WORLD OF CONTACT LENSES
Contact Lenses: Where Now and Where to?
Technology and the changing needs of the global contact lens population will determine the future of contact lenses.
By Brien Holden, PhD, DSc, OAM, Serina Stretton, PhD, Kylie Evans, BA, and Deborah Sweeney,
BOptom, PhD
Nearly 100 million people worldwide wear contact lenses 4 to 5 percent of the number that wear spectacles. Contact lenses are big business, worth over $6 billion at the supplier level, including accessories and solutions. The greatest number of wearers live in North America (36 million) followed by Asia (24 million) including Japan (14 million), and Europe (20 million). Asia, with its burgeoning middle class and more than 1 billion myopes, is likely catch up to North America within 10 years.
The years leading up to 2020 promise to yield an enormous increase in the global contact lens market through three main influences: product innovation, the rising number of people with myopia and presbyopia (up to an estimated 5.3 billion by 2020, over 60 percent of the then world's population) (Figure 1), and the demand from emerging markets such as China and India, by then well over 2.5 billion people, including at least 800 million myopes and 500 million presbyopes in these two countries alone.
The quality and scope of the products that we are able to develop will govern the number of contact lens wearers in that year.
|
|
|
|
Figure 1. Global trends indicate that the percentage of myopic and presbyopic people will rise significantly by
2020. |
|
Myopia and Presbyopia
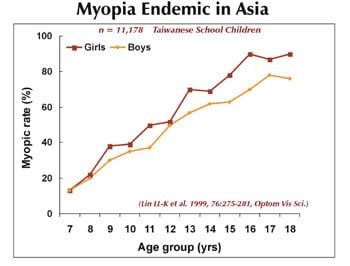
Over the last 30 years there has been a dramatic rise in the prevalence, severity and consequences of myopia (Figure 2). By 2020, over 2.5 billion people will be myopic. In developing countries, myopia has approached epidemic proportions; high myopia is the second leading cause of blindness in Asia. In Taiwanese children, for example, the incidence of myopia (0.25D or more) rose dramatically from 4 percent in 1986 to 16 percent in 2000, and the prevalence of myopia (0.25D or more) in school children aged 16 to 18 years rose to 84 percent (Lin et al 1999, Lin et al 2001) (Figure 3). In the Shunyi district of mainland China, 55 percent of girls and 37 percent of boys aged 15 have significant myopia (1.00D or more), and over 50 percent of all myopic children over 5 years have no form of vision correction (Zhao et al 2000). Although genetic factors can account for a proportion of the increase in prevalence of myopia, it is also clear that increasing urbanization, education and rising demand for near work are involved.
Myopia is not the only vision correction problem set to increase dramatically over the next 20 years. A sharp decrease in mortality rates and concomitant decrease in birth rates in almost all countries is dramatically changing the age profile of the world's population, and increasing the number of presbyopes. By 2020, the U.S. Census Bureau estimates that there will be more than 2,300 million people over age 45, with 1,750 million in the less developed countries. Asia in particular will bear a large part of the aging burden with 1,350 million presbyopes.
|
|
|
|
Figure 2. |
The striking increase in the number of myopes and presbyopes in developing nations such as China and India and the improving socioeconomic status of populations within these countries signals a huge demand for vision correction. A staggering 66 percent of the Japanese population will be presbyopic by the year 2020 (Figure 4). Contact lens companies cannot yet fully realize the great market potential of these emerging markets, but they need to invest, particularly in education, to capitalize on the rising proportion of middle- to upper-income earners within these countries. In addition, continuous wear with silicone hydrogel lenses will soon gain regulatory approval for the Japanese market. Although this market is traditionally very conservative, cost is usually not an obstacle to success. We expect that silicone hydrogel lenses will succeed in Japan because they fulfill the Japanese patients' demand for premium products.
High Dk: The Future Platform?
In August 2002, the Contact Lens Association of Ophthalmologists and the American Academy of Optometry brought together an international group of leading contact lens researchers to discuss the challenges, controversies and new opportunities for continuous wear lenses in the new millennium. The meeting focused on the potential of continuous wear as the future direction for contact lenses.
There has been a rapid recent increase in sales of high Dk soft lenses since they were approved for up to 30 days of continuous wear (CW) in Australia, in some countries in Europe (1999) and more recently in the United States (2001). In the United Kingdom, the percentage of all extended wear refits with silicone hydrogel lenses increased from 3 percent in 2000 to 12 percent in 2001 (Morgan 2000; Morgan 2001). In 2002 in Australia, Norway and the United Kingdom, more than 95 percent of all extended wear fits were with silicone hydrogel lenses (Woods 2002). Australia, usually a conservative market, currently has the greatest percentage of new silicone hydrogel fits (13 percent) and refits (40 percent) since they were released to market (Woods 2002).
|
|
|
|
Figure 3. Myopia is reaching epidemic proportions for children in
Asia. |
|
Silicone Hydrogels Generation 1: The Oxygen Platform
Current silicone hydrogel lenses exceed the critical oxygen transmissibility required to provide sufficient oxygen to the cornea during sleep. Evidence from both clinical trials and market experience demonstrate that the hypoxia-associated complications that occur with even daily wear of conventional or disposable soft contact lenses of lower Dk have been overcome.
This lack of metabolic stress means that contact lenses can be worn for hours, days, months and years without hypoxic complications. They are therefore capable of being worn by all ages and for all prescriptions if designs and surfaces can be produced to support the platform.
The development of hypoxia-free contact lenses is the first stage of releasing contact lenses from "bondage" as "specialty products," because the fundamental carrier allows normal ocular metabolism. This changes the issues that determine how many people, whether 500 million, a billion or more, can wear contact lenses to include: optics and vision, the success of contact lenses for presbyopia (controlling the mechanical behavior of lenses), biocompatibility, comfort, cost and their use in "new frontiers."
In practical terms this means:
- Can we eliminate infections and mechanically driven adverse events in CW mode?
- Can we create lenses that are truly comfortable when worn 24 hours a day for 30 days and nights?
- Can we lower the cost to the point where people can throw them away whenever they want to?
- Can we make multifocal contact lenses that always work?
- Can we use contact lenses to deliver drugs, diagnose and treat disease, prevent myopia and as permanent implants?
Future Silicone Hydrogels: Generation 2: Anti-MK?
Microbial keratitis (MK) is the only complication that can seriously impact the future of CW. So far 21 cases of microbial keratitis have been reported with silicone hydrogel continuous wear out of approximately 700,000 wearer-years around the world or one in over 33,000 wearer-years. Compare this to one in 500 in conventional extended wear (Poggio et al; Cheng et al 1999) and one in 4,000 with daily wear (Cheng et al 1999). No doubt there are more unreported, but the most closely followed and the worst case scenario at present is Australia, where eight MKs have been reported in 70,000 wearer-years, or one in 9,000. This still demonstrates a lower estimated risk with CW than with daily wear, but we must determine these figures accurately with proper studies. This is our most important current research need in assessing the true long-term potential of silicone hydrogels.
Another very encouraging finding is that as yet there have been no reports of loss of two lines or more of best-corrected visual acuity in any of these case reports (0 in 700,000 wearer-years), as opposed to one in 40,000 with modern daily wear (Cheng et al 1999; Nilsson et al 1994) and one in 100 with LASIK. Inevitably there will be cases, most likely due to improper use or treatment. We must take all possible steps to reduce the risk of MK with silicone hydrogels even further by:
- Making sure every patient
- Disinfects his lenses properly if they are out of the eye for any period of time
- Understands the warning signs of MK and what to do
- Receives rapid and proper treatment if a problem arises indicating MK
- Making sure that every eyecare practitioner knows how to treat suspected MKs properly ignorance of which was the major source of vision loss with low Dk MKs in the mid-1980s.
If MK has decreased by a factor of 10x or more with 30-night silicone hydrogel versus six-night wear of conventional or disposable soft lenses, and is equivalent to or better than daily wear, we have made good progress. But how can we lower risk by another order of magnitude?
One of the best ways to further reduce MK risk is to add anti-microbial properties on or in the contact lens. Strategies suggested include better wettability to "wash bacteria off" (polaxamer); bacteristatic surface additives (silver, selenium), bactericidal surfaces (surfactants, disinfectants) or anti-swarming, anti-growth surfaces (furanones). Ideally such a lens surface would discourage microorganisms from colonizing without killing them, which would eliminate the risk of both toxin release and resistance formation. Many companies are currently active in this area.
Unfortunately, no strategy will ever be foolproof. If a patient stores his contact lenses in a bacterial soup and then places them in his eyes, the risk of infection rises immensely. However, anti-bacterial surfaces and bulk additives have a real chance of making a difference not only with MK but with bacteria-driven adverse events, such as various forms of infiltrative keratitis.
|
|
|
|
Figure 4. Projections indicate that 66 percent of Japanese people will be presbyopic by the year
2020. |
Generation 3: Perfect Comfort
Can silicone hydrogels eliminate discomfort, the major reason for contact lens dropout? Can it be done? All day, all night, all month comfort? We can certainly get very close. If a patient applies the most comfortable lens in the world today, say a very well-designed, thick conventional soft lens, like some of the best plus torics available, it is very comfortable. But the comfort can't last; dehydration, hypoxia and deposits take their toll. If a patient applies a well-fitting silicone hydrogel lens, comfort may initially decrease slightly in some patients due to slight extra stiffness, but comfort improves with wear as the lens becomes "coated" and eventually outperforms the conventional hydrogel especially in drier environments. What we need is the best of both worlds. For perfect comfort in the future you need the best-designed, high Dk, most mechanically and physically appropriate material with superb biocompatibility. The key to achieving these prerequisites is better understanding. Generation 3 will require continuous improvements in design and performance and the ultimate in wettability and selective tear and surface interactions.
Back to the Present: Optics and Vision
Currently there is much hype about using custom ablations to reduce the horrendous aberrations resulting from spherical LASIK. Making aberration-free or aberration-controlled contact lenses is far less difficult. The future will know no other type of contact lens.
Astigmats and Presbyopes
Currently, silicone hydrogel lenses are available only for spherical prescriptions, but these materials have great advantages for toric and bifocal lenses in that thickness will not create physiological problems. Surfaces must be optimized to encourage ease of movement and reduce mechanical effects. The latest generation of well-designed disposable prism torics perform extremely well due to better location, consistency and comfort. Silicone hydrogel torics willneed to have the best designs possible to take advantage of the opportunity to provide good quality continuous vision for up to 37 percent of prospective lens wearers.
The proportion of contact lens wearers in different age groups takes a nosedive after age 45. No matter how you look at it, the $500 million spent over the last 40 years trying help presbyopes has been at best a limited success, at worst, a dismal failure. A small Australian laboratory, Gelflex Laboratories, has shown the way by reviving the translating bifocal soft contact lens. Again, silicone hydrogels could cope very well with required thicknesses if the surfaces and design are optimal.
Although GP contact lenses are generally acknowledged to have a limited market because of initial discomfort and soft lenses' easier fit, GPs are proven performers for astigmats and presbyopes. Successful GP wearers are exceedingly loyal to the modality.
Myopia Control with Contact Lenses?
High myopia affects not only quality of life, but also results in higher prevalence of ocular pathology, including increased risk of retinal detachment, cataract and glaucoma. High myopia is often bilateral, irreversible and affects individuals during their productive years causing more "blind years" (approximately 17 years) than diabetes, age-related maculopathy or glaucoma (five to 10 years). Any reduction in myopia progression will enormously benefit both individuals and the community. An effective strategy for reducing the progress of myopia would have global significance. The myopia epidemic in Asia has reawakened interest in accelerated orthokeratology to retard myopia progression in children.
There is no doubt that high Dk GP overnight orthokeratology does eliminate myopia, improve unaided vision considerably and eliminate the need for daytime correction for adult myopes. But the lessons from China and around the world show that even rigid lenses, long considered the safest lens modality, can produce a high rate of microbial keratitis if you combine PMMA, contaminated storage cases and closed eye wear.
Can ortho-k lenses slow the progress of myopia in children? Another fascinating subject. Results with conventional and GP contact lenses are equivocal, but the early ortho-k results are promising. Time and current studies will tell. One thing is certain: a myopia-controlling contact lens will cause a revolution in Asia.
Other Therapeutic Uses
Drug delivery, ocular diagnosis and other therapeutic uses have not yet been perfected with contact lenses, but current lower lens manufacturing costs will allow many new possible avenues.
Contact lens success could bring another remarkable development the low cost, high performance contact lens. At present our industry earns approximately $60 to $70 per head per year from 100 million lens wearers worldwide. With 1,000 million wearers at $25 per head per year, industry income would quadruple. Such market penetration through low cost, high performance products depends on concomitant developments in manufacturing efficiency for high Dk products, effective toric and bifocal lenses, continuous vision capability, safe and trouble-free lenses, availability of product in the most populous parts of the world and, that most elusive of goals, continuous excellent comfort. A tall order? Maybe, but the first giant steps have already been taken. The industry's vision and perseverance and the uptake of current breakthrough products will determine whether we will achieve the ultimate outcome.
References are available upon request to the editors of Contact Lens Spectrum. To receive references via fax, call (800) 239-4684 and request document #89. (Have a fax number ready.)
Prof. Holden is Director of the Cooperative Research Centre for Eye Research and Technology and the Cornea and Contact Lens Research Unit of the School of Optometry and Vision Science at the University of New South Wales, Australia.
Dr. Stretton is Scientific Writer at the Cooperative Research Centre for Eye Research and Technology, Australia.
Kylie Evans is Communications Manager at the Cooperative Research Centre for Eye Research and Technology, Australia.
Dr. Sweeney is Executive Director of the Cooperative Research Centre for Eye Research and Technology and the Cornea and Contact Lens Research Unit, Australia.