DRY EYE
Can a Dry Eye Test Predict Soft Lens Comfort?
This new tear stability test may help you choose the best lens material for your patients.
By Brenda Hall, PhD
Tear break-up time (TBUT) is the sole clinical test used to assess tear film stability and is considered a primary tool for diagnosing dry eye. An unstable tear film is the common denominator in a number of conditions causing dry eye, ocular irritation and contact lens intolerance. A new test that measures tear film stability is now available. This article describes how the Acorn Dry Eye Test (DET) may be used in clinical practice to evaluate tear film stability.
Old and Unreliable
Traditionally clinicians have relied on fluorescein break-up time (FBUT), a technique developed over 30 years ago, for assessing tear film stability. Yet fewer than one in five practitioners in a recent survey rated the FBUT test as their first choice for diagnosing tear film disorders and dry eye.
The main problem with the current FBUT test is its invasive nature and lack of control over volume and concentration of fluorescein instilled. When the standard fluorescein strip is moistened and applied to the bulbar conjunctiva, it delivers an estimated 17µl of fluid to the ocular surface. Because the total volume of the tear film is only 7µl, the excess volume destabilizes the tear film and compromises the measurement, rendering it inaccurate and nonreproducible.
In With the New
To address the problem of excess volume, Akorn Ophthalmics has introduced a modified fluorescein strip designed to deliver precisely 1µl of fluorescein to the eye without disrupting the tear film or causing ocular sensation. The company says that the Akorn DET significantly improves the accuracy and reproducibility of FBUT measurement and enables a more precise diagnosis of dry eye.
Proclear Compatibles (omafilcon A, CooperVision, formerly Biocompatibles Eyecare) was the first soft lens cleared specifically for use in dry eye patients. The specific label claim allowed by the FDA is, "The lenses may provide improved comfort for contact lens wearers who experience mild discomfort or symptoms related to dryness during lens wear associated with evaporative tear deficiency or from aqueous tear deficiency (non-Sjögrens only)." In a dry eye population, the lens has proven to significantly improve comfort and dryness symptoms when compared with other daily wear lenses. With the potential of these two tools to help better treat patients who suffer from dry eye, we decided to look closer at the benefits both have to offer.
Putting New Tools to the Test
We conducted a study to assess the use of the Akorn DET in measuring FBUT and to determine the relationship between BUT and lens comfort in soft contact lens wearers. We also investigated whether we could use the test to predict improvements in comfort that we might achieve by refitting patients with Proclear Compatibles lenses.
Before the study, 47 soft contact lens wearers wore a variety of soft lens brands -- predominantly low- and mid-water content, frequent replacement and disposable lenses. The study took place at three independent sites in the United States and was designed to mimic the process by which practitioners trial fit and refit patients with lenses in everyday practice and the role that the Akorn DET might play in this process.
|
|
|
|
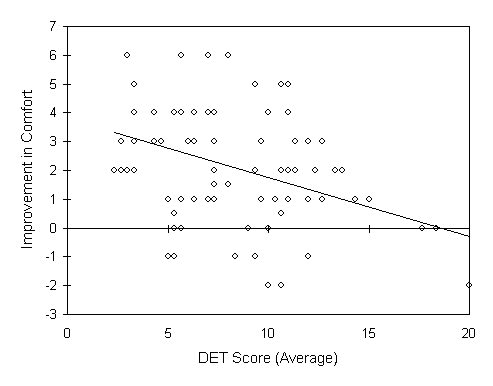
Figure 1. Existing lens performance |
|
At the initial visit, patients completed a questionnaire relating to comfort, dryness and overall satisfaction with their existing lenses by indicating their level of agreement with a number of statements. They then recorded the frequency of symptoms experienced during the previous two weeks. Patients also rated overall comfort with their existing lenses (left and right eye separately) on a scale of 0 to 10, where 0 represents extremely uncomfortable and 10 represents extremely comfortable.
Using the recommended procedure for the Akorn DET, we took three FBUT measurements within 15 minutes of lens removal and averaged them for each eye. We then fit patients with a Proclear Compatibles lens in each eye and again had them rate overall comfort. We dispensed Proclear Compatibles lenses for daily wear for two weeks and told patients to continue using their existing care regimen.
At the two-week follow-up visit, patients rated their comfort with Proclear Compatibles and completed another questionnaire relating to comfort, dryness, frequency of symptoms, overall satisfaction and lens preference during the two-week period of lens wear.
Results
Initial visit Some 87.2 percent and 31.9 percent of patients found their existing lenses comfortable (strongly agree and agree) when they first inserted them and at the end of the day (respectively) (Figure 1). However, 83 percent of patients reported that their existing lenses felt dry at the end of the day, and only 31.9 percent of patients were satisfied with the comfort of their lenses. Wearing time with their existing lenses was limited -- 57.5 percent of patients couldn't wear their lenses for as long as they wanted. Overall, 42.5 percent were satisfied with their existing lenses. The two symptoms patients wearing their existing brand of contact lenses experienced were dryness and lens awareness. A high proportion (81 percent) of patients also experienced itchiness.
|
|
|
|
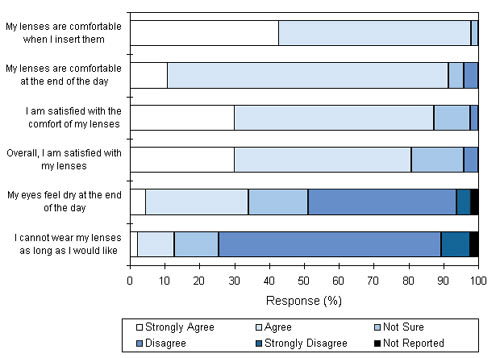
Figure 2. Comparison of comfort with existing lens and Proclear Compatibles (after two weeks'
wear). |
Lemp et al describe a normal TBUT as more than 10 seconds (s). Marginal dry eyes show BUTs of 5s to 9s. BUT of less than 5s is indicative of a dry eye disorder. At the initial visit, 18 eyes (19.1 percent) showed a FBUT of less than 5s; 45 eyes (47.9 percent) showed FBUT between 5s and 10s; 31 eyes (33 percent) showed FBUT of greater than 10s. Some 97 percent of results were within 3s across the three measurements. These results compare favorably with Korb et al (developers of the Akorn DET), who found 96 percent of results within 3s of each other.
We analyzed comfort ratings with the patients' existing lenses for the three groups of eyes based on the initial FBUT measurements. We rated comfort from 1 to 10 where 1 was poorest and 10 was best comfort. Average comfort ratings were 5.9 ± 1.97, 6.2 ± 1.75 and 6.7 ± 1.96 for the low, medium and high FBUT groups, respectively. There were no statistically significant differences between the three groups.
After refitting the patients with Proclear Compatibles, average comfort ratings were 8.9 ± 0.95, 8.3 ± 1.46 and 8.0 ± 1.29 for eyes with a low, medium and high FBUT, respectively. Comfort was significantly higher in the group of eyes with a FBUT of less than 5s (dry eyes) compared to those with a FBUT of greater than 10s (normal eyes).
Two-week visit Comfort with Proclear Compatibles lenses after two weeks of wear was similar to that found at the initial visit, with an average ranging between 8 and 8.8. Paired t-test analysis of the two-week comfort scores by FBUT values at the initial visit confirms that each group of eyes shows a significant (P<0.0001) improvement in comfort over that found with the patients' existing brands (Figure 2).
|
|
|
|
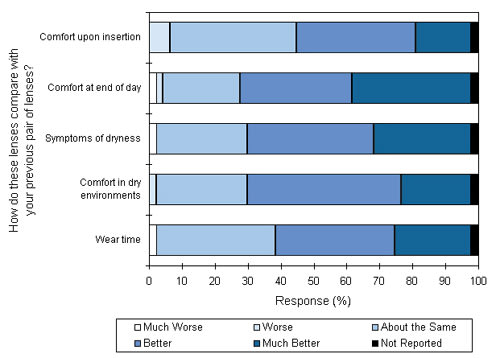
Figure 3. Scatter plot showing difference in comfort vs. DET scores with Proclear Compatibles at two-week visit. |
|
We used Pearson correlation to determine correlations between FBUT at the initial visit and the difference in comfort between the patients' existing lenses and Proclear Compatibles after two weeks of wear. A significant correlation (P<0.001) was found between FBUT and improvement in comfort with Proclear Compatibles (Figure 3). Compared to the normal group, the dry eye group experienced a greater improvement in comfort with Proclear Compatibles lenses than with their existing lenses.
After two weeks of wear, 97.9 percent of patients found Proclear Compatibles comfortable when first inserted, and 91.5 percent found them comfortable at the end of the day, despite the fact that 34.1 percent said that the lenses felt dry at the end of the day (Figure 4).
Some 87.2 percent of patients were satisfied with the overall comfort of the lens. Wearing time was limited in only 12.7 percent of patients and overall, 80.9 percent of patients were satisfied with the lenses. Approximately 57 percent of patients rarely or never experienced symptoms of dryness during the two-week period. Symptoms of redness, itchiness and lens awareness were also infrequent.
At the two-week visit, we also asked patients to compare their experience with Proclear Compatibles lenses to that of their existing lens brand (Figure 5). The percentage of patients who found Proclear Compatibles "better" or "much better" than their existing lenses for comfort on insertion and end-of-day was 53.2 percent and 70.2 percent, respectively. With respect to symptoms of dryness and comfort in dry environments, Proclear Compatibles lenses were rated "better" or "much better" in 68.1 percent of patients. Proclear Compatibles also provided improved wearing time in 59.6 percent of patients.
|
|
|
|
Figure 4. Proclear Compatibles performance at two-week
visit. |
At the end of the study, 92 percent of patients chose to continue wearing Proclear Compatibles rather than their existing lenses.
Discussion
Measurements with the Akorn DET were highly repeatable in that 97 percent of successive FBUT measurements were within 3s of each other. This performance shows a significant improvement over traditional fluorescein strips, which are reported to show 63 percent of measurements within 3s. Other investigators have observed that variations of up to 20s or more are commonly found from one measurement to the next using standard strips.
The results also show good reproducibility between measurements taken at the two visits. The improved repeatability and reproducibility of the Akorn DET compared with conventional BUT measurement will help to improve the diagnosis of normal, borderline and dry eyes. In this study, 19.1 percent of eyes showed BUTs less than 5s, indicating dry eye, and 47.9 percent showed BUTs of 5s to 10s, indicating marginal dry eye.
|
|
|
|
Figure 5. Subjective comparison between existing lens and Proclear Compatibles at two-week visit. |
|
The Akorn DET was also shown to have a useful role in trialing and refitting new lenses and in predicting lens comfort. With Proclear Compatibles, comfort ratings after two weeks of wear were significantly higher than those recorded with the patients' existing lenses at the initial visit. The difference in comfort between their existing lenses and Proclear Compatibles at two weeks was significantly greater in eyes with a FBUT of less than 5s compared to eyes with FBUTs of greater than 10s. There was also a significant correlation between FBUT and improvement in comfort: The lower the FBUT, the greater the improvement in comfort.
A higher proportion of patients found Proclear Compatibles comfortable at the end of the day (91.5 percent) compared with their existing lenses (31.9 percent), and fewer patients found the lenses dry at the end of the day (34.1 percent vs. 83 percent). Nearly 60 percent also found improved wearing times with Proclear Compatibles lenses. The significant improvement in comfort could be the primary reason why 43 of the 47 contact lens wearers chose to continue with Proclear Compatibles lenses rather than returning to their existing brand.
Conclusion
The Akorn DET is a clinically practical method of measuring tear film stability and is a highly repeatable and reproducible test that allows accurate diagnosis of normal, dry and marginally dry eyes.
This study also shows that all patients can experience improved comfort with Proclear Compatibles lenses. Eyes with poor tear stability (low BUT) show a greater improvement in comfort when refitted with this lens than those with a normal tear film. The Akorn DET may prove useful in helping practitioners determine which materials are best suited to their patients' needs based on the quality of each patient's tear film.
Acknowledgements: The author would like to thank the clinical investigators for this study: Terry Carmolli, OD, David Higgins, OD, David Huebner, OD, Stanley Shapleigh, OD, and Kevin Webb, OD. Thanks also to Visioncare Research for help in the preparation of this paper, which is based on a presentation given to the Tear Film and Ocular Society Meeting at the Third International Conference on the Lacrimal Gland, Tear Film and Dry Eye Syndromes: Basic Science and Clinical Relevance.
To receive references via fax, call (800) 239-4684 and request document #85. (Have a fax number ready.)
Dr. Hall is Clinical Projects director at Biocompatibles UK Ltd.