GP CARE
Improvements in the Care of GP Lenses
See what these practitioners discover when comparing two gas permeable lens care regimens.
By Barry Eiden, OD, Ed Bennett, OD, MSEd, Glenn Corbin, OD, Andrew
Cottingham, MD, Robert Davis, OD, Michael Greenberg, OD, MS, Kenneth Lebow, OD, Gary Meier, OD, Lee
Rigel, OD, and Evan Thomas, OD
Gas permeable (GP) contact lenses offer several benefits for contact lens wearers including better visual acuity, eye health and lens durability than most soft lenses. Moreover, GP lenses are often the only lens option for individuals who have conditions such as keratoconus, astigmatism and presbyopia.
On the other hand, GP lens wearers must adapt, not only to the feel of their often custom-fit lenses, but also to an essential lens care regimen that involves cleaning, conditioning, rinsing and rewetting. Improving the convenience of a GP lens care regimen while maintaining its safety and efficacy has the potential to enhance an individual's overall GP lens wearing experience.
This article describes a recent 90-day clinical investigation involving the subjective evaluation of two distinct lens care regimens by more than 200 GP lens wearers. In addition, the investigation assessed several clinical performance characteristics including lens deposition and wettability, as well as visual acuity and slit lamp findings.
The investigation provides evidence that a lens care regimen using Unique-pH Multi-Purpose Solution compares favorably to a more traditional lens care regimen, perhaps because of the marriage of a novel polymer system (HP Guar) that allows solution viscosity to vary with pH and a surface-acting agent (Tetronic 1304) that provides increased wettability.
|
|
|
|
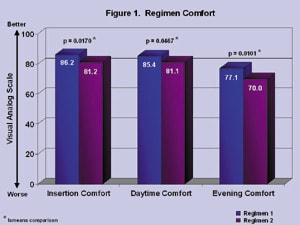
Figure 1. Regimen comfort assessed by visual analog
scale. |
|
Methods
Two hundred and eight individuals who had normal eyes volunteered to participate in a clinical investigation comparing the safety and efficacy of two GP lens care regimens. Each had worn fluorosilicone or silicone acrylate GP lenses and had used at least a two-bottle lens care regimen for at least one month before they participated in this investigation. No restrictions were imposed regarding subject age, gender, occupation or reason for wearing contact lenses.
The 90-day study required participants to visit one of 11 study sites for five visits including the lens fitting visit, baseline (Day 0), Day 14, Day 45 and Day 90, to evaluate one of two randomly assigned lens care regimens: Regimen 1 (n=103) using Unique-pH Multi-Purpose Solution with SupraClens and optional Clerz Plus rewetting drops, or Regimen 2 (n=105) using Boston Original Formula Conditioning System and Daily Cleaner with optional Boston Rewetting Drops (Table 1).
|
TABLE 1 |
||
| LENS CARE REGIMEN* | REGIMEN 1 | REGIMEN 2 |
| Disinfecting/Conditioning Solution | Unique-pH | Boston Original Conditioning Solution |
| Rinsing Solution | Unique-pH | Tap water/Boston Original Conditioning Solution |
| Daily Cleaner (manual) | Unique-pH | Boston Daily Cleaner |
| Enzymatic Cleaner | SupraClens Daily Protein Remover | None |
| Rewetting Drops (optional) | Clerz Plus Lens Drops | Boston Rewetting Drops |
| * all lens care products were masked to conceal their identity from patients and investigators. | ||
Regimen 1 incorporates lens care solution polymer technology in which the viscosity of the multipurpose solution adjusts to changes in pH. The solution also contains a surface-acting agent that adsorbs to the lens surface to provide increased wettability and lubrication. Regimen 2 represents a more traditional lens care regimen.
All participants first attended a lens fitting visit in which we assessed and adjusted their current lens parameters such that we could order an adequate number of appropriate lenses for the investigation.
|
|
|
|
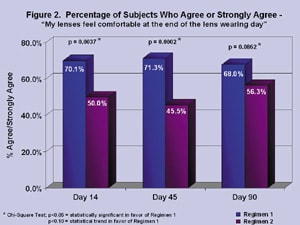
Figure 2. Regimen comfort at end of lens wearing day (Likert scale). |
On Day 0 we asked each participant to subjectively evaluate their pre-study lenses and lens care regimens using a 100-point visual analog comfort scale (Figure 1) and Likert scale questionnaire designed to assess performance characteristics such as lens comfort and satisfaction (Figure 2). We then dispensed each participant a new pair of study lenses for them to wear during the investigation. During this visit subjects also received visual acuity and slit lamp examinations before being randomly assigned to a regimen and given their re-labeled (masked) lens care products, the identities of which were unknown to both the patients and to the eyecare professionals conducting the investigation.
On each subsequent visit (Days 14, 45 and 90) we verified regimen compliance and again performed subjective and clinical evaluations. The investigators also noted any adverse events experienced by the participants during the preceding between-visit period (approximately two weeks at Day 14, four weeks at Day 45 and 6.5 weeks at Day 90).
Results
Using a visual analog comfort scale, participants who used Regimen 1 (Unique-pH) consistently reported significantly higher ratings of comfort on insertion (p=0.0170) as well as during daytime (p=0.0467) and evening (p=0.0101) wear. A significantly higher percentage of subjects who were assigned to Regimen 1 also agreed or strongly agreed to the statement, "My lenses feel comfortable at the end of the lens wearing day" on Days 14 and 45 (with a trend at Day 90) as compared to those following Regimen 2 (Boston).
|
|
|
|
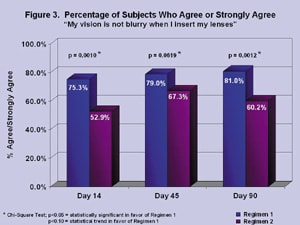
Figure 3. Subjective assessment of blurred vision. |
|
Additionally, more subjects using Regimen 1 agreed or strongly agreed with the statement, "My vision is not blurry when I insert my lenses" than did those using Regimen 2 (Figure 3). This difference was significant on Days 14 (p=0.0010) and 90 (p=0.0012), although only a trend for significance was found on Day 45 (p=0.0619).
In addition to these clear advantages over Regimen 2, the lens products used in Regimen 1 also compared favorably to the products the participants had used before the investigation. In fact, when asked on Days 14 and 90 of the study, Regimen 1 participants rated the convenience (p=0.0001, p=0.0001) and comfort (p=0.0015, p=0.0079) of Regimen 1 as significantly higher than the products they had used previously.
Subjective ratings of the Clerz Plus and Boston Rewetting Drops indicated that by Day 90 a significantly larger percentage of subjects felt that their contact lenses were more comfortable from using the Regimen 1 drops than did those using the Regimen 2 product (p=0.0358). Regimen 1 participants also significantly preferred the Clerz Plus rewetting drops to rewetting drops they had used before the investigation. In addition, a larger percentage of subjects who had a history of dry eye symptoms reported decreased symptoms with Clerz Plus compared to subjects using Boston Rewetting Drops.
|
|
|
|
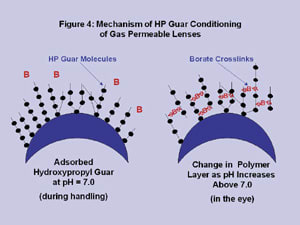
Figure 4. Mechanism of HP Guar conditioning of GP contact
lenses. |
Measurements of clinical variables such as lens film deposits, lens wettability, visual acuity and lens wearing time were similar between the two regimens on all study visits. This, in combination with a low incidence of product-related adverse events and few slit lamp findings, indicate the safety and clinical acceptability of both products.
Discussion
In this 90-day patient- and observer-masked investigation comparing the safety and efficacy of two GP lens care regimens, the 103 subjects using Regimen 1 reported several distinct advantages. Most notably, Regimen 1 was shown as statistically superior to Regimen 2 in ratings of comfort and convenience across all of the time periods assessed (insertion, daytime, evening and the end of lens wearing day). We found similar results when subjects compared the comfort and convenience of Regimen 1 products to those used before the investigation.
This comfort advantage afforded by Regimen 1 may be attributed to the novel polymer system and surface-acting agent that comprise the Unique-pH Multi-Purpose Solution. The HP Guar/borate polymer system (Figure 4) is less viscous at the approximately neutral pH present in the bottle and during handling; however when exposed to the slightly higher pH of the eye, viscosity increases because the formation of borate crosslinks between neighboring HP Guar molecules. This structural transformation renders the solution more viscous, cushioning the eye and perhaps increasing the comfort of GP lenses.
Moreover, as the viscosity of Unique-pH varies with tear pH, the solution becomes customized for each individual's ocular environment. Combining this polymer and the surface-acting agent Tetronic 1304 provides further cushioning and increased adsorption to the lens. And, although patients may be unaware of its effects, the patented antimicrobial agent in Unique-pH, Polyquad, provides safe and effective lens disinfection.
Finally, during the investigation, patient comfort was enhanced by the optional use of rewetting drops. The drops used with Regimen 1 (Clerz Plus) were subjectively superior to those used with Regimen 2 (Boston Rewetting Drops) as well as to those used by subjects before the investigation.
Although the products used in Regimen 2 were shown to be as safe and clinically effective as those used in Regimen 1, with similar ratings of lens deposits, wettability and visual acuity, the more traditional regimen was not as well received by the subjects in the study. These findings indicate that advancements in lens solution formulation technology can greatly improve a patient's overall GP lens wearing experience.
This study was sponsored by Alcon Laboratories.
Dr. Eiden is president of a private group practice specializing in primary eye care, contact lenses, and refractive surgery. Dr. Bennett is actively involved in the clinical investigation of contact lens designs, materials and care regimens. Dr. Corbin is an experienced clinical investigator for the pharmaceutical industry. Dr. Cottingham is a corneal-refractive surgery specialist in San Antonio. Dr. Davis is past chair of the Contact Lens and Cornea section of the American Optometric Association. Dr. Greenberg specializes in contact lenses and has been an investigator for numerous research projects. Dr. Lebow specializes in fitting advanced contact lens designs. Dr. Meier has been an investigator in contact lenses and contact lens solutions for more than 20 years. Dr. Rigel is a past chair of the American Optometric Association's Contact Lens Section. Dr. Thomas serves as an adjunct associate professor for SCO.