CORNEAL TOPOGRAPHY
Evaluating the Eye with Corneal Topography
Corneal topography shows more than a pretty picture. Different types of topography maps can help you better evaluate the eye's anterior surface and fit contact lenses.
By David W. Hansen, OD, FAAO
For decades contact lens practitioners used a 3mm central area of the cornea to select and fit contact lenses. Practitioners obtained this reproducible measurement with a crude instrument called a keratometer. To supplement our fitting skills and enhance lens fits, we used diagnostic lenses and sodium fluoroscein.
|
|
|
|
Figure 1. Dark areas on this axial map represent dry spots. |
|
Today, through the use of science and technology, we have gained an appreciation for measuring and evaluating almost the entire surface of the cornea through corneal topography. Why don't all practitioners embrace corneal topography? How can we use its information to help diagnose and treat clinical ocular problems?
Gary Powers, in his U-2 spy plane, systematically mapped the earth's surface over Russia in 1960. But it wasn't until the 1990s, 40 years later, that such advances in eye care helped us to measure the cornea. As Benjamin Franklin stated in his Poor Richard's Almanac in 1733, "He's the best physician that knows the worthlessness of the most medicines." Does this mean we should give up keratometry? I believe so.
Corneal topography provides central keratometry (Sim K) and much more. Franklin also stated, "This is old medicine and we need to move on to new science." I believe that corneal topography has risen to the gold standard in contact lens practice and ocular pathology. It is more than a pretty picture; its useful indices quantitatively and qualitatively interpret data to help diagnose and manage conditions affecting the eye's anterior surface.
Placido Disk Technology
Placido disk technology is currently one of the standards for measuring corneal curvature with topography. Doctors in the late 1800s used a series of concentric rings drawn on a target and backlit by the sun to evaluate the corneal surface. They observed the reflected rings with the naked eye and made subjective assumptions about the health and regularity of the ocular surface. Polaroid cameras and other methods of capturing light have revised and expanded this method, and the instrument became known as a photokeratoscope.
These early observations became important for advancing corneal measurements, and today topography maps display this corneal data. These two-dimensional maps use decoding colors that provide scales for measuring steep and flat areas to represent three-dimensional corneal curvature.
|
|
|
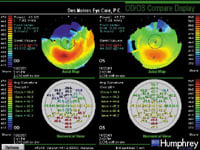
| Figure 2. Absence of data superiorly on this axial map indicates blepharochalasia and a need for blepharoplasty. | Figure 3. OD/OS compare map shows keratoconus fit with Rose K multifocal using numerical view data. |
Types of Topography Maps
All corneal topography nomograms and individual maps use thousands of data points to graphically present information. The different types of maps represent different data of the same corneal shape.
Axial Map The "sagittal" reading measures the curvature of the cornea in diopters and is called the axial or power map. Most corneal topography systems use this common map. It is a simple way to describe the overall shape of the cornea, and it actually calculates curvature rather than power. Placido ring configuration may limit periphery measurement. Despite the limitations, the axial map remains the most widely recognized map because it is easy to understand. Colors visually correspond to "flatness" and "steepness," which keratometry users know well. Figures 1 and 2 show examples of axial maps.
Tangential Map Tangential (instantaneous radius) maps are more sensitive. They calculate corneal curvature based on a "tangent to the normal." These maps best identify corneal pathology such as keratoconus (OD/OS compare display, Figure 3). Practitioners less frequently use dioptric power calculations from tangential maps to fit contact lenses or determine outcome analysis for refractive surgery.
Axial and tangential maps represent measurements of corneal curvature, not true corneal power. Central tangential maps show detailed patterns and they reveal a more exact location of a corneal defect when compared to an axial map.
|
TABLE 1 Specialty Lens Choices Based on Topography |
||
| TYPE OF ABNORMALITY | AVERAGE NUMERICAL VALUE | TYPE OF LENS |
| Keratoconus | 2mm average K | Rose K |
| Pellucid marginal degeneration | 4mm average K | Dyna Intra Limbal Lens |
| Post-graph or refractive surgery | 8mm average K | Post Graph lens |
Refractive Power Map This map accounts for spherical aberration and shows how light rays strike an aspheric surface such as the human cornea. Refractive power maps may differ from axial maps in calculating power and radius for the same patient. This results from the spherical aberration. Refractive power maps are most useful when assessing the visual performance of post-refractive surgery patients or the end result of refractive surgery (difference display).
Elevation Map The difference in the height or elevation of the cornea, measured in microns, from a reference surface determines an elevation map. Software programs attempt to superimpose the reference surface on top of the measured cornea. Measuring the corneal surface with small elevations or depressions provides a more detailed corneal assessment.
Irregularity Map This technique is much like the elevation map, but it uses the best fit toric surface as a reference. This eliminates any toricity from the eye and displays the elevation differences. The irregularity map measures the wavefront error, which closely matches a smooth-fitted toric surface (displayed as "normal"). The irregularity map quantifies and defines the most irregular areas of the corneal surface. Irregularity displayed as wavefront error helps quantify areas of distortion, which affect the quality of vision depending on location and size.
Photokeratoscopic View This picture uses the placido rings, which are reflected onto the eye, and subjectively determines the location and regularity of the rings. This view helps identify artifacts on the eye, such as the location of the central steepening in keratoconus.
Numerical View This map arranges individual keratometric findings to depict curvature readings of the eye. This view is extremely useful when fitting specialty contact lenses. Corneal topographic software calculates the "average keratometric" value. Table 1 indicates the initial GP lens designs I choose for various pathological corneas. I select the average keratometric numerical value as the base curve of the individual specialty contact lens, and I use this lens as the initial trial diagnostic lens.
Keratometry View This map represents the keratometric readings along the axes of the eye's presumed astigmatism. Dioptric values define the findings from the center of the cornea to the periphery. This view helps the practitioner quickly determine if corneal astigmatism is symmetrical.
Profile View This view graphically represents the individual axes of the cornea to help depict the three-dimensional nature of the cornea. It presents a side view of the major axes of the cornea and can help you determine if a toric contact lens is required. It can also present sodium fluoroscein patterns with a profile view to assist in contact lens fitting.
Statistical Indices in Corneal Topography
The following indices present a clear picture of the cornea and further assist the clinician when selecting the best contact lenses, detecting and monitoring changes in ocular disease and determining the potential for refractive surgery or orthokeratology (corneal refractive therapy). Understanding these statistical indices helps practitioners interpret the results when uncovering corneal irregularities and abnormalities.
Shape Factor Shape factor (SF) is the measurement of corneal asphericity, which helps determine whether a cornea is highly aspheric. When the cornea is less spherical or more elliptical in any meridian, it resembles a prolate shape. A negative SF usually indicates a post-refractive surgery eye with the center flatter than the periphery.
Eccentricity values are based on the mathematical description of an ellipse where 0.0 represents a circle with no flattening and 1.0 represents the maximum flattening in the periphery. Average corneas usually have an eccentricity of about 0.55 (e = 0.55). The SFs (e2) for the general population are as follows:
- Normal 0.13 to 0.35
- Borderline 0.02 to 0.12 and 0.36 to 0.46
- Abnormal 1.0 to 0.01 and 0.47 to 1.0
Different corneas may have the same central radius of curvature (Sim K or keratometry) but display a different rate of peripheral flattening or eccentricity. Therefore, if you choose base curves based on the central keratometric reading, you should know that peripheral flattening determines the contact lens-to-cornea relationship. If an eye demonstrates rapid peripheral flattening (e = 0.8, for example), it would produce a steep lens-to-cornea fitting relationship because the sagittal depth of the spherical lens would surpass that of the aspheric eye. Contact lens modules take these differences into consideration when they preselect the best contact lens to fit the aspheric cornea. These contact lens nomograms calculate the overall fitting relationship, the diameter of the contact lens, the optic zone and the peripheral curve configuration to determine the best contact lens fit. They may help you preselect a contact lens prior to the actual diagnostic fitting.
Corneal Irregularity Measurement The corneal irregularity measurement (CIM) is a number or index which represents the irregularity of the corneal surface. The higher the irregularity index, the more difficult it is to fit the corneal surface with a contact lens. It often can predict irregular astigmatism or visual distortions. Higher CIM values indicate that ocular pathology such as keratoconus or other pathological cases is more probable. The general population exhibits the following distribution ranges:
- Normal 0.03µm to 0.68µm
- Borderline 0.69µm to 1.0µm
- Abnormal 1.1µm to 5.0µm
Mean Toric Keratometry The mean toric keratometry (TKM) indices use elevation data to compare the toric reference to the actual cornea. The mean apical curvature value helps select the best toric fit using a sphero-cylinder design. This provides the most accurate toric representation of a patient's cornea. Human TKM ranges are as follows:
- Normal 43.10 diopters to 45.90 diopters
- Borderline 41.80 diopters to 43.00 diopters and 46.00 diopters to 47.20 diopters
- Abnormal 36.00 diopters to 41.70 diopters and 47.3 diopters to 60.0 diopters
Pathfinder Corneal Analysis The Atlas Corneal Topographer (Carl Zeiss Meditec, Inc.) uses special software that combines the above indices (CIM, SF and TKM) to determine the probability of irregular corneas. This helps practitioners qualitatively and quantitatively measure the probability of keratoconus (Figure 4). The Pathfinder Corneal Analysis also helps determine whether a GP or soft toric lens fits poorly on the cornea or should be replaced with a different base curve. It also helps when fitting GP lenses. New keratoconus fitting philosophies use a lens-to-cornea relationship with less central bearing. Trend with Time or Stars technology (Figure 5) can monitor corneal disease and determine how corneal shape responds with new contact lens designs.
|
|
|
Figure 4. Keratoconus (OD) determined with Pathfinder indicies. |
Figure 5. Healing Trend/Stars Map shows RK and post penetrating keratoplasty healing. |
Keratoconus and pellucid marginal degeneration (PMD) look similar on topography maps, so you must differentiate the true diagnosis to select the appropriate contact lens design. Typically, steepening with keratoconus is confined to a small centralized location whereas PMD corneas are usually diffuse and spread more over the entire inferior portion of the cornea (Figure 6). Corneal topography determines the location of this irregular pattern and helps differentiate degenerative corneal diseases.
In the early stages of keratoconus or PMD, a toric contact lens design may be more appropriate. You may even need a bitoric contact lens to improve visual acuity and comfort. As the disease advances, this corneal analysis program may indicate nomograms that select a keratoconus contact lens design such as Rose K. For PMD, it may select a specialty contact lens such as the Dyna Intra Limbal lens (Lens Dynamics, Inc.). Before corneal maps, no one used bifocal GP designs for these degenerative corneas. Now practitioners can design aspheric surfaces on the front surface of the contact lens and design the posterior surface for the overall disease process. This fitting provides a full complement of vision for far, intermediate and near. Patients who wear these sophisticated lenses gain new advantages for their overall visual health and visual clarity.
|
|
|
|
Figure 6. Overview map of pellucid marginal
degeneration. |
|
Corneal Map Qualitative Observation
The nomogram indices are extremely helpful for designing contact lenses and assessing corneal disease, but the qualitative map itself presents useful information. Absence of data points superiorly over one eye or both can indicate a blepharochalasis (dermatochalasis) or a ptosis condition of the eyelids. Combined with taped and untaped visual fields, this information may help determine the medical necessity for blepharoplasty surgery.
"White areas" on the maps may indicate a physiologically dry area of the cornea or a marginal dry eye syndrome. You may need punctal occlusion and/or lubricants for these patients to improve comfort with or without contact lenses.
Highest elevation indicators (a triangle on the Atlas Instrument) helps determine the overall position of the contact lens on the cornea. Posterior aspheric multifocal GP designs and other rigid lenses usually position over this area. It may not correspond with the steepest portion of the cornea and it may be positioned away from the pupillary axis. In our work with bifocal contact lenses (soft and GP), the highest peak on the cornea predicts the type of overall bifocal design. I have found that when the highest peak of the corneal map is centrally positioned, above the pupillary axis or to either side of the cornea, I can use either a translating or a simultaneous (aspheric) contact lens bifocal or multifocal design (Figure 7).
When the highest peak of the cornea is below the visual axis in the inferior portion of the cornea, a translating lens design usually works best. I usually use a truncated prism ballast lens when this highest peak is inferior because the contact lens tends to decenter inferiorly. Bifocal lens centration is extremely important, and corneal topography elevation helps reduce your preselection time.
Compression rings on the cornea usually present as "lined artifacts" that correspond to areas where the contact lens either adheres or is adjacent to the cornea and causes hypoxia. Compression rings can also be areas where the lens is required to touch the cornea, as in orthokeratology or corneal refractive therapy. For example, a paracentral inferior "smile" steepened area of the cornea indicates that an orthokeratology lens is superiorly positioned and will not provide the overall desired treatment necessary for long-term visual acuity.
Other pathological conditions such as vascularized limbal keratitis, pterygiums or pingueculae may distort areas of the cornea as a result of the overall disease process. Corneal topography can help you successfully change a contact lens to accommodate these areas.
|
|
|
|
Figure 7. OD/OS compare map shows that aspheric or translating multifocals will work because the highest peak is not
inferior. |
Benefits For Contact Lens Fitting
Most practitioners believe they can fit contact lenses without corneal topography and that topography is appropriate only for bizarre or diseased corneas. I believe this is incorrect. Corneal topography can help you fit almost any patient who desires to wear contact lenses, whether he is a previous wearer or a new prospect.
Are all 2.00D myopes the same? Why are some 2.00D myopes easy to fit and others more difficult? Why do some patients succeed with spherical soft lenses and others with aspheric soft lenses? Why do some patients need toric soft lenses or other designs to mask their refractive toricity? I believe corneal topography can help answer all of these questions. If we know more about the corneal surface before we initiate contact lens diagnostic fitting, we can reduce chair time, boost efficiency in the office, improve fitting selection and final lens performance with difficult and specialty fits and streamline the overall fitting process. Corneal topography can also establish an electronic link between the doctor and the contact lens lab, if necessary.
I also believe that although contact lens modules on corneal topography are not necessary for certain predictable cases, some patients warrant this software. As future instrumentation moves to wavefront error technology, which measures surface irregularity or distortion, it will allow us to more precisely predict overall success of contact lenses.
The U.S. gas permeable contact lens industry is scattered throughout the country, which prevents a single gold standard nomogram to establish a "best fit" design. But this is not all bad. Individual laboratories have distinctive lens designs for certain situations. If we can add this information to our individual corneal topographers, then this custom lens design package would facilitate lens fitting.
The simulated fluorescein pattern of the contact lens module must accurately depict the clinical picture of the contact lens on the eye. When this is the case, a corneal topographer can decrease chair time up to 50 percent compared to diagnostic fitting, according to a report about the EyeSys Pro-Fit contact lens program (EyeSys Vision).
Not All Topographers are Created Equal
Although corneal mapping technology has improved over time, no two instruments are alike. One study (Cho et al 2002) reported the performance of four corneal topographers on human corneas. Its conclusion reiterates the importance of good technique when taking individual patient information. The researchers reported that some instruments exhibited more accurate repeatability and reproducibility than others. They concluded that several repeated readings should be required for maximum repeatability for individual topographers.
The researchers also recommended that practitioners incorporate repeated readings as a matter of clinical routine to increase the chances of first fit success. They stated that individual contact lens parameters calculated from topography data depended on the topographer used and were not interchangeable between different topographers. Practitioners should also be aware that corneal topographic maps are informative in making a diagnosis, but other clinical information is required to diagnose a corneal problem.
Don't Limit Yourself
Corneal topography offers practitioners a wide variety of information, and practitioners should use topography to replace keratometry because of keratometry's limitations. This instrument can help practitioners with many anterior segment pathologies outside of contact lens fitting.
To receive references via fax, call (800) 239-4684 and request document #96. (Have a fax number ready.)