TOPOGRAPHY AND ORTHO-K
Corneal Topography and Orthokeratology: Pre-fitting Evaluation
Corneal topography accurately analyzes the pre-fitting cornea of an
orthokeratology patient.
By John Mountford, Dip. App. Sc,
FAAO, FCLSA, Patrick J. Caroline, FCLSA, FAAO, and Don Noack, Dip Opt (WA)
Our concepts of corneal shape and how it affects contact lens fitting have changed since the introduction of computerized corneal topography (CCT). Similarly, the development of reverse geometry contact lenses has dramatically changed the way we currently view the practice of orthokeratology.
Orthokeratology involves modifying corneal contour, so it stands to reason that an instrument that was specifically designed to map corneal contour should play an important role in expanding our understanding of the procedure. Uses for CCT in the contemporary orthokeratology practice can be divided into two categories:
Pre-fitting Topographical Analysis:
- Screening for pathologic corneas
- Establishing the baseline corneal shape
- Predicting the outcome based on the pre-fitting apical radius and corneal eccentricity.
- Accurate shape analysis to assist in selecting optimum lens parameters
Post-fitting Topographical Analysis:
- Identifying and documenting induced corneal changes
- Assisting with problem solving and lens design refinements
- Patient education
In this article we will review the important role of initial topographical analysis. In Part Two, we will discuss post fitting topographical assessment and its role in patient management and problem solving.
|
|
|
|
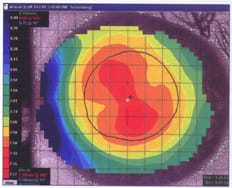
Figure 1. Subtractive map, upper left is the pre-fitting map, lower left is the post-fitting map and the right center, the subtractive or difference map. The pre-fit Rx was 4.00 0.50 x 140, post-fit +0.50 0.25 x 160, difference 4.50D. |
|
Pre-Fitting Topographical Analysis
Screening for Pathology As with pre-screening for refractive surgery, initial topographical analysis allows you to detect corneal anomalies such as irregular corneal astigmatism, keratoconus and pellucid marginal degeneration. These conditions are totally contraindicated for orthokeratology, and you must properly identify them and advise the patient that the treatment would not be suitable in his case. Also individuals with limbus-to-limbus astigmatism may not respond as well to orthokeratology, so that also must be diagnosed and the patient advised of his unsuitability.
Baseline Corneal Shape and Predicting Outcomes One of the most important functions of pre-fitting CCT is to provide a baseline corneal shape from which to compare subsequent topographical changes. Baseline corneal shape is best visualized by the subtractive map function (Figure 1), a common feature in all currently available topography instruments.
Apical Radius Since orthokeratology results in a flattening affect at the corneal apex, it is important to differentiate the apical radius of curvature from the flat K measurement. Normally on a symmetrical cornea the apical radius is the radius of the highest point on the cornea. This point is usually located near the geometric center of the cornea, but its location can also vary dramatically. It is usually 0.50D to 1.00D steeper than the flat K reading, depending on the actual corneal eccentricity and the degree of corneal astigmatism. Figure 2 shows a pre-fit axial curvature map. The apical radius (Ro) value (shown in the lower right hand window) illustrates a radius of curvature of 7.40mm (45.75 diopters) 0.01mm from center. The flat K (shown in the lower left hand window) is 1.00D flatter or 7.54mm (44.75 diopters). The flat K will equal the apical radius only if the eccentricity of the cornea is zero. Apical radius or its invert, apical corneal power, represents the point of greatest refractive change. Previous studies (Ericson and Thorn 1977; Mountford 1997) have shown that there can be a refractive change of 0.75D before any change in keratometric readings is noted.
|
|
|
|
Figure 2.
Normal pre-fitting topographical map with an apical radius of 7.39mm, 45.75 diopters. and a flat K of 7.55mm, 44.75
diopters. |
Corneal Eccentricity A major pre-fitting CCT objective is to determine the degree of corneal eccentricity. Eccentricity has proven to be a valid predictor of refractive change, in that the greater the eccentricity, the greater the predicted change (Mountford 1997, El Hage et al 1999). A further refinement of this trend, which linked apical radius, eccentricity and lammellar fiber length, also showed a high predictability for the refractive change possible (Mountford and Noack 1998).
Shape Analysis The pre-fitting corneal mapping provides valuable shape data that helps determine the optimum lens parameters required to achieve the desired effect. Lens fitting using CCT provides a degree of accuracy that is simply not possible with the keratometer or fluorescein pattern interpretation of diagnostic lenses.
Calculating Sagittal Height
The most accurate and reproducible technique for fitting reverse geometry is often called the sagittal height technique. Put simply, the formula is:
Lens Sagittal Height = Corneal Sagittal Height + Apical Tear Film Thickness
Today, specially designed software calculates the sagittal height of the cornea and tear film over an area equal to that covered by the fitting portion of the contact lens. For example, for the tear film profile of a 10.6mm reverse geometry lens, the area that makes up fitting portion of this lens includes the following:
| Optical zone diameter (BOZD) | 6.0mm |
| Width of the reverse curve | 1.2mm |
| Width of alignment curve 1 | 1.5mm |
| Width of alignment curve 2 | 1.5mm |
| Total fitting chord area | 10.2mm |
Therefore, we need to calculate the sagittal height of the cornea (over a chord of 10.2mm). We entered the following corneal data into the ortho-k software:
| Apical radius of curvature | 7.70mm D |
| Corneal eccentricity | 0.50 E. |
| Desired apical tear layer thickness | 5 microns |
The total sagittal height of the above cornea over a chord of 10.2mm=1.86mm. Therefore, if an allowance of 0.05 microns is made for apical clearance, the total sagittal height of the lens at a chord of 10.2mm = 1.91mm.
|
|
|
|
Figure 3. Sagittal height profile of a 10.6mm reverse geometry. The fitting portion of the lens includes the optical zone diameter, as well as the area covered by the reverse and alignment curves. The optimum clearance factors are
shown. |
|
Corneal Shape and Reverse Geometry Lens Designs
In the design and fitting of modern reverse geometry lenses, it is critical to establish an appropriate fitting relationship in the area of the mid-peripheral cornea. The lens should incorporate a curve or angle specifically designed to align "lock" the lens into position mid-peripherally along the horizontal corneal meridian. This alignment zone is the single parameter that ultimately dictates the centering and movement characteristics of the lens. In contemporary reverse geometry lens designs, this parameter may be a spherical radius, an aspheric radius or a tangent angle (straight line).
Modern corneal mapping techniques can provide valuable insights into the degree of flattening in the mid-peripheral cornea. While it is true that most videokeratography systems map only the center 7.0mm to 8.0mm of the cornea, clinical experience has shown that extrapolated data beyond this region is surprisingly accurate.
|
|
|
|
Figure 4.
Three normal corneas, all with an apical radius of 7.80mm, 43.25 diopters with different eccentricities of 0.32, 0.50 and 0.63. |
The Lens and Its Clearance Factors In designing modern five curve orthokeratology lenses, a number of initial lens-to-cornea clearance factors (Table 1) are required for optimum fitting and tissue displacement performance (Figure 3).
Establishment of these critical clearance factors will be influenced by the underlying corneal topo-graphy, especially in the area of the mid-peripheral cornea. The three normal corneas represented in Figure 4 best illustrate this. All three corneas measure the same apical radius of 7.80mm, 43.25 diopters; however, each has a different eccentricity which can be described as:
- Low eccentricity = 0.32
- Medium eccentricity = 0.50 mm
- High eccentricity = 0.63
It is clear that the 7.80mm cornea with an eccentricity of 0.32 (shape factor 0.10) will require a steeper alignment curve/angle to appropriately align the mid-peripheral cornea. Whereas the 7.80mm cornea with an eccentricity of 0.63 (shape factor 0.40) will require a significantly flatter curve/angle.

Figures 5 illustrates the critical role that corneal eccentricity plays in the ultimate design of a five-curve reverse geometry lens. Both cases used the same underlying model cornea.
- Apical radius Ro = 7.80 mm, 43.25 diopters
- Desired refractive change = 3.00D
- Overall lens diameter = 10.6mm
However, Figure 6 shows a standard eccentricity of 0.50.

To maintain the desired clearance factors of five microns at the apex and 10 microns at the alignment curve, significantly different lens parameters were required in the reverse curve radii and in the alignment curves 1 and 2. Table 2 lists the actual lens parameters required for eccentricities of 0.32, 0.50 and 0.63. Again, the computer software is instrumental in calculating the optimum lens parameters to align the sagittal height of the cornea. These parameters include:
- Base curve radius (BOZR)
- Optical zone diameter (BOZD)
- Reverse curve radius and width
- Alignment curve 1 radius and width
- Alignment curve 2 radius and width
|
|
|
|
Figure 5.
Optimum tear profile of a reverse geometry lens fitted onto a cornea with an apical radius of 7.80 mm, 43.25 diopters. with an
eccentricity of 0.50. |
Some may argue that initial topographical assessment is not necessary and that you can determine the appropriate mid-peripheral fitting relationship by simple fluorescein pattern interpretation of diagnostic lenses. However, it is important to remember the many limitations to fluorescein patterns, not the least of which is a clinical interpretation of ±20 microns.
Computerized Contact Lens Fitting Programs
A number of orthokeratology software programs err in two ways:
- They use the flat K measurement as the central radius of curvature instead of the more desired apical radius
- They assume that the cornea will always have an eccentricity of 0.50.
Therefore, a reverse geometry lens designed to fit a 7.80mm cornea with a eccentricity of 0.50 will result in excessive apical bearing and excessive peripheral lift when placed on the same radius cornea with an actual eccentricity of 0.32 (Figure 6).
|
|
|
|
Figure 6. A reverse geometry lens designed to fit a 7.80mm cornea with an eccentricity of 0.50 will exhibit heavy apical bearing and
excessive peripheral lift when placed on a cornea with an actual
eccentricity of 0.32. |
|
In this case, the assumption that the cornea had an eccentricity of 0.50 will result in a decentered lens with a loss of peripheral lens alignment. Additionally, the lens would be excessively flat centrally with an apical clearance of less than zero.
Conversely, a reverse geometry lens designed to fit a 7.80mm cornea with a eccentricity of 0.50 will result in excessive apical clearance and inadequate peripheral clearance when placed on the same radius cornea with an actual eccentricity of 0.63 (Figure 7).
In this case, the apical clearance will be 23 microns instead of five, and the depth of the tear reservoir will be 71 microns instead of 54 microns. This lens is obviously too steep and will not create the desired refractive changes.
The Accuracy of CCT
Clearly, the accuracy in fitting modern reverse geometry lenses depends on the accuracy of the topographic data. Therefore, it is important to identify the limitations of modern corneal mapping systems and appreciate the fact that the accuracy of any individual reading depends upon:
- The algorithms used to reconstruct the corneal shape
- The image capture hardware
- The stability of the patient and tear film during the capture process
- The number of readings required for statistically significant accuracy
|
|
|
|
Figure 7.
A reverse geometry lens designed to fit a 7.80mm cornea with an eccentricity of 0.50 will exhibit excessive apical clearance with heavy peripheral bearing when placed on a cornea with an actual
eccentricity of 0.63. |
Although all of the above limitations are important, practitioners most frequently overlook the number of readings required to establish accuracy. A recent study by Russell Lowe found that an unacceptable orthokeratology fit could be the direct result of an inaccurate or "rogue" corneal map. Overcome this by obtaining six consecutive topographical maps of each eye. Obtain accurate information by omitting the high and low readings and calculating the mean apical radius and eccentricity values from the remaining four maps. This simple technique helps to avoid many of the fitting problems you encounter when using data from a single map to calculate the initial lens parameters.
Advanced topography systems like the Medmont Topographer (Victoria, Australia), will automatically collect and calculate the mean and standard deviation of the apical radius, elevation, eccentricity and flat K at any nominated chord, making the final lens calculations much easier (Figure 8).
|
|
|
|
Figure 8. A standard deviation plot form the Medmont topography system. The mean and standard deviation of the apical radius and elevation are shown for the four repeat readings. The standard deviation of elevation at a 9.35mm chord is 0.8
microns. |
In Part II we will discuss the use of post-fitting topographical mapping as a guide to better understand the changes which take place beneath modern reverse geometry lenses. Additionally, we will review the role of CCT in problem solving and post-fitting patient management.
To obtain references via fax, call (800) 239-4684 and request document #81. (Have a fax number ready.)
Dr. Mountford is an Optometrist in private practice specializing in advanced contact lenses for keratoconus, post refractive surgery and pediatric aphakia. He is a visiting contact lens lecturer to QUT and UNSW, Australia.
Patrick Caroline is an associate professor of optometry at Pacific University and an assistant professor of ophthalmology at the Oregon Health Sciences University.
Dr. Noack is an optometrist with expertise in advanced contact lens mathematic and computer programming. He has recently retired from practice to work fully on computer applications for contact lens design and manufacture.