IRREGULAR CORNEAS
Managing Irregular Corneas with Gas Permeable Lenses
Three cases show that trial and error and careful fluorescein evaluation are needed to success-fully fit irregular corneas.
By Shelley I. Cutler, OD, FAAO, Loretta B.
Szczotka, OD, MS, FAAO, Robert Maynard, OD, Bruce Anderson, OD, FAAO, and Edward S. Bennett, OD,
MSEd
Patients exhibiting irregular corneas are best corrected with oxygen permeable (GP) contact lenses. Quality of vision with GP lenses is typically unparalleled when compared to soft lenses or spectacles.
Patients with irregular corneas are among the most challenging in contact lens practice, particularly post-surgical cases. Every case is unique and, as the following cases illustrate, no one lens design or fitting method is ideal. Drs. Shelley Cutler and Loretta Szczotka presented the following cases during the May online symposium sponsored by the RGP Lens Institute. The RGPLI's web site (www.rgpli.org) provides an online symposium on various GP topics the second Tuesday night of every month.
|
|
|
|
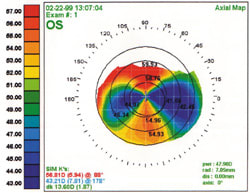
Figure 1. Penetrating keratoplasty resulted in over 9.00D of corneal toricity for this patient. |
|
Case One
History A 78-year-old male needed a contact lens following penetrating keratoplasty OD. The refraction was +2.50 6.50 x 080, resulting in blurry 20/70 best corrected visual acuity. His corneal topography revealed 9.00D of corneal toricity (Figure 1).
The Fitting Process A few large diameter, flat base curve lenses were initially trial fit to determine if the positioning and fluorescein patterns were acceptable. The first was the Post Graft Lens (Lens Dynamics), with 8.04mm base curve radius (BCR), 10.4mm overall diameter (OAD) and 9.0mm optical zone diameter (OZD). The second was the Post PK lens (Infinity Optical) (8.04mm BCR, 11.0mm OAD, 9.5mm OZD).
Both lenses decentered temporally, and the fluorescein pattern showed that the amount of toricity contributed to the decentration. We then tried a bitoric design. Initial lens parameters included 8.25mm/7.54mm BCR, 9.5mm OAD and 8.0mm OZD. This lens also decentered temporally, but aligned better. The final design was a 4.00D spherical power effect (SPE) bitoric with a larger diameter to improve centration. Final design parameters included: BCR: 8.10mm/7.40mm, powers: +0.25/ 3.75D, OAD: 11.0mm, OZD: 9.5mm, SCR/W: 9.20/8.50 @ .5mm; PCR/W: 11.20/10.50 @ 0.25mm. The lens-to-cornea fitting relationship was much improved, and this lens yielded a visual acuity of 20/25.
|
|
|
|
Figure 2. This patient's penetrating keratoplasty resulted in over 13.50D of corneal astigmatism. |
Discussion Recognize that bitoric lenses, on occasion, have applications in post-surgical cases. Although most such cases result in not only high cylinder but also irregular astigmatism, a bitoric lens may be used if the topography shows significant regular astigmatism, greater than 4.00D. This astigmatism should be fairly regular across the entire surface of the cornea and not limited to the graft.
If you analyze the central cornea with keratometry only, you can expect a large amount of astigmatism. However, when you compare this with topography measurement, you may observe that this astigmatism exists in only the central 3.0mm to 5.0mm of the cornea. In this case an aspheric or spherical base curve lens may be more successful because it vaults over the central cornea to the more spherical peripheral cornea. When high regular astigmatism extends across the cornea, a bitoric lens design will provide a more stable fitting relationship without excessive bearing along the flatter meridian. This is especially important in a post-PK cornea, as excessive bearing with a spherical design may irritate the graft and initiate physiological changes.
This case also illustrates how important it is to carefully evaluate the post-surgical cornea. Bruce Anderson, OD, FAAO, divides the cornea into three zones: the central (donor tissue) region, the graft junction and the peripheral host cornea. How each of these areas are configured and how each effaces the next zone will dictate which type and design of contact lens to fit. Evaluate the central cornea for significant astigmatism and irregularities and measure the curvature of this region. Evaluate the graft interface 360 degrees for evenness or elevations between the host and donor tissues. Examine the peripheral cornea for smoothness or puckering due to tight sutures.
Use fluorescein when fitting the trial lenses on the eye to help you more accurately determine the high (bearing) and low (pooling) areas of the contact lens against the cornea. Careful fluorescein pattern evaluation will help determine a proper fit. The goal is to avoid heavy bearing areas and hope for an even or light touch fluorescein pattern.
|
|
|
|
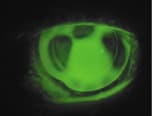
Figure 3. The MacroLens as fit on the patient in Figure
2. |
|
Case Two
History A 73-year-old female was referred for potential contact lens fitting. She had undergone penetrating keratoplasty resulting from Fuch's dystrophy. The surgery resulted in 13.50D of corneal astigmatism (Figure 2). If the lens fit was unsuccessful, a refractive surgeon would perform LASIK on the transplanted eye. Her visual acuity with pinhole was 20/300. The refraction was very difficult to perform.
Fitting Process Initial bitoric lens attempts, including a 10.00D back surface toricity lens, all tended to decenter or even eject out of the eye with the blink. Her visual acuity was 20/50. A reverse piggyback tandem of a soft lens placed on top of a GP lens failed to provide an optimum fitting relationship in this case.
We then fit the patient with the semi-scleral MacroLens (C & H Contacts, Inc.) After several trial lenses (8.04mm, 7.94mm, 7.85mm), a steeper base curve lens was ordered (7.50mm). Figure 3 shows the fitting relationship. Although the patient was satisfied with this lens, it caused central superficial punctate keratitis (SPK). Her visual acuity was 20/50. We refit her into the Epicon lens (Specialty Ultravision) with a 6.80mm BCR to determine if corneal health would improve. The result was excellent corneal integrity with 20/40+ visual acuity. Unfortunately, the Epicon lens is no longer available in the United States.
|
|
|
|
Figure 4. Initial GP lens fit for a patient with a history of a penetrating keratoplasty and cataract
surgery. |
Discussion This case illustrates the benefits and applications of large diameter GP lenses in post-surgical cases. They can be very beneficial for patients with high cylinder, "proud grafts" and very irregular corneas. It is not uncommon to initiate the fitting process with a conventional diameter lens; however, these cases show that the cornea may not hold a conventional lens, primarily when the superior or inferior cornea is too steep and there is a significant plateau or drop. A smaller diameter lens passing over this region may result in excessive edge lift that could cause lens decentration or even ejection from the eye.
Common large diameter lens designs include the MacroLens, the Epicon lens, Dyna Intra-Limbal lens and Post Graft lens (Lens Dynamics) and the PSC lens (Infinity Optical). The Dyna Intra-Limbal lens has an 11.2mm OAD with a 9.4mm OZD and is recommended for tilted and/or decentered grafts. The Post Graft lens has a 10.4mm OAD and 9.0mm OZD with an aspheric periphery. The MacroLens has OADs ranging from 12.9mm to 15.0mm and a BCR range from 39.00 to 51.00 diopters. This base curve range has limited the applications of this lens in very steep corneas.
These designs typically have proprietary peripheral curves. Many laboratories have specialty lenses for post-surgical patients or are willing to manufacture a larger diameter lens when desired. For example, a patient with a history of both a penetrating keratoplasty and cataract surgery was initially fitted with a large diameter (12.4mm), very flat base curve radius (11.00mm) GP lens (Figure 4). This patient eventually found success with a 12.5mm diameter lens that had a 10.65mm base curve radius and an aspheric periphery (Figure 5), manufactured by Metro Optics (Austin, TX).
This case emphasizes three important factors in fitting post-surgical corneas:
- You must work with your laboratory consultant to achieve a successful fit.
- You do not need to be an expert to fit these contact lenses, but you must be open to using multiple lens designs and treating every post-surgical eye as unique.
- Careful fluorescein pattern evaluation is imperative.
Many CLMA member laboratories have lens designs for irregular/post-surgical corneas. You can access them either via the RGPLI web site or the RGPLI GP Product Guide, a supplement to this issue of Contact Lens Spectrum.
The most significant problem with a large diameter contact lens notably one as large as the MacroLens is a tight fit and possible adherence. Large scleral imprints may also result. These lenses can actually tighten up over time. When fitting any large diameter lens design, use diagnostic lenses and provide sufficient time for the lens to stabilize on the eye to properly evaluate the lens-to-cornea fitting relationship. It is not uncommon for a large diameter design to exhibit a good fitting relationship initially, then tighten on the eye so that 20 minutes later there is very little movement. When this occurs, select another diagnostic lens and then re-evaluate the fit. This is a more time-consuming fitting process, but ensuring that a good fitting relationship is achieved initially will reduce future chair time.
A second problem with large diameter designs, related to the first, is poor tear flow under the lens. Even in the presence of a good fitting relationship, the design limits tear flow, which creates problems with trapped mucus and debris accumulating underneath the lens as well as superficial punctate keratitis and hypoxia. In these cases, perform careful fluorescein evaluation of the entire 360 degrees of the lens periphery. Under the peripheral lens region, 270 degrees to 360 degrees of pooling should be present. If you use a MacroLens, look for edge clearance, not impingement, at the sclera. Flattening the secondary and, most important, the peripheral curve radius should improve both peripheral pooling and lens movement with the blink. Use a radius tool as flat as 13.0mm to accomplish the latter change.
|
|
|
|
Figure 5. The patient from Figure 4 succeeded with a large diameter lens that features an aspheric periphery. |
|
Another option for a post-graft eye is a reverse geometry lens (RGL) design that incorporates a steeper secondary curve than base curve radius. An RGL design is especially beneficial in oblate grafts, which you can detect only with corneal topography. An RGL is an excellent option if there is peripheral steepening, at minimum, 270 degrees surrounding the graft.
Dr. Szczotka uses axial maps to measure the amount of steepening from the center to the mid-periphery, then orders the secondary curves this same amount steeper than the base curve radius. Many laboratories provide RGL designs featuring secondary curve radii with varying amounts of steepening relative to the base curve. This can help post-graft and post-refractive surgery cases, as it is not uncommon to find upon fluorescein evaluation that a certain base curve fits well but the periphery is too loose and requires a steeper secondary curve. However, transition zones can be more abrupt in a post-graft than a post-LASIK eye, which would necessitate a steeper than average secondary curve radius in the RGL design.
Case Three
History This 50-year-old female had been diagnosed with pellucid marginal degeneration (PMD). Her spectacle refraction was: OD: 3.75 3.25 x 095; OS: 0.75 3.75 x 076, 20/40 OU. The pupil diameter was 6.0mm in normal illumination OU.
Fitting Process We initially attempted several conventional spherical lens designs. The initial lenses ordered were:
OD: 7.50mm BCR, 9.9mm OAD, 8.5mm OZD, 14.2mm diameter, 6.37D, Paragon HDS
OS: 7.40mm BCR, 9.9 OAD, 8.5mm OZD, 14.2mm diameter, 6.12D, Paragon HDS
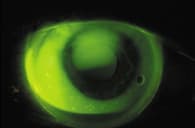
The patient noticed glare OU and had an adherence ring inferiorally upon contact lens removal as well as spectacle blur. The over-refraction was: OD: +1.00 1.25 x 068 (20/25); OS: +0.75 0.75 x 018 (20/25). We then refit her into the MacroLens with the following parameters:
OD: 7.14mm BCR, 0.8 "E" value; 7.75D, three fenestrations (Macro A) 20/30
OS: 7.14mm BCR, 0.8 "E" value, 6.25D, three fenestrations (Macro A) 20/25
|
|
|
|
Figure 6. White light illumination of a MacroLens fit on a PMD patient. |
The fitting relationship was acceptable (Figures 6 and 7) and the patient was very satisfied with her vision with no complaints of glare. However, she felt the right lens was "pinching" the eye.
She was then refit successfully into Dyna Intra-Limbal lenses in the following lens parameters:
OD: 7.34mm BCR, 12.2mm OAD 8.6mm OZD, 8.00D; 20/20
OS: BCR: 7.34mm; OAD/OZD: 12.2/8.6mm; 6.00D; 20/30
These lenses provided a good fitting relationship with adequate movement and satisfactory patient comfort and vision.
Discussion This case demonstrates another example of specialty lenses successfully fit on irregular corneas. However, many of these cases can succeed with conventional spherical lenses. Typically, for post-surgical cases, select a diameter that is larger than the graft or flap. If the central cornea is very steep with minimal astigmatism, Dr. Anderson selects an OAD as small as 9.0mm. In very flat corneas, with corneal elevation in the suture zone, he uses lenses as large as 11.0mm. The latter lens may have as many as four to five peripheral curves, with the outer curve being especially flat. Make the optical zone conventional to small to decrease the sagittal depth of the lens design, and allow for more stable centration on the flat post-surgical eye. Use topography to select the base curve radius, which can be equivalent to the value a few millimeters off the apex or the average curvature from the axial map.
Because most of these patients are myopic, the best material is one that exhibits good wettability and resists flexure, especially on highly astigmatic patients. Therefore, we recommend a low (25 to 50) Dk fluorosilicone/acrylate lens, assuming these patients will be limited to daily wear. A higher Dk lens material (> 50) is indicated for hyperopic patients to provide an edema-free state.
|
|
|
|
Figure 7. Fluorescein pattern of the MacroLens on the PMD patient from Figure
6. |
Conclusion
Irregular cornea patients, especially post-surgical, are quite challenging to fit with contact lenses. Be patient; do not become frustrated if you are on your fourth lens. Do not to be afraid to make a major change if one design is not successful. Trial and error, in combination with careful fluorescein evaluation, is paramount to success.
Dr. Cutler is a contact lens consultant and specializes in fitting difficult contact lens cases. She has lectured worldwide on various contact lens-related topics.
Dr. Szczotka is an associate professor at Case Western Reserve University Dept. of Ophthalmology and Director of the Contact Lens Service at University Hospitals of Cleveland.
Dr. Maynard has been in private practice in Phoenix and Superior, AZ, since 1967 and has served as a clinical investigator for a number of contact lens companies.
Dr. Anderson is a Diplomate in Cornea and Contact Lenses. He is also a Clinical Assistant Professor of Ophthalmology at the University of South Florida and director of the Contact Lens and Low Vision Clinics at the Department of Ophthalmology/College of Medicine.
Dr. Bennett is an associate professor of optometry at the University of Missouri-St. Louis and executive director of the RGP Lens Institute.