contact lens care
Phlyctenulosis: Another
Consequence of Noncompliance
BY SUSAN J. GROMACKI, OD, MS, FAAO
In the past two months, I have diagnosed four patients with phlyctenulosis. That's as many phlyctenulosis patients as I've seen in my previous 10 years of practice combined. The reason for the sudden increase remains unknown, but the patients shared two common characteristics: (teen) age and noncompliance with their contact lens care.
I couldn't place the blame on any single lens care system. Regimens included saline alone and ReNu MultiPlus Multi-purpose solution (Bausch & Lomb) without rub or rinse, and one patient shared her sister's Opti-Free Express (Alcon). The real culprits were the patients themselves.
|
|
|
|
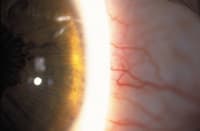
Figure 1. Bulbar conjunctival hyperemia in
phlyctenulosis. |
|
A Tricky Diagnosis
You may initially find it challenging to diagnose phlyctenules because they do not always manifest at initial presentation. Look for bulbar conjunctival hyperemia (Figure 1) combined with symptoms of mild-to-moderate tearing, irritation, foreign body sensation, pain or photophobia.
Phlyctenules present as small, raised, pinkish-white infiltrative nodules at the limbus that may subsequently develop on the bulbar conjunctiva or cornea. If corneal, the lesion may migrate toward the center of the cornea and produce a triangular pannus, which will eventually ulcerate and form a triangular scar at the limbus upon healing.
Use sodium fluorescein to confirm the diagnosis, as the phlyctenules will glow when viewed with the cobalt blue filter (Figure 2).
Phlyctenulosis results from a delayed hypersensitivity to staphylococcal antigens. Infrequently, it can result from hypersensitivity to tuberculoprotein, Candida, Coccidioides immitis, nematodes, lymphogranuloma venereum, adenovirus and herpes simplex virus. Phlyctenulosis may also be associated with ocular rosacea, most likely because of the common occurrence of staphylococcal blepharitis that manifests in patients with this condition.
|
|
|
|
Figure 2. Fluorescein staining of phlyctenules at 3:30, 4:00, 4:30 and
5:30. |
Treating Phlyctenulosis
Treatment is easy and effective. Prescribe a topical steroid (prednisolone acetate) or a steroid-antibiotic combination such as dexamethasone 0.1% / tobramycin 0.3% (TobraDex, Alcon) q.i.d. Add artificial tears if desired, lid hygiene if blepharitis is present and an antibiotic ointment at bedtime if severe. The eye should almost completely clear within one week.
Many patients report resolution after two to three days. Corneal phlyctenules may take longer to resolve (up to 10 to 14 days) and result in residual stromal scarring. Taper the steroid accordingly. If the condition recurs or if you suspect tuberculosis, order a tuberculin skin test (PPD) with anergy panel and a chest X-ray.
Dr. Gromacki has a specialty contact lens practice as part of a multi-subspecialty ophthalmology group in Fishkill, NY, and has served as a faculty member at the University of Michigan Department of Ophthalmology and Visual Sciences.