ORTHO-K AND MYOPIA
Orthokeratology and Adolescent Myopia Control
This study set out to determine whether overnight wear of an orthokeratology lens would affect the progression of myopia in young people.
By Thomas R. Reim, OD, Max Lund, OD, and Richard Wu, OD
Ever since the 1960s, rigid contact lenses have been found to control myopia. Initially, these reports were anecdotal with few controlled clinical studies to either confirm or refute these claims. In the study by Morrison of 1,000 patients, he found that none of the patients showed any increase in myopia during the length of his study. More controlled studies have since been reported. Governson reported an increase in myopia in children of 0.48D over a three-year period using daywear gas permeable (GP) contact lenses. The control group of spectacle wearers progressed by 1.53D. A more recent study by Koo reported an annual increase of 0.42D for the GP group and 0.78D for the control group. Both studies suffered from a 50 percent dropout rate with poor comfort as the major reason. Some of the myopia reduction was attributed to an orthokeratology effect from the central cornea being flattened. Koo found a measurable amount of axial length growth inhibition in the GP group, so some mechanism is taking place, which is unrelated to the corneal orthokeratology effect. We wanted to see if the overnight wear of DreamLens for orthokeratology would have a similar effect.
|
|
|
|
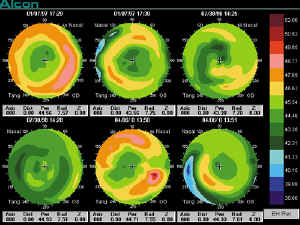
Three-year topographies for representative sample patient
JL. Age at stabilization: 13 years, 9 mos. Initial Rx: OD 2.000.75x90, 20/20; OS 2.000.50 x90, 20/20. Stabilization visit: 1/7/97; Rx: OD Pl; OS Pl. One year visit: 7/3/98; Rx: OD +0.25D; OS 0.25D. Three year visit: 4/6/00; Rx:OD 0.25D; OS 0.25D. Last visit: 5/31/01; Rx: OD Pl0.25x180; OS Pl. |
|
Methods
To see if orthokeratology does have any effect on myopia progression, we reviewed the records of 462 consecutive eyes fit with the DreamLens night wear orthokeratology lens between January 14, 1997, and March 20, 1997. Since this was a retrospective review of the records, carefully controlled data was not possible. We wanted to look only at adolescents, so all eyes over 18 years of age were eliminated. Patients had to have been seen at the three-month visit to establish a baseline refraction and then again at either the one-year or three-year mark to determine the amount of myopic progression. Many variables would skew the results, but we felt that we would get some idea about night wear orthokeratology and myopia. If the results were positive, then controlled studies could be initiated.
We did not look at the amount of myopia reduced or the range of treatment powers. Our only goal was the difference in refraction from a stable baseline and the refraction at one year and three years. At the one-month visit, most orthokeratology changes to the cornea had taken place and were stabilized by the three-month visit. Our assumption is that at the stable refraction at three months, any increase in refraction will be an increase in myopia progression. Of course there can be uncontrolled variability in the refraction from day to day, and patients might only return for their yearly and three-year visit if they are having trouble seeing. Patients who did not return for the three-year visit were not necessarily dropouts. Some moved away, and others will return when they notice a problem. If the base curve of a lens had to be flattened during the study period, the amount of flattening was considered an increase in the amount of myopia.
|
|
|
|
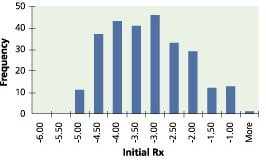
Rx
distribution pretreatment. |
Results
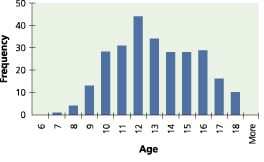
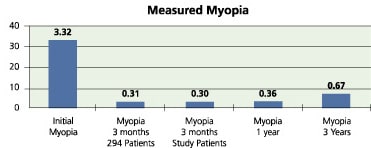
Of these 462 eyes, 350 were younger than 18 years of age. Some 294 eyes were seen for the three-month stability visit, 253 eyes were available for the one-year visit and 164 for the three-year visit. The subjective refraction at the three-month stabilization visit was used as the baseline for all refraction calculations. Only the sphere component was considered in all cases. Any changes in base curve after the three-month stabilization visit was considered an increase in the amount of myopia and was added to the refraction for the next visit. Some 60 percent were female and 40 percent were male with an average age of 12.5 years old with a range of 6.6 years to 17.8 years and a standard deviation of 2.5. The average initial refraction was 3.32D with a range of 0.50D to 5.25D and a standard deviation of 1.05. The average refraction at three months (294 eyes) was 0.31D with a standard deviation of 0.50 and a range of 2.25D to +0.50D. The average refraction for patients seen at the three-month stabilization visit (253 eyes) and at either the one-year or three-year visit was 0.30D with a range of 2.25D to +0.50D and a standard deviation of 0.45.
At the one year follow-up, the average refraction was 0.36D with a range of 3.00D to +0.50D and a standard deviation of 0.50. For the three-year follow-up, the average refraction was 0.67D with a range of 4.00D to +0.50D and a standard deviation of 0.78. At the end of the three-year period, the average increase in myopia was 0.39D with a range of 3.50D to +1.25D and a standard deviation of 0.76. The average increase in myopia over the time of this study was 0.39D or 0.13D per year, which is less than found by Koo and Grosverson and slightly more than Stone.
|
|
|
|
Age distribution at three-month
visit. |
|
Discussion
Previous attempts to study how rigid lenses affect the progression of myopia have been faced with various difficulties in study design. High patient dropout rates and the effect of corneal curvature changes are just two of the challenges encountered. The task of trying to find out if orthokeratology has the same effect as rigid contact lenses suffers from not only the same problems but also from determining exactly what the refraction really is. Successful and happy patients will not give up their lenses to allow the cornea to return to its natural shape. An over-refraction will show any increase in myopia, assuming that the original over-refraction at the three-month stabilization visit was plano and that the base curve of the lens has not changed during the study period. The advantage of an over-refraction in determining any increase in myopia is that it will neutralize any change in corneal curvature with the induced tear lens, implying that any increase in over-refraction will be due to an increase in myopia caused by the elongation of the eyes' axial length. In this study, neither an over-refraction nor axial length measurements were recorded. Orthokeratology can also vary from day to day, which will cause slight differences in the result. Patients also tend to come in only when problems present themselves, so many considered lost to follow-up are really not lost. They just are not having any problems and don't see the need to come in for follow-up.
The goal of this study was not to be a regimented controlled study, but rather to follow a large number of adolescents who were fit with an overnight orthokeratology lens to see if there appeared to be any effect on the progression of myopia, and if so to form the basis for a more controlled study.
The advantages of controlling myopia with an overnight orthokeratology lens over a traditional GP lens would be two-fold. First is comfort. Most patients who drop out of GP lens wear do so because of discomfort. Sleeping with the lens on the eye dramatically reduces lid interaction to the point where comfort has not been a problem.
The second advantage is good distance vision after lens removal and no correction required during the day. This is the major reason why adults choose orthokeratology, and it is a very compelling point for active adolescents. Parents like that they can stop worrying about their children breaking their glasses during their activities.
|
|
|
|
Average myopia at start, stabilization, one-year and three-year
visits. |
Conclusion
This study indicates that overnight wear of the DreamLens for orthokeratology has a similar effect on myopia progression as GP daily wear, as shown in previous studies by Stone, Groverson and Koo. Can you tell your patients that overnight wear of orthokeratology contact lenses will reduce the progression of myopia? No. You can say that studies indicate that GP lens daily wear may reduce the progression of myopia, and preliminary studies indicate that overnight wear of orthokeratology lenses has the same effect. These results clearly indicate that overnight wear of the DreamLens for orthokeratology has the same effect as GPs, but a controlled study must confirm this relationship.
You should give every adolescent who shows a progression in myopia and is within the recommended parameters the choice of overnight orthokeratology. No other procedure will provide the benefits of reduced progression of myopia along with freedom from glasses or contact lenses during the day.
Editor's note: Overnight orthokeratology is an off-label procedure in the United States at this time.

|
Dr. Reim is in private practice in Indian Harbor Beach, Florida specializing in orthokeratology. He is the inventor and patent holder of the DreamLens design for orthokeratology and has lectured extensively on orthokeratology both nationally and internationally. |

|
Dr. Lund has a large pediatric orthokeratology practice in Alhambra, Calif. and has been fitting the DreamLens since 1997. He is a well-known national and international lecturer on pediatric orthokeratology. |

|
Dr. Wu is currently the dean of the Taiwan Optometry school in Taipei, Taiwan and is finishing work on his PhD. He has lectured on orthokeratology extensively in Asia and Australia and is head of clinical research for the DreamLens in Taiwan. |