IRREGULAR CORNEAS
Fitting Challenging Corneas
By Shelley I. Cutler, OD,
FAAO
September 2001
Learn your options for fitting irregular corneas altered by disease, trauma or surgery.
The normal human cornea generally has a prolate configuration. It is steepest in the center and progressively flattens toward the periphery. Some corneal mapping systems estimate an eccentricity factor, or "E" value. A toric cornea is a normal variation.
When disease, trauma or surgery alters the corneal shape, fitting these corneas becomes a challenge for even the most experienced contact lens practitioners. If the change to the cornea is a minor one, spectacles or soft toric contact lenses may satisfy the patient's visual needs. However, many times there is a significant amount of corneal irregularity that does not allow acceptable vision through spectacles or soft contact lenses. Only rigid lenses will allow the patient to visually function once more.
Many times a standard design rigid gas permeable contact lens will not work. You may need creativity and knowledge of the many patented, trademarked and other proprietary designs available to help you fit these patients successfully. Occasionally, a piggyback or scleral design will be the only option.
Corneal topography can guide contact lens fitters to the most practical starting point, but it's just a starting point. You need to place a contact lens on the eye. Only then can you make alterations in design. Although each cornea presents the practitioner with a unique situation, there are some generalities to guide you in a specific direction.
Fluorescein patterns reflect the many peaks and valleys that can occur with altered topography. You must try to distribute the weight-bearing forces of the contact lens as evenly as possible. Sometimes this can be most difficult. Let the fluorescein pattern be your guide. Is the bearing light, with good tear flushing underneath, or is it too heavy and will it cause some epithelial disruption later on? Many times there is a fine line between the two, and only time will reveal the answer. A successful contact lens fit allows the patient to wear the lens for as many hours as desired, maximizes vision and, most important, keeps the corneal integrity intact.
Corneal Ectasias
Keratoconus and pellucid marginal degeneration (PMD) are progressive corneal thinning disorders. They both cause a thinned protrusion with irregular astigmatism.
|
|
|
|
Figure 1. Oval or sagging cone. The steepest dioptric
portion of the cone is larger in shape, more decentered and inferior in location |
|
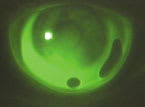
Keratoconus. The thinned protrusion in keratoconus is usually slightly decentered off the visual axis. Historically there were two basic keratoconic patterns: the nipple cone (the steepest dioptric value is smaller in shape and somewhat more central in location) and the oval or sagging cone (the steepest dioptric portion of the cone is larger in area and the position is more inferior and decentered) (Figure 1). Corneal topography has revealed to us that there are many variations, and the description may not fall into either category. Because of the variations in size and depth of a cone, one trial set may not necessarily work for all keratoconus patients. Figure 2 shows the contact lens fit of the patient with the large sagging cone in Figure 1.
|
|
|
|
Figure 2. Contact lens fit on the larger, sagging cone shown in Figure
1. |
You need several trial sets and a yellow filter (for enhanced fluorescein analysis) to fit keratoconus. Some experts in the field, such as Ed Bennett, OD, MSEd, and Dennis Burger, OD, have designed their own sets of tri- and quad-curve RGP lenses. The trial set that the Collaborative Longitudinal Evaluation of Keratoconus (CLEK) study presently uses is another popular set.
Choosing an initial trial lens can vary depending on the contact lens fitter's philosophy. The CLEK trial set estimates the apical curvature by finding the first lens that vaults the corneal apex. This first definite apical clearance lens (FDACL) is often near the steep K value. Some fitters suggest that you choose a base curve that is the average of the two keratometric or Sim K (topography) values, evaluate the lens and make changes from there.
In my opinion, a well-fitting lens will demonstrate a light kissing touch centrally surrounded by a ring of clearance (pooling), mid peripheral alignment and adequate edge lift for tear exchange. Many times when this occurs, the optic zone and base curve radius are very close in value (mm) to each other. Depending on the size of the cone, you may need to make the optic zone larger and flatter or smaller and steeper to house the cone appropriately.
Besides a standard RGP design, a multitude of proprietary lenses are now available to fit the keratoconic patient. If using a proprietary set, follow the fitting guide and strive for the ideal fluorescein pattern. Some of these proprietary lenses include the Rose K, ComfortKone, Nicone, Soper Cone, McGuire lens and others. More recently available is Specialty UltraVision's Epicon lens, a larger diameter, semi-scleral lens made from carbosilfocon material.
|
|
|
|
Figure 3. Typical corneal topography of pellucid marginal degeneration
(PMD). |
|
Pellucid marginal degeneration. PMD has a classic topographical pattern sometimes described as a mustache, claw or two kissing birds (Figure 3). There is against-the-rule astigmatism, and the thinned protrusion is usually much more inferior than keratoconus. Many times these patients are misdiagnosed as keratoconic. If spectacles or soft toric lenses no longer provide good vision, try a high-riding sphere to fit the normal superior cornea. On occasion, a smaller bitoric design, fit centrally, may be successful (Figure 4).
Traumatic Injury
|
|
|
|
Figure 4. An intrapalpebral bitoric RGP fit on a cornea with
PMD. (Courtesy of Joel Silbert, OD) |
Severe traumatic injuries can happen at any age. If the injury is penetrating, not only does the cornea require immediate repair, many times cataract or transplantation surgery follows in the near future. These patients are emotionally worn out by the time they appear in your office for visual rehabilitation. They want success immediately and can be in for disappointment if you do not initially discuss realistic expectations with them. If you are lucky, the first lens you order after an initial diagnostic fitting may be successful. Most often, though, it will take several attempts to refine the fit.
Because each injury and contact lens design will be different, keep different trial sets to facilitate success. You could try spherical rigid lenses of varying diameters and a 2.00D or 3.00D bitoric trial lens set. Corneal topography will provide knowledge of the resulting shape to facilitate a starting point.
If the patient needs cataract extraction, occasionally the surgeon may choose to leave the patient aphakic. Keep in mind that these thicker lenses don't always behave like a trial lens of plano or minus power. Large flatter lenses that attempt to vault the area of injury are usually a good starting point. If there is too much toricity, try a back or bitoric design.
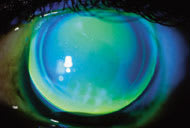
Case Example 1. A 15-year-old female sustained a penetrating injury OS that required cataract extraction. I fit her with a large keratoconic lens design (Nicone #2) in aphakic power. Figure 5 reveals the massive sutured scar. Figure 6 shows the fluorescein pattern.

|
|
| Figure 5. Penetrating injury with aphakic contact lens in place. Note the large scar of the sutured cornea. |
Figure 6. Fluorescein pattern of a lens fit on the cornea shown in Figure 5.
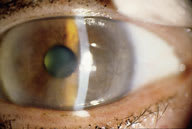
Case Example 2. An 85-year-old-female sustained chemical injury as a young woman while imprisoned in a Nazi camp during WWII. She was unable to rinse her eyes, so the chemical contact was sustained for days (Figure 7). Acuity with glasses was OD 20/100 OS 20/80. There were early lenticular changes present, as well. She kept PMMA lenses from many years ago that improved her vision but hurt her eyes. She wished to be refit so she could read music and play the piano. VA with her present 20-year-old PMMA lenses: OD 20/80, OS 20/40. I refit her in RGP lenses (Figure 8), which were able to distribute the weight-bearing forces more evenly. Increased edge lift aided in tear circulation. The patient was able to achieve eight to 10 hours a day of comfortable wearing time, which just thrilled her. Final VA was OD 20/80, OS 20/30-.
|

|
| Figure 7. Illustration of a chemical injury, OS, in an 85-year-old female. |
Figure 8. RGP lens of patient, OS in Figure 7.
Penetrating Keratoplasty (PK)
Corneal transplantation allows surgeons to replace diseased corneal tissue with healthy tissue from a donor. The number of patients that need only spectacle correction after undergoing PK is higher than ever. There is, however, still a small percent of transplanted corneas that will not achieve an optimum result. Many factors can cause this, including the physiology of donor cornea, existing host corneal disease and/or neovascularization (pre or post surgery) and tear film abnormalities. Some form of rigid contact lens can maximize vision for these patients.
A corneal lens would be the optimal choice. Experience has shown us that larger, flatter lenses that vault the host/graft junction, with minimal bearing elsewhere, show the most overall success. There are a few proprietary designs specifically for this type of cornea, including the Post PK by Lens Dynamics and Infinity Optical's PSC.
Evaluating post-PK topography. The resulting corneal topography following PK can fall into a variety of categories, depending on the individual healing factors of the patient and the surgeon's technique. Some corneas maintain their basic prolate shape, while others exhibit a reverse, oblate configuration. You may see regular astigmatism either with the rule or against the rule. Sometimes there is mixed astigmatism or mixed irregular astigmatism. The most difficult shape to fit is a cornea that is steep on one half and progressively flattens to the other half.
Use a topographical map prior to contact lens fitting to significantly reduce the time in determining an initial lens order. Although some fitters advocate always beginning with a large flat spherical lens, some contact lens designs are more conducive for specific shapes. For example, if the corneal topography reveals an oblate configuration, a reverse geometry lens such as the PK Bridge (Conforma), NRK (Lancaster), Plateau lens (Menicon) or one of the many OK lenses (Contex) might be a good starting point. A bitoric design is best for high regular astigmatism. If the lens appears to release from the upper eyelid and drift toward a steeper part of the cornea, consider incorporating a minus lenticular edge to increase superior lid grab.
If you cannot obtain a topographical map, try starting with a large diameter lens (9.8mm to 11.0mm) with a base curve halfway between the two main meridians. Fluorescein analysis is imperative. If there are areas of excessive bearing, attempt to vault them. There will be times that you may have to accept more edge lift than with a routine RGP fit.
On occasion, many attempts with different designs will indicate that a corneal lens is not possible. Other alternatives include soft lenses, piggyback fits (soft lenses in combination with rigid corneal lenses), scleral RGPs, the Epicon lens and hybrid (Softperm) lenses.
Case Example A. A 78-year-old male needed a contact lens post-PK, OD. Refraction was a fuzzy 20/70 with +2.50 6.50 x 80. Figure 9 shows his corneal topography. I initially tried a few large diameter spherical lenses, but the positioning and fluorescein patterns were unacceptable. All of the lenses decentered temporally. The highest toricity trial lens with a toric base curve I had was a 3.00D spherical power effect (SPE) lens. When I placed this on the eye, it was clear that I would need more toricity in the base curve. The final lens design had 4.00D of base curve toricity and yielded a final acuity of 20/25. (Figure 10)
|
|
|
|
Figure 9. Topography post PK with high against-the-rule (ATR) astigmatism. |
Figure 10. Final lens for patient in Figure 9. |
Case Example B. A 73-year-old female was referred to me to see if a contact lens was possible on her transplanted eye as opposed to sending her to a refractive surgeon for LASIK. Visual acuity with pinhole was 20/300, and refraction was extremely difficult. Since I would eventually place a contact lens on the eye, there was no real reason to attempt a low vision refraction. Corneal topography revealed about 13.50D of corneal cylinder (Figure 11).
I attempted a few corneal lenses with large amounts of toricity (8.00D), but they would not center. I eventually fit the patient with the Macrolens, a semi-scleral lens from C & H Labs. Visual acuity was 20/40. After many months of successful lens wear, I noted some epithelial breakdown centrally within the graft. Visual acuity was also slightly reduced to 20/50. I refit her with the Epicon lens to see if the corneal health would improve (Figure 12), which it did. Vision also returned to 20/40+.
|
|
|
|
Figure 11. Topography post PK with high with-the-rule (WTR) astigmatism. |
Figure 12. Cornea from Case Example B fit with the Epicon lens. Even with the steeper peripheral curve, there is still clearance (and bubbles) in the far periphery. |
Post-Refractive Surgery
When refractive surgery causes an irregular cornea and decreased acuity, rigid lenses are usually the only choice. Because the majority of patients who seek this procedure are myopic, the resulting corneal shape is oblate-like. The major challenge in fitting these corneas is centering a lens with no excessive bearing or pooling. You need larger diameters to accomplish this.
Radial keratotomy (RK). For post-RK corneas, standard lens designs tend to not center. These lenses drift over to the steepest part of the cornea known as the "knee" (the steepened transition area from the central to mid peripheral cornea). Many times, if the lens is steep enough to center on the cornea, too much clearance in the central area of the cornea causes trapped air bubbles, tear stagnation and edema.
Reverse geometry lenses can address this. Using the post-surgical topography, make the initial base curve of a reverse geometry lens slightly steeper than the central readings. Using the second or third ring is a good starting point. If you don't have a map, choose an initial base curve 1.00D to 2.00D steeper than the flatter K reading. As always, use the fluorescein pattern to guide you in adjusting the optic zone, base curve, reverse curve and peripheral curve values. Chances are, even with the best fitting lens, the fluorescein pattern will reveal central clearance or pooling. Make sure that it is not excessive. If you see alignment through the intermediate area and adequate edge lift, the patient will most likely be fine.
Case Example. A 43-year-old male presented with unstable vision 18 years after his RK procedure. His original procedure resulted in eight incisions OU. Several years later he underwent enhancement in both eyes. A few years later, the OD was enhanced once more.
Entering acuities with his present glasses were OD 20/30, OS 20/40. Refraction yielded 20/30 OD, OS. Since he is a pilot, he wished to be fit with RGPs for stable, consistent vision. Topography OS revealed a typical oblate-like pattern.
The final lenses, which he has worn successfully for three years, were the OK-4 lens by Contex. Fluorescein pattern revealed a near-alignment pattern centrally that changes to minimal clearance at the end of the flattened central area. You see alignment mid-peripherally with good edge lift. The lens positions superiorly under the eyelid and exhibits excellent tear exchange on the blink.
LASIK. Most LASIK procedures result in a smooth corneal surface. When this is not the case, and spectacles or soft lenses are not an option, RGPs are the lens of choice.
The transition area of a post-LASIK cornea is less dramatic than that of a post-RK cornea. Initially stay away from reverse geometry lenses and instead try large diameter, smaller optic zone RGPs with standard peripheral curves.
Do not choose the initial base curve radius from post-surgical keratometry or Sim K values. This will result in an exceptionally flat lens with lots of edge lift. Other practitioners suggest choosing the base curve by subtracting approximately one-third of the refractive error reduction from the pre-operative flat keratometric value (For example, pre-op Ks are 44.50 @ 180 / 45.75 @ 90: Myopia reduction 3.00: 44.50 1/3 [3.0] = 43.50 or 7.76mm as the initial base curve). Once the lens is on the eye, make adjustments according to fluorescein analysis.
Final Thoughts
When addressing such difficult cases, keep in mind that these corneas are attached to human beings. Patients who are confronted with the fact that they have a corneal disease or a less than perfect surgical result experience many feelings and emotions. Whatever the cause, the integrity of their eye has been changed forever. They may have fear, depression, anger and/or frustration, and they may vent it at you. If you can help these patients return to their daily activities as productive human beings, you will gain loyal patients for life.
References are available upon request to the editors of Contact Lens Spectrum. To receive references via fax, call (800) 239-4684 and request document #74. (Have a fax number ready.)