ORTHOKERATOLOGY
A Look at Ortho-k and Corneal Epithelium Health
This study investigates the use of
single-fit lenses for ortho-k and how they effect the corneal epithelium.
By Ruiduan Liao, Juanjuan Feng, Yongcong Chen, Jingwen Wang and Wenhui Zhu
Accelerated orthokeratology (ortho-k) has been widely used to treat myopia in China. We usually use only subjective refraction and keratometry readings to order orthokeratology lenses for patients. Typically we do this without a detailed fitting trial. Our goal is no lens refitting during the procedure. This procedure was what we wanted to evaluate in this report because many practitioners have hoped this procedure would work.
|
|
|
|
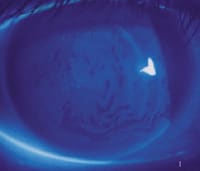
Figure 1. An example of
low-grade corneal staining. |
|
Safety of the ocular surface is a great concern for us. We wanted to know if individual corneal variation would result in lens position variation or affect corneal shape during treatment. We also wondered if overnight wear of ortho-k lenses had any side effects on corneal health as assessed by corneal fluorescein staining.
We investigated whether accelerated ortho-k using a single-fit lens for all patients can reduce myopia and still maintain corneal epithelium health, by analyzing the relationship between lens positions and corneal staining. We'll share the details and the results of our investigation.
Setting Up the Study
We performed a retinoscopy examination in the mydriatic condition, subjective refraction and keratometry and corneal topography to assess the corneal curvature and eccentricity value for each of the 147 (51 male, 96 female) young myopic subjects (292 eyes), who ranged in age from 10 to 30 years. Their subjective refractions ranged from �1.00D to �9.00D (average in �4.26D) with astigmatism of less than �2.00D and unaided visual acuities (VAs) from 20/40 to 20/2000. We then trial fit each patient with diagnostic lenses that had a base curve (BC) limited to 3.50D flatter than the subject's flat K for an efficient fit estimation.
We then fit each subject with optimal four-curve reverse geometry design ortho-k lenses (with a Dk of 58 and a 10mm diameter). All subjects wore the original pair of lenses overnight (for eight to 10 hours) for 28 days and removed them during the day. We measured and examined unaided VA, subjective refraction and corneal topography and evaluated lens movement, lens position, fluorescein pattern and corneal staining for each subject the day after we dispensed the lenses and weekly thereafter.
We analyzed the effect of ortho-k and the relationship between corneal staining and lens position mainly according to the results of the first and the 28th days.
|
|
|
|
Figure
2. An example of higher-grade staining. |
Examining the Results
Of the 292 eyes, 60 reached an unaided VA of 20/25+ after one night of wear. On the 28th day of observation, 219 eyes had reached 20/25 or better. We found corneal staining in 131 treated eyes, among which 69 percent (90 eyes) had tight-fitting lenses moving less than 1mm. Tight-fitting lenses were more likely to exhibit staining. The subjective refraction decreased in average from the initial �4.26D to �2.47D on the first day, and to �0.80D on the 28th day.
Corneal Staining We graded corneal staining in our study according to the Schnider system: grade 0 = the absence of staining and shows a situation in which the cornea wets well; grade 1 = diffuse light staining with no coalescence; grade 2 = light coalescence but the absence of fluorescein penetration into the deeper layers of the epithelium; grade 3 = marked coalescence with some deep penetration of fluorescein into the deeper epithelial layers; grade 4 = complete coalescence and extensive loss of epithelial cells.
We saw a high incidence of corneal staining in our study, most of which was grade 1 (Figure 1) or grade 2 after one night of treatment. On the 28th day, among eyes with corneal staining 36 percent were of grade 2 or grade 3. We did not observe any grade 4 staining in our research (See Table 1 and Figure 2).
|
TABLE 1 Incidence of Corneal Staining |
WITHOUT STAINING
Lens Positions The fluorescein pattern of the ideal lens fit is: base curve (BC) 4mm to 6mm central touch, fitting curve (FC) 0.5mm to 1mm ring of fluorescein pooling, alignment curve (AC) 1mm bearing and peripheral curve (PC) 0.2mm to 0.4mm ring of fluorescein pooling around the edge. The lens centers well and exhibits 1mm to 2mm of movement with each blink.
The lens is considered decentered when it overruns the limbus by more than 0.5mm and in these cases ring jam may appear on the Placido ring reflections on topography.
The lens fit is tight when it moves less than 0.5mm. An AC tight fitting lens central zone demonstrates fluorescein pooling, while in the entire tight-fitting lens the FC and AC fluorescein patterns are thin or even disappear completely. This may result in lens imprinting on the cornea. (See Figure 3 for an example fluorescein pattern of a tight-fitting lens.)
In our study some lens positions changed during the therapy though they were initially ideal. We found 79 lenses decentered on the 28th day (Table 2). The lens fit became tight in 148 eyes. Some were AC tight fitting, while in most cases the entire lens fit tight with lens fixation, central islands or ring jam (Table 3).
|
TABLE 2 Corneal Staining vs. Lens Position on the 28th Day |
|||
| CENTERED | DECENTERED | TOTAL EYES | |
| With staining [eyes (%)] | 91 (43%) | 40 (51%) | 131 |
| Without staining [eyes (%)] | 122 (57%) | 39 (49%) | 161 |
| Total eyes | 213 | 79 | 292 |
|
TABLE 3 Corneal Staining vs. Lens Movement in the 28th Day |
|||
| NORMAL MOVEMENT | TIGHT FITTING | TOTAL EYES | |
| With staining [eyes(%)] | 41 (29%) | 90 (61%) | 131 |
| Without staining [eyes(%)] | 103 (73%) | 58 (39%) | 161 |
| Total Eyes | 144 | 148 | 292 |
| *P≤0.01 | |||
Discussion
In accelerated ortho-k using one single-fit lens for each patient, the FC is 6.00D to 12.00D steeper than BC for the reverse curve. The BC creates a force to redistribute the epithelial cells from the center to the periphery during the treatment process, which we believe accelerates the speed of the myopia reduction.
In China, ortho-k lens designers do not observe patients' overall corneal shape directly, but refer only to the central curve and subjective refraction. However, we believe the corneal curvature (central and especially peripheral) varies in different races, regions and individuals, as do lid structures, blink patterns and tear quality, and these all affect lens position.
Therefore when lenses were designed and dispensed without considering these factors, or the lenses can't be modified or refit as necessary, they could easily become decentered or tight especially in cases of great reductions (>5.00D) or for flat peripheral corneas.
We found corneal staining in more eyes with decentered lenses than in those with centered lenses. The difference in corneal staining incidence between the normal lens movement group and the tight-fitting is significant. We speculate this occurs because the lens fits improperly and/or the Dk of the materials is not high enough.
Most
important in maintaining corneal health is supplying it with enough oxygen. The
tear film is the major source of oxygen for GP lens wearers. GP lenses supply
the cornea with oxygen by:
a. Tears pumped under lens with movement and b. Oxygen transmission through the
lenses.

|

|
| Figure 3. Note the bubbles under the BC zone and how the FC and AC widen and sharpen on this tight-fitting lens. | Figure 4. A case of corneal indentation exhibited by corneal topography. |
Therefore the exchange of tears under the lens and the lens position are important in maintaining the corneal oxygen supply. Research shows that while wearing GP lenses, the equivalent oxygen percentage (EOP) can or may decline from 15 percent to six percent under closed eyes, which is lower than the minimal physiologic needs of corneal oxygen supplies (10 percent).
In overnight wear therapy, the oxygen from air is cut off, the secretion of tears decreases and blinks are absent, leading to corneal hypoxia.
In accelerated ortho-k using a single-fit lens for all patients, when the amount of myopia reduction is large, and the lenses aren't refit according to changes in corneal curvature during the therapy, the lens can easily change to a tight-fitting one.
We believe the direct mechanical impairment from tight-fitting lenses and the toxic simulators of the metabolic by-products in the hypoxic condition cause corneal lesions. Also, perhaps even more seriously, tight fitting leads to lens fixation, which destroys the structure and stability of the tear film. Tear exchange under the lens is broken off, resulting in corneal edema and epithelium lesions caused by corneal anoxia, after which corneal staining appears.
|
|
|
|
Figure
5. A case of a warped cornea exhibited by the placido
disk of corneal topographer. |
Summary
The tendency of obvious improved unaided VA and the decrease of the subjective refraction shows that ortho-k is effective in reducing myopia. However the VA improvement alone does not mean that the whole process of ortho-k treatment is a success.
Also, the lenses changed position and corneal staining occurred during the procedure. Tight lens fitting is related to corneal staining. We suggest that a fitting trial and refitting are essential in maintaining a good visual outcome and corneal epithelium health. In the design of accelerated ortho-k, using a single-fit lens for all, the BC is 4.00D to 5.00D flatter than the flat K. Generally it can reduce 2.00D to 5.00D of myopia within a period of about two weeks to two months.
Ortho-k is an individual patient procedure. The lens position changes because of individual corneal variations, and this changes corneal shape during therapy even though it may have been optimal at first. So a detailed fitting trial and subsequent refitting are essential in maintaining good visual outcomes and corneal epithelium health.
We don't recommend the use of a single lens for ortho-k treatment. Whether we should use a higher Dk materials for overnight wear ortho-k treatment is also a serious consideration.
References are available upon request. To receive references via fax, call (800) 239-4684 and request document #96. (Have a fax number ready.)
Drs. Liao, Feng, Chen, Huang and Zhu are ophthalmologists at the First Affiliated Hospital of Sun Yat-sen at the University of Medical Sciences in Guangzhou, P.R. China, where Drs. Liao and Chen are also associate professor.