RGP MULTIFOCALS
Comparing RGP Multifocal Lens Designs
Comparing classic RGP alternating multifocal systems to a simultaneous alternating multifocal lens design.
By Andreas Allmoslechner, MCOptom, MS,
FAAO
The job of an eyecare practitioner is to provide the best possible vision with the least necessary restriction. Some 40 percent of the population exceeds the age of 45. Industry data indicates that between 20 and 50 percent of presbyopes are interested in contact lenses. These numbers show that eyecare practitioners can anticipate a great deal of growth in fitting presbyopes with contact lenses in the future.
This growth, however, depends on whether practitioners can fulfill the patients' expected level of satisfaction. The rising number of multifocal lens designs offers practitioners new possibilities in satisfying presbyopes who are both previous lens wearers and newcomers. Alternating multifocal systems offer, especially in the area of optics, clear advantages compared to all other multifocal systems.
Selecting Candidates
Presbyopic patients are more than just young people with receding accommodation. With increasing age, the eye is subject to various changes that you need to consider when fitting contact lenses (see "Age-related Fitting Concerns").
New wearers with a distance correction of +0.75D to 2.00D may have problems succeeding. Success is greater for patients with a history of lens wear, especially RGP lenses. The expected astigmatism over a spherical or back surface toric lens should be < 0.75D, and the near addition should be > +1.00D.
Patients must be motivated to succeed with multifocal lenses and have the needed financial means to invest in this modality. Most candidates are unhappy with their spectacles and find changing spectacles or multifocal lenses bothersome, or they want presbyopic lenses to maintain a youthful, dynamic and vital image.
Practitioners must choose the correct presbyopic system for each patient from the start. Also, the practitioner's positive attitude is just as important as the necessary knowledge.
Classic Alternating Systems
Alternating multifocal systems correct both near and far because the contact lens features two optical spheres of activity that are placed differentiated in front of the pupil (Figure 1). The design requires that the lens moves freely. While looking in the distance, mostly straight ahead, the distance part of the lens must be in front of the pupil. While looking at near objects, mostly downward, the near part of the lens lies in front of the pupil. Patients perceive the dividing line less compared to bifocal spectacles.
Advantages of classic, alternating systems:
- Clearly differentiated near and distance zones
- Good vision with good contrast
- Custom design
- Possibility for the fitter to distinguish himself
- Exclusion of the mail-order business
- Fitting based on corneal topography possible
- Wide range of parameters
|
|
|
|
Figure 1. Optical zones of a classic alternating RGP bifocal
system. |
Disadvantages of classic, alternating systems:
- Prismatic stabilization often produces thicker lenses that can reduce oxygen permeability
- Stabilization with truncation affects meibomian gland secretion, which often leads to more rapid soiling of the lens. Truncation also requires a longer settling-in period
- The transition line from far to near is, depending on the lens, prone to deposits
- The fit is not easy and is not always economically advantageous
- Position and lid pressure affect the lens fit, which affects the optics on the system
- Lens movement may cause variations in visual acuity, depending on the position of the near and distance zones
- In dim lighting, the pupil widens and a greater field of the near zone rests in front of the pupil
- The dividing line can cause reflections
Effective alternating multifocal systems require:
- Easy transfer from spherical monofocal lenses to presbyopic lenses
- Simple, effective adaptation
- Dividing line without an obvious jump
- Minimal, even thickness
- Distance and near zones evenly distributed over different pupil openings
- Constant stabilization to avoid truncation
Fitting Classic RGP Alternating Systems
To fit classic alternating RGP multifocal contact lenses, you must first understand the system as a whole. When the eye looks down, the lid position changes (Figure 2). For example, the upper eyelid varies 0.23mm parallel to the corneal apex during downgaze, whereas the lower eyelid sinks by only 0.11mm. The result is a palpebral fissure constriction of 0.12mm, which, with 20 degrees of movement, leads to a palpebral fissure constriction of 2.4mm. Dieter Muckenhirn published these findings in DOZ Deutsche Optiker Zeitung in 1992.
Alternating systems require unrestricted vertical lens movement. Influential factors are lid closure, lid position and pressure. The vertical corneal diameter and the vertical corneal scleral profile determine the path along which a stable lens can travel. The smaller the corneal diameter in proportion to lens diameter, the smaller the path of vertical movement.
Astigmatism, depending on how high the amount, may affect lens movement. The lens may move suddenly or tip in a meridian.
The entire corneal topography is relevant to lens movement. The amount of tears and composition can change movement. The state of the lens, such as diameter, thickness, inside geometry, bevel, edge, weight and surface are factors for vertical mobility.
|
|
|
|
Figure 2. The lower lid changes position when the eye looks down. |
Measuring and Assessing Alternating Multifocal Lens Adaptation
- Measure the corneal topography to define the contact lens geometry
- Measure the corneal diameter to define the contact lens diameter
- Define the maximum and minimum pupil diameter and position (central, nasal, decentered)
- Assess the lid position: a lower lid position 2.0mm under or 3.0mm above the limbus can cause difficulties
- Measure the lid palebral fissure height
- Assess the vertical cornea scleral profile
- Assess the visual axis by the eye movement to near fixation and assess the amount of head movement
- Assess the tear film
Basic Function and Demands
|
|
|
|
Figure 3. Classic RGP alternating
system. |
|
When the patient gazes straight ahead, the dividing line should position on the lower part of the pupil, and the near segment should cover no more than 20 percent of the pupil for tolerable distance vision.
During downgaze, the lens remains stable on the lower lid compared to the downward movement of the eye, and the near segment positions in front of the pupil. We have found that vision is sufficient if the near segment covers two-thirds of the pupil during downgaze. When looking at near, the pupil is smaller and uses more foveal vision. Complete translation requires that the lens moves the same distance at the size of the pupil diameter (3.0mm to 4.0mm).
Assessing the trial lens on the eye:
- Determine the back surface of the lens based on the fluorescein pattern
- Define the stabilization axis and dividing line
- Assess the geometrical lens center to the pupil
- Define lens fit in normal head and eye position
- Over-refract distance and near
Figure 3 shows an alternating bifocal lens fit.
|
|
Effects on Adaption
Stabilization prism determines essential lens positioning. The ballast and the lid dynamic result in a centering downward. Make sure that the near segment does not cover more than 50 percent of the pupil during blinking.
A steeper fit is usually less successful because it can stagnate the precorneal tear film and cause lens binding. Enlarging lens diameter decreases lens movement, which could prevent the near segment from translating properly in front of the pupil. Thicker lenses decrease both the prism's effect and the oxygen permeability. A thinner lens with a smaller total diameter is often a change for the better.
Use an inside toric lens (back surface toric) if the corneal astigmatism is higher than 2.00D. You may need to modify the lens, such as thinning the edge or making the lens oval in the upper region.
The Presbylite Multifocal System
The Sub Micron lathing technique allowed, for the first time, reproducible lens surface forms without polishing. This technique made possible a new presbyopic lens type: combined monocentric, bivisual alternating or simultaneous alternating system.
The near zone of the Presbylite lens (Lens Dynamics) is distributed over one-third of the lens, and the distance zone covers the remaining two-thirds. The lens structure allows minimal thickness. Truncation is not necessary for stability. This guarantees best possible oxygen permeability. The independent design provides an even distribution of the near zone and distance zone for different pupil sizes. The back surface geometry can be spherical or back surface toric. Fitting from corneal topography is possible.
Presbylite Adaptation
Successful adaptation of Presbylite lenses is possible with only two Presbylite lens versions. Choose the first trial lens based on refraction and corneal topography. Use the ophthalmoscope to evaluate the fit of the trial lens and its movement. Near and distance vision segments are easy to recognize in the reflex of the retina. Check the recentering time, which should remain under one second. If it is greater than one second, try changing the lens radius or diameter or switch to a back surface toric design. If the recentering time is not reduced, stop the fitting procedure.
|
|
|
|
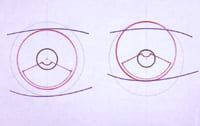
Figure 4. Optimal position of the Presbylite multifocal RGP lens at distance (left) and near (right). |
The Presbylite lens features two marks in the horizontal axis. The imagined line between the two marks passes through the center of the lens where the optical focus rests. If this line passes through the lower third of the pupil, use Presbylite version C. If the imagined line falls above the lower third of the pupil, use Presbylite version CL. A central or lower fit is best (Figure 4). If changing the lens geometry does not improve the fit, again stop the procedure.
Over-refraction is best performed with the trial frame. For the distance correction, use the maximum plus. Determine how the distance power coincides with the refraction before defining the near add. Use a slit lamp to assess the fluoroscein pattern and determine lens stabilization. If lens rotation >30 degrees nasal or >10 degrees temporal occurs, compensate for it in the final lens order.
To receive references via fax, call 800-239-4684 and request document #82. (Have your fax number ready.)