CORNEAL MEASUREMENT
Corneal
Diagnostic Technology
Use advanced diagnostics to improve visual
function and quality.
By Mohinder Mohan Merchea, OD, PhD, FAAO
The majority of long- or short-term contact lens wearers have no symptoms or complaints of compromised visual function or corneal physiology. However, we occasionally run into patients who present with reduced best corrected visual acuity, lens discomfort, reduced wearing time or signs of compromised corneal physiology. Often the causes of these symptoms are obvious, but we occasionally face symptomatic patients who have obscure clinical signs.
Standard instruments such as the slit lamp, biomicroscope and keratometer may not detect subtle changes in ocular structures. Therefore, using advanced diagnostic technologies may help elucidate causes of reduced visual performance or quality and intolerance to lenses or may quantify the effectiveness of a treatment.
|
|
|
|
Figure 1. Orbscan II analysis displays anterior and posterior corneal surface elevation maps, a traditional keratometric (tangential or axial) map and a pachymetry map. |
|
Surveying the Pachymetry Scene
Slit lamp-based optical pachymetry systems such as Haag-Streit's Optical pachymeter are predominately research-based instruments because they use a cumbersome measurement procedure and require substantial operator training. Additionally, various studies suggest that newer pachymetry techniques provide better interobserver repeatability than slit lamp-based optical pachymetry. Below are a few of the newer techniques.
Adding Ultrasound to Pachymetry The first instrument for measuring corneal thickness that was widely adopted in clinical settings was the hand-held ultrasonic pachymeter. An ultrasound pachymeter is comprised of a hand-held probe and a digital display console. The probe generates and directs ultrasound waves into the cornea and then detects the reflected ultrasound waves. The ultrasound waves are reflected when they cross between adjacent tissue layers, analogous to reflection of light rays passing between materials of differing refractive index. Ultrasound pachymeters assume the speed of sound through the human cornea to be about 1,640m/s. The pachymeter calculates thickness based on the time delay between reflected ultrasound waves.
Several corneal pachymeters are available, including the Sonogage CorneoGage Plus (Sonogage) and the DGH-550 Pachette 2 (DGH Technologies). These units use a 50MHz transducer and claim precision of 1µm to 5µm (similar to other high-frequency transducer systems). Other corneal pachymeters that have lower frequency transducers typically report precision to within 5µm to 10µm. However, clinical studies have determined the repeatability (95 percent limits of agreement) of hand-held ultrasound pachymetry to be about ±20µm. Pachymeters using transducers of 50MHz or higher measure epithelial, stromal and total corneal thickness.
Corneal thickness is measured by perpendicularly (about ±10 degrees) applanating the probe tip on a topically anesthetized cornea. Typically you should use the average of at least three ultrasound measurements in determining corneal thickness at any location. An advantage of ultrasound pachymetry is that you can easily train office staff to efficiently perform this procedure. Manufacturers of contact pachymeters recommend using a 70 percent alcohol swab to disinfect the probe after each use.
According to several studies on ultrasound pachymetry, the measurement procedure itself may influence the mean corneal thickness and variability observed because of possible compression of the corneal tissues being examined. Ultrasound pachymetry is further limited because it can measure only one region at a time, limited by the diameter of the applanation probe. You can use it to measure corneal thickness centrally or in peripheral locations, but it's more difficult to repeatedly locate the same peripheral corneal locations in serial measurements with hand-held devices.
An ideal instrument for measuring corneal pachymetry would have the ease of use of the ultrasound pachymeter and the non-invasiveness of the optical pachymeter. Two modern, non-invasive optically based techniques for corneal thickness measurement include partial coherence interferometry and slit scanning topography.
Modern Optical Pachymetry
The Orbscan II Anterior Segment Analyzer (Bausch & Lomb) scans, maps and displays the geometry of the anterior segment. It projects 40 slit images onto the cornea with equidistant angles from the optical axis through the entrance pupil of the cornea. A video camera coaxial with the optical axis records the images of the slits as they are scanned over the corneal surface. The Orbscan processes the images using an edge detection algorithm to determine the location of all of the edges that the slit beam strikes during the exam. The elevation of the anterior and posterior corneal surfaces is calculated using triangulation. Corneal thickness is then calculated by subtraction of the posterior surface from the anterior surface. The resultant thickness appears graphically in a colored map. The Orbscan II displays the regional averages in the central cornea and mid-peripheral quadrants, as well as the thinnest point measurement (Figure 1). The software allows you to calculate the average thicknesses in specified customized locations. This single instrument provides topographic and pachymetric measurements at the same time. Studies have reported the repeatability of the Orbscan for central pachymetry to be approximately ±6µm.
Another device for corneal thickness measurement that is available in international markets is the OLCR Pachymeter (Haag Streit), which is a slit lamp mounted non-contact corneal pachymeter that uses optical low coherence reflectometry technology. The slit lamp maintains perpendicularity of the measurement beam and the cornea. The OLCR Pachymeter uses a 100µm spot size generated from a 20Hz near infrared laser source. Haag Streit claims that the OLCR Pachymeter may be installed within an excimer laser system for intraoperative flap thickness or residual stromal thickness measurement after ablation. This instrument has the same limitations as ultrasound pachymeters in that it only provides single-point measurements. OLCR is similar to other ophthalmic (retinal) OCT devices, but it has been adapted to measure the cornea. OCT devices have been used for several years in research clinics to measure the corneal shape or tear film thickness, but no clinical OCT devices dedicated for corneal assessment have been marketed. Research studies have shown that repeatability of retinal OCT devices used for corneal thickness measurements is estimated at about 5µm to 10µm.
Ultrasound pachymetry has become a clinical gold standard because of its ease of use, but no evidence exists to suggest that it provides more in-vivo accuracy than optical techniques. In fact, optical techniques provide better inter-observer repeatability than ultrasound contact pachymeters. Ultrasound instruments typically report central corneal thickness measurements about 10µm thinner than either Orbscan or OCT derived measurements. This difference may result from the compression of corneal tissues by the ultrasound probe, but this explanation is debated. Regardless, Orbscan or OCT pachymetry measurements are highly correlated to ultrasound pachymetry measurements, but exercise caution when comparing ultrasound to optical measurements.
|
|
|
|
Figure 2. Confirmation that the patient is a keratoconus suspect. Midperipheral thinning is apparent in the inferior quadrant, with an inferiorly displaced thinnest
point. |
Pachymetry and Corneal Degenerations
In keratoconus, pachymetry can monitor the progression of the central corneal thinning that is associated with the disease. In subclinical cases or keratoconus suspects, where Fleischer's ring or striae are not evident, confirmation of corneal thinning may assist in diagnosis (Figure 2). In patients who have endothelial dystrophies, corneal swelling is frequently present in advanced cases. Pachymetry may help monitor progression of corneal decompensation and help in deciding to perform a penetrating keratoplasty. Orbscan II pachymetry is a valuable tool to assist in the diagnosis of peripheral thinning disorders including pellucid marginal degeneration.
Pachymetry in Continuous Wear
Traditional hydrogel lenses are known to cause corneal swelling beyond the normal physiological overnight level of four percent with continuous wear. However, slit lamp signs such as striae are typically not observed below eight percent swelling in the general population. But don't be surprised if a patient reports reduced contrast or clarity without slit lamp signs of corneal edema.
Corneal thickness measurement is useful in these patients to determine whether swelling is present and may provide an indication to switch to other hyper Dk lens materials or to discontinue continuous wear.
Pachymetry and Ortho-k
Researchers have also recently investigated the use of pachymetry in orthokeratology. Several authors have suggested that reverse geometry contact lenses flatten the central cornea and redistribute the corneal tissue to cause a shift in refractive error. It is hypothesized that the epithelium may be compressed centrally and squeezed into a midperipheral region. Other researchers have observed that the thickness profile of the stroma demonstrates a similar change.
In a clinical setting, the Orbscan II provides serial thickness measurements across the central and midperipheral corneal surface. Since it's also a topographer, you can determine the region of anterior corneal flattening and rule out any corneal swelling by monitoring the posterior corneal elevation topography map for change.
Pachymetry and Glaucoma
The Ocular Hypertension Treatment Study (OHTS) deemed essential the use of corneal pachymetry to diagnose and manage glaucoma and ocular hypertension. The investigators described central corneal thickness as a risk factor for progression of ocular hypertension to glaucoma, in addition to intraocular pressure (IOP), cup-to-disc ratios, race and visual fields. Goldmann assumed a central corneal thickness of 500µm when he described applanation tonometry, but failed to recognize the significant population variability of corneal thickness. In general, thinner corneas yield falsely low IOP measurements and thicker corneas yield falsely high IOP measurements. A high IOP with a thinner cornea would imply greater risk of progression to glaucoma than the same IOP with a thicker cornea.
The correlation between IOP and corneal thickness is not a simple linear relationship. However, several studies have described simple IOP correction factors in the range of about 3mmHg for each 50µm change in thickness. The OHT Study also showed that African American subjects had central corneal thickness values about 23µm thinner than Caucasians. These considerations indicate that corneal pachymetry is important in making an accurate diagnosis in a racially diverse population.
Measuring Corneas in the Surgical Setting
Refractive surgery candidates who have high myopia require a large amount of tissue removal, and knowledge of the exact amount of tissue available for ablation is critical. Many surgeons use ultrasound pachymetry intraoperatively to determine the measured flap thickness to more accurately estimate the amount of stroma available for ablation. Using this information, the surgeon can intraoperatively adjust the treatment zone diameter to maintain a safe residual stromal thickness.
|
|
|
|
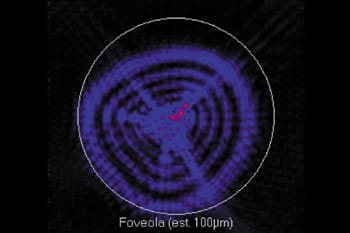
Figure 3. Higher-order aberration Zernike distribution for a
keratoconus suspect. Note that coma and trefoil have significantly larger magnitudes than other
HOAs. |
What's New? Wavefront Aberrometry
With the rapid growth of refractive surgery, we've become keenly aware of the implications of measuring aberrations to quantify the optical quality of the eye. Custom refractive surgery attempts to correct for an individual's specific preoperative aberrations by incorporating them into its calculated ablation profiles. The clinical aberrometer is a relatively new instrument that will continue to trickle down into everyday practice as we explore its diagnostic utility.
A wavefront aberrometer in is simplest form is a phoropter, an instrument with which we are all familiar. But more sophisticated and robust instruments are necessary to sample a patient's wavefront profile beyond sphere and cylinder. Clinically, the Hartmann-Shack type of wavefront sensor has been the most widely adopted aberrometer, but other technologies using ray tracing technology are marketed.
We typically sample a patient's wavefront pattern using a lenslet array to collect light reflected out of the eye. The Zernike Polynomial series mathematically describes the wavefront surface. The wavefront profile can be deconstructed into fundamental aberration components including the lower order aberrations defocus and astigmatism, and higher-order aberrations such as coma, trefoil and spherical aberration.
The magnitude of each Zernike term is quantified by its root mean square (RMS) error, which defines the deviation from a plane wavefront. In general, the population tends to have a slight amount of spherical aberration, while the remaining higher-order aberrations tend to have magnitudes near zero. However, patients are known to demonstrate individual variation from the population in any aberration term. Even with the best corrected spherocylindrical refraction, patients may report a poor visual quality.
|
|
|
|
Figure 4. Ocular point spread functions for a keratoconus suspect who complains of poor vision with a hydrogel toric lens. The left side displays the complete higher order
PSF, and the right side the PSF without coma or trefoil. This patient would benefit from a rigid
contact lens fitting. |
|
Diagnostic Aberrometry
Clinicians are often uncertain how to diagnose or best manage patients with mild topographical changes and slight reduction in visual acuity, but no other clinical signs of keratoconus. Often these patients report to the office for a refractive surgery consultation and it is important to measure the wavefront profile of these eyes to help identify a possible etiology. On average, keratoconus patients demonstrate a significantly higher magnitude of predominantly coma and trefoil (3rd order Zernike terms) compared to a normal population (Figure 3). Many of these patients wear toric hydrogel lenses and are still unable to achieve acceptable visual acuity. By examining the ocular point spread function (PSF) of these patients we see that if the 3rd order terms are neutralized a dramatic improvement in the point spread function is measured (Figure 4). For these patients, such a finding would indicate that a rigid contact lens may be beneficial.
Complaints of poor distant vision, ghosting, halos or glare are not uncommon with the use of high add powers for multifocals. The wavefront aberrometer can measure the effect of the optics of a lens on the eye's habitual aberrations while focused at optical infinity. If a large increase in the habitual aberrations are experienced with the lens on the eye, then try another lens design or a lower power add. In patients who have high magnitudes of spherical aberration, aspheric multifocal lens designs may result in poor visual quality, despite any improvement in near acuity. These patients would benefit from a translating lens design instead of simultaneous vision lenses.
|
|
|
|
Figure 5. Ocular point spread function for a
post-LASIK (high myopia) patient. Spherical aberration dominates the higher-order aberrations, accounting for severe glare and halo
complaints. |
Post-refractive surgery patients frequently visit optometric offices with complaints of halos, glare and ghost images even when Snellen acuity is acceptable. The cause of this reduction in visual quality may be related to the centration of the ablation, depth of treatment, flap complications or increased postoperative higher order aberrations (Figure 5). Although these symptoms are rare even in non-wavefront guided procedures they are serious and debilitating to patients. The wavefront aberrometer is valuable in educating these patients about the cause of their visual impairment and may indicate options for surgical or contact lens management.
Specular Microscopy
The development of the corneal specular microscope enhanced our ability to monitor the in-vivo integrity of the corneal endothelium. It allows us to quantify the degree of pleomorphism and polymegethism and has been available since the mid 1970s. Even now, we find most of these instruments in research or tertiary care clinics. Modern versions of the instrument are of the non-contact variety and can achieve the same or better resolution of their predecessors that required applanation of the microscope objective to the corneal surface. Most of today's specular microscopes are automated, require minimal training, provide improved patient comfort, avoid epithelial injury and minimize risk of infection. However, applanating specular microscopes provide better imaging in highly edematous or irregular corneas.
Some instruments provide images of the midperipheral cornea. The digitized image is analyzed using computer-assisted software to determine cell morphology, cell density or size and coefficient of variation (SD of mean cell area/mean cell area). In the normal adult human cornea, endothelial cell density measures in the range of about 2,000 to 3,000 cells/mm2. The typical coefficient of variation in healthy endothelium is about 0.25. The specular microscope is a valuable tool to determine the physiologic status of the endothelial layer by examining changes in listed metrics. Clinically, the specular microscope can monitor acute and long-term changes in the endothelium because of contact lens wear, particularly in low-Dk hydrogel continuous wear.
Redefining the Standard of Care
These technological advances are no longer limited to the research clinic or educational institution. In fact, you could include them as the newest additions to your ancillary testing rooms. These instruments have already started to redefine the standard of care for managing corneal disease and for providing the best visual quality to our contact lens patients.
References are available. Call (800) 239-4684 and request document #99. (Have a fax number ready.)