con-Cise currently uses for bitoric RGP lenses is in the 9.2mm range.
Since this article, originally published in 1988, the Mandell-Moore guide has changed slightly. The guide now does not go flatter than 0.75D in the steep meridian. According to Moore: "We continued to respond to experience and found if we went much flatter than 0.75D in the steep meridian, there was too much standoff at the six o'clock position." Pads with the revised fit factor guidelines added to the Mandell-Moore guide are available from the RGPLI and the CLMA.
Our study indicates that the Mandell-Moore guide provides an accurate way of selecting an initial, and likely successful, bitoric lens. It proved to be an excellent clinical predictor of final RGP bitoric lens parameters for our clinical population. Furthermore, the guide is easy to use, time-efficient and eliminates most common arithmetic errors.
References are available upon request.. To receive references via fax, call (800) 239-4684 and request document #75. (Have a fax number ready.)

|
TABLE 1Remba's Table for Selecting Base Curves for a Back Surface Toric Lens |
||
| CORNEAL ASTIGMATISM |
FLAT MERIDIAN |
STEEP MERIDIAN |
| 2.00D | Fit 0.25D flat | Fit 0.25D flat |
| 3.00D | Fit 0.25D flat | Fit 0.50D flat |
| 4.00D | Fit 0.25D flat | Fit 0.75D flat |
| 5.00D | Fit 0.50D flat | Fit 0.75D flat |