REFRACTIVE SURGERY
Contact Lenses as an Adjunct in Refractive Surgery Practice
Contact lenses can have many pre- and post-op applications within your refractive surgery practice.
By Peter D. Bergenske. OD, FAAO, Patrick J. Caroline,
FCLSA, FAAO, and Jennifer K. Smythe, OD, MS, FAAO
Contact lenses and refractive surgical procedures are very similar in the way they correct for refractive error. In fact, most candidates for refractive surgery could just as well be candidates for contact lenses, and a great many of those electing for refractive surgery are self-professed contact lens failures. Although refractive surgery may save many patients the inconvenience of lens wear, contact lenses offer a wide range of tools that can be effectively used in the refractive surgery practice. The main applications of contact lenses in the refractive surgery practice include corneal rehabilitation of the lens wearer prior to surgery; monovision trials; pain management during epithelial healing phase; temporary or long-term correction of post-surgical over or under correction; and management of post-surgical complications.
Many refractive surgery patients are looking to avoid the inconvenience of contact lens wear, but the similarities of these two options for refractive correction make them inseparable in practice. All contact lens wearers should understand that when they have refractive surgery and have an absolutely perfect result, they will see just as they do with their contact lenses. Contact lenses provide the perfect model for refractive surgery correction, and in cases in which the surgery is less than perfect, they offer a solution that may allow patients to enjoy clarity of vision that they might otherwise have to live without.
Pre-surgical Applications for Contact Lenses
|
|
|
|
Figure 1. Topographic changes occur over a period of months after discontinuing rigid contact
lenses. |
|
Corneal Rehabilitation One of the most common uses for soft contact lenses in the refractive surgery arena is for the rehabilitation of the cornea whose topography has been altered by long- term rigid contact lens wear. It is well known that long-term rigid lens wearers need to abstain from their habitual contact lenses for weeks, or even months, in order to achieve topographic stability (Figure 1). Many of these patients are loath to spend their preoperative "Contact Lent" in spectacles. Disposable soft lenses can offer these patients the ability to wear contact lenses at least some of the time while they wait for corneal stability. A thin, spherical soft contact lens worn on a daily wear basis will have little or no effect on recovery from rigid lens molding. A three-month supply of disposable soft lenses is an economical solution for this waiting period. Toric soft lenses may also be used; but they should be removed at least one week prior to the final preoperative refraction and topography, as should high minus spherical lenses, because both can alter corneal topography. For high myopes, a silicone hydrogel is likely to be a better choice in order to minimize the effects of inadequate oxygen. Any lenses should be worn only as needed and never on an overnight basis. In any event, it is recommended that even low power soft lenses be removed a minimum of 72 hours prior to surgery.
Monovision Trials Another valuable preoperative application for contact lenses is to allow patients to experience monovision prior to making a surgical commitment to this modality. Studies of monovision with contact lenses have shown that approximately 20 to 30 percent of individuals experience difficulty adjusting to monovision correction; using contact lenses to test the acceptability of monovision can help avoid disappointment and unnecessary enhancements later on. Contact lenses allow the patient and practitioner to determine in advance the proper laterality and ideal degree of anisometropia to target for optimum result. Don't follow the myth that the distance correction must always be on the dominant eye; most successful monovision patients tolerate the distance correction on either eye.
Determining such flexibility is easy with contact lenses but can be costly and problematic with surgical correction. As refractive surgery does not provide the precision and forgiveness of contact lens correction, determining the ideal target for each eye in advance has its merits. In some cases, the refractive surgery candidate may already be wearing rigid or soft lenses on a monovision basis. If the current correction has been satisfactory, information from the patient's contact lens experience can be used to determine the targeted laser correction.
|
When is the veteran contact lens wearer ready? |
|
Topography: Inferior steepening should resolve to normal, with-the-rule topography Refraction: Should be repeatable and provide crisp acuity. Cylinder axis should correlate closely with axis indicated by topography Retinoscopy: Reflex should be free of distortion or scissoring Fitting contact lenses after surgery
|
|
Testing for acceptance of monovision does not require that the patient already be presbyopic. A trial with monovision may be in order, particularly for the pre-presbyope, if the patient's hope is to be as free from spectacles for as long as possible.
Peri-operative Applications
Pain Management Soft contact lenses have been used effectively for pain management during healing of epithelial defects following PRK or LASIK in the immediate postoperative phase. With the exception of therapeutic bandage use, avoid contact lens use in most cases during the initial postoperative month because hypoxic effects may influence healing, and the process of inserting and removing a contact lens may disrupt the flap in the early phase of healing. On the other hand, it has been reported that a plus power soft lens worn on an overnight basis may promote regression in cases of significant over-correction of myopia. Hypoxia is presumed to be responsible for this effect.
Over and Under Correction Refractive compensation for over and under correction are obvious uses for contact lenses in postoperative care, although, for some patients, contact lenses are not a satisfactory long-term solution. On the other hand, contact lenses can provide the perfect solution for patients who have chosen monovision and occasionally want bilateral distance vision for activities such as golf or tennis. Likewise, the presbyopic patient who has perfect distance vision may enjoy monovision under special circumstances. Either of these situations are often well suited to single-use disposable lenses.
In most situations, soft contact lenses are the preferred choice due to ease of fit and initial comfort. Thin soft lenses are best suited, as they will drape relatively easily on the plateau topography of the post surgical cornea. Base the selection of base curve radius on the visible iris diameter, which is more indicative of the needed sagittal depth than the altered central curvature. That is, for larger corneas (greater than 12.0mm) a steeper curve is often required despite the flat central radius of curvature. Smaller corneas (less than 11.6mm) often require a flatter base curve radius. Depending upon the power and rigidity of the material, a soft lens may slightly vault over the central treatment area of the cornea, creating a plus tear lens. The final lens power may therefore be unpredictable and best determined by refraction over an adapted lens. For example, the patient who displays a 1.00D refraction may require a 1.50D lens for optimum vision due to a tear layer optical effect. The only accurate way to determine this is to apply lenses of known power and over-refract. On the same token, never base the target for enhancement correction on contact lens power. As previously noted, the refraction without the lens in place can often be quite different from the lens power due to a tear layer, lacrimal lens effect. Thin plus lenses, with a thicker optical zone and thin periphery, tend to center and fit well on the typical post laser cornea. Plus power, multifocal soft lenses have also been utilized successfully on post-LASIK patients who have hyperopic and presbyopic errors.
In cases in which the amount of ablated tissue is great, the geometry of the cornea may require a special rigid lens design that may incorporate scleral support, a reverse curve or both of these features.
Post-operative Complication Management
The vast majority of LASIK patients have good, or even excellent, visual outcomes, but a small percentage of complications do occur. Fortunately, many of these resolve with time or enhancement procedures. Some complications can best be managed with contact lenses at least until further surgical treatment is safe or reasonable. Postoperative visual compromise resulting in significant, persistent glare and irregular astigmatism may be due to flap irregularities, decentered ablation or central islands or haze.
Flap Complications
Too Thin Flaps In LASIK, loss of adequate suction during the procedure typically results in a thin and usually irregular flap. In some cases, the flap is so thin centrally that a "buttonhole" is created. If the thin flap is recognized and the surgeon uses good judgment, simple replacement and smoothing of the flap will generally result in little long-term effect on visual acuity or refractive error. After three months, the procedure may be safely attempted again.
Unfortunately for some patients, lesser skilled and over confident surgeons too often proceed with the laser ablation despite the thin flap, creating an irregular corneal surface that may be difficult or impossible to improve with further surgery. Particularly problematic is the "buttonhole" cornea that has been lasered, as this often results in scarring and irregularity centered over the visual axis.
|
|
|
|
Figure 2. A flap that is too thick can lead to corneal ectasia with
keratoconus-like topography and vision. |
|
Too Thick Flaps Error in proper assembly of the microkeratome has been associated with the creation of an abnormally thick flap and, in some cases, actual penetration of the cornea. With overly thick flaps, too little stroma remains, particularly if ablation is performed. Insufficient stromal bed following any surgical procedure results in corneal ectasia. Such eyes display keratoconus-like topography and develop high degrees of irregular astigmatism (Figure 2). Ultimate resolution can be achieved only with corneal transplant; however, rigid lenses can allow the patient functional vision during the interim.
Lost Flap Loss of the corneal flap is a rare LASIK complication that can result in extreme corneal surface irregularity. Rigid contact lens fitting is often indicated but may be complicated by the resultant extreme oblate corneal shape.
|
|
|
|
Figure 3. Decentered ablation usually results in under-correction and glare. The asymmetric topography creates significant fitting challenges. |
|
Decentered Ablation Both PRK and LASIK can cause over and under correction, as well as decentered ablations (Figure 3). Decentered ablations may be managed with soft or rigid lenses, but rigid lenses may gravitate to the decentration and not provide adequate vision correction. Undercorrection is typical in decentered ablation, so patients benefit from refractive correction. High modulus, or thicker, soft lenses can help. Sometimes a specially designed soft lens with a thickened optic zone and thin periphery, such as the Harrison PRS (X-Cel Contacts, formerly owned by Paragon), may be useful.
Reverse Curve Lenses
The variety in presentation of complications in the post refractive surgery patient is great and as such requires a wide variety of remedies. Many lessons have been learned from the management of post-radial keratotomy patients. Rigid lens fitting is typically focused on the peripheral cornea (outside the central flattening zone or the flattened zone in radial keratotomy). Rigid lenses can be used at least as a diagnostic tool when dealing with patients with irregular topography, and in some cases they offer the only solution for improving acuity.
|
|
|
|
Figure 4. Reverse curve
designs can help fit the
altered corneal shape. |
|
Reverse curve lenses have been successful in many postoperative cases where central flattening is extreme and spans a large area (Figure 4). Success with such designs in post-radial keratotomy eyes may be complicated by possible corneal irregularities, resulting in lens decentration. This is usually not the case following laser procedures. Fit these lenses, which have a flatter optic zone and steeper periphery, to align or slightly vault the ablated zone and fit the remaining peripheral cornea.
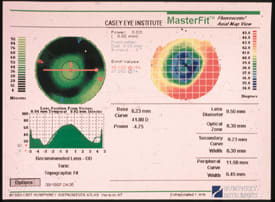
Topography as a Fitting Aid
|
|
|
|
Figure 5. Rigid lens fitting is concentrated on the
unaltered, peripheral cornea. |
|
Topography is a great fitting aid. Use the curvature just outside the ablation zone (4mm temporal from center) as the base curve of the conventional lens or the peripheral zone curve of the reverse geometry lens (Figure 5). The central curve of the reverse geometry lens is often three to four diopters flatter. The optic zone of the lens should be just a bit larger than the ablation zone, 6.5mm to 7.0mm.
Conclusion
Fitting post-LASIK or PRK eyes requires a wide variety of lens types, and fitters must be flexible in skill and knowledge. Conventional lenses will often provide good results, but many cases will require special designs and unique applications. In cases requiring correction of extreme irregular astigmatism, rigid lenses that have scleral support may be necessary in order to achieve centration and stability. Soft lenses can be helpful in cases of mild irregularity.
Dr. Bergenske, a Past Chair of the American Academy of Optometry's Section on Cornea and Contact Lenses, has practiced for over 20 years in Wisconsin and now is on the faculty at Pacific University College of Optometry
Mr. Caroline is an associate professor of optometry at Pacific University and an assistant professor of ophthalmology at the Oregon Health Sciences University.
Dr. Smythe is an Associate Professor of Optometry at the Pacific University College of Optometry and a Diplomate in the Section on Cornea & Contact Lenses of the AAO.
|
Discontinuing Contact Lenses Prior to Refractive Surgery |
|
Rigid Lenses Most experienced clinicians agree that patients wearing rigid contact lenses must discontinue lens wear for several weeks (at least) to be certain the corneal shape has stabilized. The most common effects from long-term contact lens wear are inferior steepening and sphericalization. Some patients have excessive corneal molding from contact lenses, which may take months to resolve, and others will be stable within days. The most accurate way to determine stability is by repeat topography and refraction. There should be a crisp endpoint to best corrected acuity and distortion-free retinoscopic reflex. The safest approach is to allow at least one month after lens removal, but the patient should be prepared to wait longer if needed. One rule of thumb is that the patient will need to be out of RGP lenses one month for every decade of lens wear. This means the 30-year veteran of rigid lens wear should plan on three months of non-lens wear prior to surgery. Soft Lenses It is generally believed that soft contact lenses do not cause significant corneal molding, and often this is the case. On the other hand, thicker lenses such as high minus, toric or plus power soft lenses, as well as any lens worn overnight, can cause temporary corneal changes and need to be removed from the eyes long enough to allow the cornea to resume a consistent shape. As with rigid lenses, repeat topography, refraction and retinoscopic examination should be used to determine complete recovery. Even with no evidence of influence, a minimum of 72 hours of soft lens abstention is prudent prior to surgery. |
|