Contact Lenses and Complications
Hypoxic and infectious complications are the most preventable and most potentially severe adverse events.
By Charlotte Joslin, OD, FAAO
While many different complications can result from contact lens wear, the causes of most complications fall into five main pathophysiological categories: hypoxic, osmotic, mechanical, inflammatory or infectious. While there is overlap among the various categories, the primary inciting factor should be identified in order to most appropriately treat the condition. This article reviews the basics of hypoxic and infectious complications as they represent the most easily preventable and the most potentially severe adverse events.
Hypoxic Complications
Contact lens wear reduces the amount of oxygen to the cornea, especially under closed eye conditions. Numerous factors beyond individual variability affect corneal oxygen demand, which include pH, previous ocular history (including surgical and use of contact lenses), type of lens material and lens design. Complications can result if contact lenses result in inadequate corneal oxygenation given the patient's physiological demands and desired wearing schedule.
|
|
|
|
Figure 1. Mucopurulent exudate adherent to necrotic stroma in a Pseudomonas aeruginosa microbial
keratitis. |
|
In 1984, when Holden and Mertz determined the critical oxygen levels necessary to avoid corneal edema in normal eyes under daily and extended wear contact lens use, no contact lenses were commercially available that met the "Holden-Mertz criteria" for extended wear. Their criteria suggested an oxygen transmissibility (Dk/L) of 24.1 in daily wear and 87 in extended wear contact lens use to limit overnight corneal edema to 4 percent (the level experienced without a contact lens in place). More recently, Harvitt and Bonanno suggested transmissibility values of 35 for the open eye and 125 for the closed eye to prevent anoxia throughout the entire corneal thickness. While lenses previously approved by the FDA for extended wear have oxygen transmissibilities in the mid 30s, some of the new hyper oxygen-transmissible silicone hydrogels approved in 2001 by the FDA for 30 nights continuous wear have transmissibility values as high as 175. Hyper oxygen-transmissible silicone hydrogels and gas permeable lenses are expected to help prevent hypoxic-related complications not only in patients who use lenses for continuous wear, but also in daily wear patients with high oxygen demands and finally in healthy daily wear patients who want a soft lens that all laboratory and clinical data suggests is least likely to cause complications. Hyper oxygen-transmissible silicone hydrogels are now the only soft lens I prescribe in patients interested in extended or continuous wear.
Patients who wear lenses not providing enough oxygen to the cornea risk developing hypoxia. Common complications related to hypoxia include epithelial and stromal edema, increased bacterial adherence to epithelial cells, decreased epithelial cell regeneration, compromised epithelial junctional integrity, microcysts and vacuoles, endothelial polymegathism and bleb formation and corneal vascularization. Fortunately, most of these acute complications can be managed rather easily by changing lens materials. On a more serious note, hypoxia may play an important role in one of the most serious contact lens-related complications, microbial keratitis, which likely results from increased bacterial adherence to epithelial cells under hypoxic conditions. Note the disparity in the annualized incidence of microbial keratitis in soft lenses used for daily vs. extended wear (a more hypoxic condition): for daily wear, the annualized incidence is 3.5 per 10,000 as compared to 20.0 per 10,000 in extended-wear.
Infectious Complications
While all types of keratitis can present in contact lens wearers, two main types of ulcerative keratitis are associated with contact lens use. These are microbial keratitis (Pseudomonas aeruginosa, in particular) and Acanthamoeba keratitis. Both can have significant visual morbidity. Although other types of keratitis (viral, herpetic fungal, parasitic, etc.) can occur with contact lens wear, the frequency with which these types occur is generally not different between contact lens wearers and non-contact lens wearers. Differentiating early microbial keratitis from sterile marginal infiltrates, an immunologic response, represents one of the greatest diagnostic dilemmas, and errors in treatment and management can lead to potentially sight-threatening consequences.
|
|
|
|
Figure 2.
Neovascularization. |
While microbial keratitis, or an infectious corneal ulcer, is an infrequent event, sources for microbial contamination put all contact lens wearers at risk. Common sources of contamination include the environment, the wearer's hands (especially beneath the nail), the eye and ocular adnexa, a contaminated lens or lens case and contaminated solutions.
Clinical characteristics consistent with microbial keratitis include stromal infiltrates, anterior chamber inflammation, a decrease in visual acuity and significant subjective pain. Stromal involvement is usually central or paracentral, is diffuse and extends deep into the stroma (with the exception of early ulcers). Most of the time, an overlying epithelial defect is present, but this is not always the case. Culture-positive cases of microbial keratitis without the presence of an epithelial defect have been reported with both Gram positive and negative organisms. Other stromal changes present include corneal thinning (which can thin to perforation), edema, necrosis (Figure 1) or neovascularization (Figure 2). Dense corneal infiltrates can make assessment of the anterior chamber inflammation difficult, but cell, flare and hypopyon may be present and result in miosis and posterior synechiae.
Most "sight-threatening" infectious corneal ulcers are referred by optometrists and ophthalmologists to corneal sub-specialists for treatment and management. Management includes taking cultures and Gram stains initially, and then starting two different fortified antibiotics rotated every 30 minutes for the first 24 hours. Corneal ulcers that are "rarely sight-threatening" are commonly treated empirically with fluoroquinolone agents, and most resolve with broad spectrum therapy. The clinical characteristics that I use to distinguish an ulcer as "rarely sight-threatening" include the presence of each clinical characteristic: a corneal infiltrate less than 2mm in size and more than 3mm from the visual axis, and an anterior chamber response of 1+ or less.Keep in mind, however, that antibiotic resistance, even to fluoroquinolones, is increasing and is always a risk with empirical treatment.
The other type of keratitis in which the major risk factor is contact lens wear is Acanthamoeba keratitis. Acanthamoeba is a free-living amoeba that resides in water, soil and air, and it exists in two forms, an active trophozoite and a more resistant, dormant cyst. Both forms can adhere to contact lenses, which likely plays a significant role in Acanthamoeba keratitis as contact lens wear allows for easy transfer of the organism to the cornea.
|
|
|
|
Figure 3. Ring-shaped stromal infiltrate and radial keratoneuritis produced by Acanthamoeba
keratitis. |
|
Risk factors include contact lens wear (88 percent of patients with Acanthamoeba keratitis wore contact lenses), hard water as opposed to domestic soft water, irregular or inappropriate disinfection and a recent history of swimming with contact lenses.
Unfortunately, many contact lens disinfection products do not have appropriate amoebicidal effects, particularly for the resistant cyst form. Multipurpose solutions and two-step hydrogen peroxide systems, in which lenses are soaked in peroxide for four hours before neutralization, provided superior cysticidal effects, and rinsing appears to beneficial in trophozoite removal.
The classic clinical presentation of advanced Acanthamoeba keratitis is a ring-shaped infiltrate with severe pain and photophobia disproportionate with the clinical appearance. Early disease may present as a nonspecific keratitis and result in a delay in the correct diagnosis, as it is frequently misdiagnosed as other types of keratitis. Linear infiltrates may develop along the corneal nerves, known as radial keratoneuritis, and their presence is considered a hallmark of this disease (Figure 3). Acanthamoeba keratitis must be considered in any patient refractory to treatment or in the face of negative cultures.
Immediate diagnosis of Acanthamoeba keratitis and initiation of appropriate therapeutics is critical to maintaining good visual outcome. Cases in which the diagnosis and treatment begins within one month of the onset of symptoms result in less morbidity and better visual acuity. All potential cases of Acanthamoeba keratitis should be referred to a corneal sub-specialist for diagnosis and management. Acanthamoeba keratitis has traditionally been diagnosed through cultures, smears, and biopsy. More recently, confocal microscopy has been employed, as it provides a non-invasive method to diagnose the condition. Organisms can be seen in vivo in the epithelium and stroma, with the double-walled cystic form appearing as highly reflective, ovoid bodies approximately 10-25 microns in diameter (Figures 4 and 5).
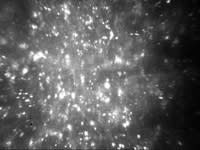
|

|
| Figure 4. Double walled, highly reflective Acanthamoeba cysts in the corneal stroma viewed by confocal microscopy. | Figure 5. Normal stromal keratocytes of the same patient in the unaffected eye viewed by confocal microscopy. |
| Courtesy of Elmer Tu, MD | |
Immune Mediated Complications
Inflammatory complications that result from contact lens use occur frequently. Common examples affecting the eye and lids include peripheral corneal ulcers (Figure 6), contact lens acute red eye, contact lens-associated superior limbic keratoconjunctivitis, giant papillary conjunctivitis and preservative hypersensitivity and toxicity reactions. Following a correct diagnosis, most of these are easily treated using techniques such as recommending lid hygiene, altering the lens fit or lens material, prescribing anti-allergy drops or changing care regimens. In cases of peripheral corneal ulcers, it is imperative to rule out an early microbial keratitis. Misdiagnosis of a microbial keratitis that is treated with steroids alone can cause a devastating result.
|
|
|
|
Figure 6. Contact lens peripheral ulcer. |
Mechanical Complications
Mechanical complications can range from subclinical to visually significant. All lenses can produce effects ranging from microtrauma to full-thickness abrasions, which put the contact lens wearer at a greater risk for infectious corneal ulcers. Other types of mechanical complications include corneal warpage, which is readily evident with corneal topography. All contact lenses, soft included, commonly produce mild corneal warpage, which may only be evident with corneal topography. No treatment is required for mild warpage unless it is significant enough to produce spectacle blur or result in unstable vision following contact lens removal. In patients interested in refractive surgery, it is imperative that lens wear discontinued until corneal warpage is resolved and serial topography is stable in order to reduce the risk of corneal ectasia following refractive surgery.
Osmotic Complications
Osmotic complications result from changes in the tonicity of the tear film, such as that which occurs following epiphora (hypotonicity) or in dry eyes (hypertonicity). Both hypotonic and hypertonic situations can alter the fit of a soft contact lens, usually creating a tight lens situation, leading to a continuing cycle of further compromise. Remedies include refitting the lens as necessary and treating the underlying cause of the osmotic complication (prescribing lubricants, inserting punctal plugs, etc.).
In conclusion, while we are fortunate today to have technology that provides for healthy contact lens wear in our patients, complications can and do occur. Three criteria are important to providing superior care to our patients: making sensible selections in lenses when prescribing; being suspicious of early signs of ocular compromise; and, appropriately educating patients how to avoid potential risks.
References are available upon request to the editors of Contact Lens Spectrum. To receive references via fax, call (800) 239-4684 and request document #xx. (Have a fax number ready.)
Dr. Joslin is assistant professor at the University of Illinois at Chicago Department of Ophthalmology and Vision Sciences.