DRY EYE
Dry Eye Today
Current and new developments provide better chances for success in treating dry eye.
By Jennifer A. Barr, BA, and Joseph T. Barr, OD, MS, FAAO
Dry eye syndrome (DES) has been recognized as a leading reason why patients visit eyecare professionals in the United States. In fact, as many as one out of every five Americans is affected by symptoms of dry eye. DES may be even more common worldwide, and up to half of contact lens wearers complain of dry eye-like symptoms. It is believed to be a common cause of contact lens drop out.
The definition, etiology and treatments of DES remain a topic of concern for practitioners, researchers and manufacturers. Treatment is based on the intensity of the symptoms and/or signs.
Etiology and New Ideas
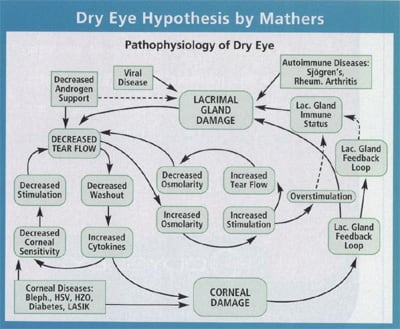
Dry eye symptoms result from inadequate quantity and/or quality of tears or ocular surface abnormalities. This lack of tears or abnormal tear quality deprives the eye of necessary nutrients and immune protection and ultimately could damage the ocular surface. Today it is believed, based on many histological and biochemical analyses, that increased inflammation resulting in further lacrimal gland damage and inability to produce tears is an underlying basis for DES (Figure 1, adapted from Mathers). Roslyn, NY, optometrist Art Epstein describes the "cycle of dry eye" as decreased tear production or increased tear evaporation or surface non-wetting, increased tear osmolarity and toxin concentrations, decreased goblet cell density, epithelium desquamation and destabilized tear film interface. Increased inflammatory mediators such as cytokines result in permanent surface (stem) cell and stromal matix damage and neurotrophic changes. Risk of infection increases with dry eye, and severe forms of dry eye can ultimately lead to loss of vision.
Classically, the precorneal tear film contains distinct lipid, aqueous and mucin layers. Today's theory is that the lipid layer covers an aqueous layer which gradually becomes thicker near the corneal surface as the mucins, or MUCs as they are now called, allow surface wettability and lubrication over the epithelial glycocalyx, the cornea and the conjunctiva.
|
TABLE
1: Contact Lens Solution and |
|
Complete Lubricating and Rewetting Drops and ClerzPlus (Alcon) PEG Refresh Contacts (AMO) Carboxymethylcellulose TheraTears Carboxymethylcellulose Complete (AMO) Poloxamer 237 and HPMC OptiFree Express (Alcon) PEG and Tetronic 1304 SoloCare Plus (CIBA Vision) BisTrisPropane/HPMC, PluronicF127, Aqualube/CremophorRH40 |
|
The new paradigm of dry eye models includes hormone control of the lacrimal glands, common control of the main and accessory lacrimal glands for both basic and reflex tearing and immune response or inflammation as an etiology of the dry eye. Estrogens and androgens are being tested to treat dry eye. Hormone replacement therapy (HRT) has been shown to both improve lacrimal gland function and cause more dry eye symptoms. The jury is still out on whether HRT affects dry eye.
Thus, the cornea and conjunctiva must be repaired or supplemented in order to reduce inflammation and keep dryness symptoms from occurring. Fortunately, new and improved as well as old diagnostic techniques support these new theories.
Diagnosis and Testing
Symptoms of irritation, burning, dryness and foreign body sensation, in the absence of other sources of inflammatory sensation such as allergy and infection, often make DES a symptom-based diagnosis of exclusion. Signs of redness, ocular surface staining, tear debris, reduced invasive or non-invasive tear break-up time, poor tear production as measured with Schirmer test or a tear prism height of less than 0.3mm are hallmarks of dry eye. Although methods to measure high tear osmolarity, immune system modulators, fluorophotometry and tear thickness with interferometry are used in modern tear research, clinical testing remains dependent upon case history and slit lamp signs.
To further test a patient's primary causes for dry eye symptoms, Dr. Epstein suggests the slit lamp examination as an important first step. "I look for corneal and/or conjunctival (fluorescein or lissamine green) staining as an indicator of dry eye-related surface damage," he says.
Risk factors for dry eye include dryness of other mucous membranes (Sjögrens syndrome), lid disease, acne rosacea, hormone imbalance, LASIK, thyroid disease, dry environments, contact lens wear and certain drugs (See Therapeutic Topics, the monthly column by Julie Schornack, OD).
|
|
TABLE 2: Contact Lenses Claimed to Minimize Dry Eye Symptoms |
|
Daily Disposable (Vistakon 1-Day
Acuvue, CIBA Silicone Hydrogel (CIBA Vision Focus Night & Day and B&L PureVision) Omafilcon (CooperVision Proclear) Extreme H20 (Hydrogel Vision Corp.) |
Prevention and Treatment
While many patients experience the dryness, redness, irritation, burning or excessive watering and tearing symptoms of dry eye, some people are more susceptible to these conditions based on their own lifestyles. Dry living or working conditions will increase symptoms of dry eye. Preventive measures can be taken within specific environmental conditions because these varying conditions can affect a patient's symptoms of dry eye.
Humidifiers can be added to an environment to keep moisture present. Patients who smoke or frequent smoky environments will be more susceptible to dry eye symptoms. People over age 65, post-menopausal women, computer users, people who live in dry, sunny, windy conditions and contact lens wearers will more commonly experience symptoms of dry eye. Many contact lens complications can be solved by teaching the patient to blink more consistently, avoid environmental stimuli and improve the home/work environment.
"Contact lens patients with dry eye are a subset of the general dry eye population," says Dr. Epstein. They may be dry eye patients due to the contact lenses, or they may be dry eye patients even if they do not wear contact lenses.
Contact lens wearers commonly develop dry eye because of the increased tear evaporation. "But not all dryness is the same," says Milton Hom, OD, in Azusa, CA. There are numerous causes of dry eye and therefore various treatments for managing these symptoms. Dr. Hom uses detailed questioning to diagnose the possible causes and determine the proper treatments.
|
TABLE 3: New and Future DES Treatment |
|
MUCOMIMETICS AND VISCOSITY AGENTS SECRETAGOGUES ANTI-EVAPORANT ANTI-INFLAMMATORY AGENTS |
|
Lid hygiene is the number one factor for preventing dry eye symptoms. Dr. Epstein begins by treating evident lid disease with warm compresses, lid hygiene and topical antibiotics if necessary. In some cases, oral antibiotics such as tetracycline or doxycyline may be needed to treat lid disease and improve tear quality.
Patients can prevent symptoms of dry eye by adding or subtracting nutrients from their diet. It has been suggested that dry eye patients avoid caffeine, artificial sweeteners and hydrogenated and trans fats. Avoiding red meat and refined sugars also has been suggested as a means to reduce symptoms of dry eye.
In addition to avoiding certain foods, doctors and patients have the option to add supplements and vitamins to possibly decrease dry eye symptoms. Cold-water fish such as salmon, cod, sardines, herring, trout and eel are all high in Omega-3 fatty acids that could restore moisture in the eye. Patients can take Omega-3 fish oil pills to obtain these nutrients. Those patients with fish allergies or who are vegetarian can add flaxseed oil to their diet for similar benefits. TheraTears Nutrition contains an Omega-3 supplement EPA- and DHA-enriched flaxseed oil and Vitamin E, and Ocusoft makes Hydrate Essential with flaxseed oil, evening primrose oil and bilberry extract. ScienceBased Health offers HydroEyes, a combination of Vitamin C, A, B6, mucin and magnesium as well as black current seed oil and cod liver oil as sources of Omega-3 and Omega-6 fatty acids, which they claim reduces prostaglandin productions.
Vitamins A and E may help to decrease dry eye symptoms because of their antioxidant activity. Water is a key nutritional factor when trying to reduce the effects of dry eye. Patients should consume half of their body weight in ounces of water per day on a regular basis (50oz per 100lbs)
Many treatments restore tear film that has been irritated or damaged so that symptoms diminish. Traditional drops and ointments may help resolve dry eye symptoms, but often offer only temporary relief. Artificial tears have been the mainstay of dry eye treatment, and ointments have given way to gels that change viscosity on the eye. These agents not only re-hydrate the eye, but help wash away inflammatory mediators. Most modern artificial tears contain electrolytes to maintain proper cellular function.
Contact Lens Care
Although some contact lenses dehydrate less on the eye, they do not necessarily decrease dry eye symptoms in head-to-head testing. Some patients are symptomatic with both high and low dehydrating lenses, according to Fonn and coworkers. Indeed, with all contact lenses, dryness and discomfort increased during the day of wear.
New contact lens solution development emphasizes eliminating the preservatives that aggravate the corneal surface of the eye. Contact lens solutions are manufactured to minimize preservative damage and provide more daylong comfortable wear. According to Dr. Hom, the emphasis for contact lens solutions has shifted from strength of disinfecting power to more comfortable and longer wear.
Ingredients such as hydroxypropylmethycellulose (HPMC) in Advanced Medical Optics' (AMO) Complete Solution act as a wetting agent and for dimulsification of debris. This solution is thicker than previous contact lens solutions and helps reduce evaporation that creates dryness. Aqualube and Tetronic 1304 were ingredients added to CIBA Vision's SoloCare Plus and Alcon's products, respectively, each of which performs similar functions (Table 1).
AMO's newest formulation, Complete Moisture Plus, has two new added ingredients: propylene glycol and taurine. Propylene glycol organizes water in the solution, lining up the charged molecules and allowing for better attraction to the lens surface, according to Dr. Hom. Taurine works as an osmoprotectant.
Says Dr. Hom: "Studies have shown that desiccation causes dryness symptoms and then creates corneal cell shrinkage or cell damage." He says that the uptake of taurine leads to less damage.
Various manufacturers also claim that their solutions' cleaning effects prevent dry eye symptoms. Caroline and Smythe have found more symptoms of dryness and corneal surface staining with ReNu MultiPlus as compared to AOSept. Indeed, some solutions may be better for some patients than others.
"Not all of our dry eye patients can wear contact lenses," says Kelly Nichols OD, PhD, from The Ohio State University College of Optometry. "However, some dry eye patients can wear contact lenses successfully while others have reduced wearing time." Keeping several different types of contact lenses available for patients can help patient success. She has learned that some contact lenses are better for dry eye patients (Table 2).
New Dry Eye Treatments
Most modern treatment strategies also target tear production and reducing inflammation (Table 3).
Systane, a new artificial tear from Alcon with HP Guar, decreases dry eye-related morning and end of day symptoms and foreign body sensation according to Alcon's studies. HP Guar combines with ocular surface glycocalyx to maintain stability and hydration. In a clinical study comparing Systane to another leading tear supplement, Alcon reports 51 percent reduction in corneal staining. The demulcent activity of Systane is like a "wet bandage," says Dr. Epstein.
Restasis (Allergan, 0.05% cyclosporin A emulsion) is recently available for anti-inflammatory treatment of dry eye. It prevents T-cell activation, which increases tear production. Restasis is dosed bid and is suspended in its vehicle, which is similar to Allergan's Refresh Endura tear supplement. Other tear supplements can be used 15 minutes before or after Restasis, and it is not absorbed systemically. Restasis should be instilled 15 minutes prior to contact lens insertion, if contact lens wear is approved by the prescribing practitioner.
Punctal plugs and punctual occlusion can be an option for dry eye, though return of symptoms and complications may occur. The Medennium (Smart Plug) is FDA approved and changes from gel to solid at body temperature. Alcon continues to develop the Intelliport, a liquid, injectable punctual plug system.
Conclusion
Careful case history to identify risk factors, testing tear stability and volume and examination for lid and ocular surface disease and inflammation are the mainstays of dry eye diagnosis. Proper selection of preventive treatments are the first line of treatment, followed by tear supplements, lens lubricants and lens care systems. New treatments for DES, including anti-inflammatory agents and secretagogues, will follow from the new research in dry eye.
Jennifer Barr is a freelance writer based in Dublin, OH.
Dr. Barr is editor of Contact Lens Spectrum and assistant dean of Clinical Affairs at The Ohio State University College of Optometry.



