GP MULTIFOCALS
Pinpoint Success with
GP Multifocal Lenses
Learn basic guidelines for fitting all types of GP multifocal lenses and specific guidelines for fitting lenses in each design category.
By Robert L. Davis, OD, FAAO
Most articles about multifocal contact lenses begin with demographic information that shows how many presbyopes are in the marketplace. But demographics can't help you when a patient comes to your office requesting help with his near point demands.
I find that gas permeable (GP) multifocal contact lenses are the best optical design to correct reduced accommodative abilities that occur as the ocular system ages. Not only that, but with today's highly permeable GP materials, you can choose the appropriate polymer to match a patient's wearing habits.
This article will explain how to manage presbyopic patients through the GP multifocal lens fitting process as well as provide details of different GP multifocal contact lens designs and how to fit them.
Managing Presbyopic Patients
Communicate the ground rules as you begin a presbyopic patient/practitioner partnership. Inquire about vision, comfort, cost and convenience expectations to obtain an initial direction from the patient. If cost is an important issue, then begin with monovision. If convenience is an important factor, then consider an extended wear aspheric or annular GP design.
You will need to define vision and comfort issues as the fitting process reaches its conclusion. These parameters are difficult to test during the screening portion of the fitting process.
Refractive surgery has taught us that perfect vision is not necessary for success. A multifocal design does not necessarily have to meet a patient's visual goals all the time -- it only needs to perform for specific visual tasks during wearing time, which might be at work, during sport activities or just going out on the weekends.
Evaluate Before Fitting
Certain key observations during the screening process may simplify GP multifocal fitting. Examine the pupil size to help determine which bifocal modality will offer the best opportunity for success. When the pupil size is 5mm or larger, translating lenses will provide the best chance of success. If the pupil size is 5mm or less, the best option is an aspheric or annular design.
Evaluate tear quality and tear quantity to ensure that the lens can move on the eye appropriately and that the corneal epithelium has a cushioning layer to optimize comfort. Also evaluate the punctum for proper drainage. Large puncta can drain all the tears that are produced, culminating in dry eye symptoms. This often missed problem of excessive drainage creates 3 o'clock and 9 o'clock staining and mandates punctal occlusion. Hyperemia might be the only sign to signal distress when discomfort is not present.
Examine the lower lid position to help choose the proper lens design. If the lower lid positions significantly below or above the limbus, then an aspheric or annular bifocal lens is the best design option. Translating lens designs perform optimally when the lower lid positions slightly above, below or at the limbus.
Always check the "Bells Phenomenon" to avert improper lens movement resulting from torsional effects of the blink. GP contact lenses always move in the least restrictive pathway. If a cornea exhibits with-the-rule configuration, then the path of least resistance is in the vertical meridian and lenses will center in the vertical meridian. If a cornea exhibits against-the-rule configuration, then the path of least resistance is in the horizontal meridian. Contact lenses floating on an against-the-rule cornea will tend to decenter horizontally. The Bells Phenomenon describes the eye movement under the lid with the blink. Even though we can't see the lens movement underneath the lid unless we instruct the patient to blink while we hold their eyelids up, we should not underestimate the influence of this movement. If the lens moves in an unpredicted path, then look for an abnormal Bell's Phenomenon for your solution. Create better lens stability by making the lens or optic zone larger to solve this GP lens design difficulty.
Fitting GP Multifocal Lenses
All GP multifocal lenses have common fitting guidelines to help you attain a successful outcome. For example, when arriving at a final prescription, always adjust in 0.25D increments monocularly and select the least minus or most plus for the distance prescription. The smallest plus power adjustment can improve near vision without degrading binocular acuities. Perform prescription adjustments outside of the phoropter with the room illumination as normal as possible. The pupil will dilate behind the phoropter as well as when the lights are off, giving erroneous results.
Remember the examination room is not a patient's normal visual environment. Instead of using an acuity card, I often use a newspaper or ask patients to look around outside or bring their near point activities to the office to ensure that near vision is adequate. The real test occurs when patients go home and experience their new lenses in their own surroundings. The one-week follow-up visit should focus on remediating any visual difficulties they experience.
The following three simple rules summarize the key to fitting GP multifocal lenses.
Rule one: Determine the fitting relationship to sagittal height. If you increase lens diameter, then compensate by selecting a flatter base curve and adding plus to the prescription to offset the tear layer power. Reducing lens diameter reduces the sagittal height -- compensate by selecting a steeper base curve and adding minus to the power to counteract the tear layer power.
Rule two: Position the lens over the pupil to reduce flare/glare and enhance acuity. The lens will move up on the eye when you select a flatter base curve. A steeper base curve will cause the lens to move down.
Rule three: Select the appropriate zone size in an annular design to optimize vision. Increasing the distance portion of the optic zone will degrade near acuity. Increasing the near portion of the optic zone will degrade distance acuity.
Overall lens diameter has a relationship to base curve and sagittal height. A steeper cornea flattens quicker as it approaches the limbus, whereas a flatter cornea does not flatten at the same rate. Flatter corneas have lower eccentricities than steeper corneas because the amount of corneal curvature change is less in a flatter cornea as it approaches the limbus. Determine lens diameter from the base curve radius to optimize sagittal height. Flatter corneas require a larger lens diameter to offset the low eccentricity and improve sagittal height. Fit small lens diameters on steeper corneas that have higher eccentricity to maintain an optimum sagittal height.
|
|
|
|
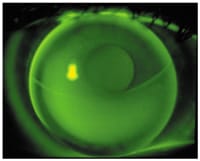
Figure 1. Most GP multifocal lens fits should demonstrate an alignment fluorescein
pattern. |
The lens fluorescein pattern illustrates the lens-to-cornea fitting relationship and helps you determine how to modify the lens design. A bright green area underneath the lens base curve indicates a space filled in with tears. This designates lens vaulting or apical clearance. Use a smaller lens diameter or a flatter base curve to reduce the sagittal height and create a more even amount of tears underneath the contact lens, which creates an alignment fit (Figure 1).
If the lens traps tears centrally and restricts tear movement in the intermediate zone, which creates areas devoid of fluorescein, this represents a bearing fitting relationship. To relieve the tourniquet effect in the mid-periphery, increase sagittal height in the intermediate area. If you want to maintain a constant sagittal height, then steepen the base curve by 0.25D when you reduce the optic zone diameter by 0.5mm.
Monovision: Still Going Strong
Monovision can consist of two spherical lenses or it can incorporate other multifocal design modalities such as aspheric, annular and translating lenses (modified monovision). Practitioners can choose from more than 20 GP multifocal lens designs in the marketplace. Monovision's advantage is that near and distance vision are independent of direction of gaze. Patients don't have to look down to translate into the near portion of the lens, and practitioners don't have to worry that the near zone may obstruct distance vision. I don't explain monovision to a patient before I perform a trial fitting because many patients find the monovision idea undesirable.
The monovision technique offers flexibility to choose the best lens designs that will produce a successful multifocal arrangement. Reduced depth perception and peripheral field vision have been controversial issues. Monovision does not reduce the extent of the visual field size, and the quantity of peripheral visual acuity does not decrease with monovision. Monovision limits central visual field suppression to three degrees. Peripheral field continues to contribute to binocular visual functions. Monovision does not affect motion detection, color recognition, light detection, reaction time and localization.
Fitting Monovision If one eye demonstrates reduced vision, then place the near lens on that eye because the plus power's magnification effect may compensate for the reduced acuity. If a patient has difficulty suppressing centrally, then add 1.50D over the distance prescription to help enhance central suppression. You must consider the distance, intermediate and near vision criteria when fulfilling a full range of vision with two lens powers. Initially, try not to blur the near eye more than 20/40. Add +0.50D to the distance eye and subtract 0.50D from the near eye to reduce the power separation between the two eyes, which is problematic to some patients. When adaptation becomes troublesome, try switching the far/near arrangement. Also, consider using modified monovision with one multifocal lens to satisfy the patient's visual requirements.
Aspheric GP Multifocals
Try aspheric GP multifocal lens designs first for early presbyopic patients. Aspheric GP designs are more comfortable than alternating, translating GP lens designs and it is easy to switch existing GP lens wearers into them.
|
|
|
|
Figure 2. Eye positions during straight-ahead and downgaze with aspheric GP multifocal
lenses. |
|
Aspheric GP multifocals provide excellent distance and intermediate visual acuity, and patients can achieve near vision correction by looking straight ahead. This design requires good centration and is unaffected by the lower lid position below the limbus. Higher add powers can't be incorporated into an aspheric multifocal design, but you can employ the monovision technique to offset the distance or near prescriptions as the patient ages.
Aspheric multifocal lens designs may cause corneal molding. The lens is steeper than the corneal surface and the eccentricity becomes greater as the add power increases. The rate of flattening induces a progressive increase in plus power as the cornea/tear/contact lens relationship changes in the downgaze position (Figure 2). The plus power tear film adds minus power to the prescription that is eliminated on downgaze. As the near portion of the lens positions itself, the pressure of the fitting relationship flattens the central corneal configuration and creates a steep configuration inferiorly where there is clearance between the cornea and contact lens. For high myopic prescriptions the lens mass increases in the periphery and creates a lid attachment scenario. In the plus prescription the edge mass is reduced, so you need a minus carrier to create a lid attachment fitting relationship. To counteract the effect of the prescription, design the lens with a lid attachment configuration with decentered optics or lenticularize the edge in a plus design.
Essential RGP multifocal (Blanchard), Lifestyle Gp multifocal (Lifestyle Gp), Tangent Streak no-line (Fused Kontacts) and Boston Multivision (Polymer Technology Corporation) are all commonly fit back aspheric lens designs that you should fit slightly steep with a superior-central position. A concentric zone on the front of these lenses can hold additional add power. These lenses are all similar, but slight differences make their designs unique to their names.
|
|
|
|
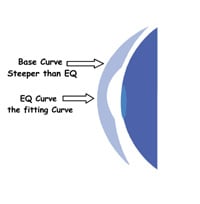
Figure 3. The Lifestyle Gp Multifocal uses two lens curves for presbyopic correction. |
The Lifestyle Gp multifocal features a multi-aspheric progressive add on the back surface of the lens. The equivalent (EQ) base curve or fitting curve fits on alignment and is flatter than the base curve. The base curve is approximately 0.16mm steeper than the EQ curve (Figure 3). The aspheric curves on the back surface provide approximately +1.50D of add power. The front surface's center-distance concentric bifocal area can range from 3.0mm to 6.0mm in diameter. You can put additional add power on the front surface of the lens to provide a total up to 3.00D of add power.
You can manipulate the front zone size to improve the quality of distance or near vision. Use a 9.0mm diameter lens for patients who have less than 1.50D of astigmatism when the EQ is 7.80mm or steeper. When the EQ is 7.90 or flatter, use a 9.5mm lens diameter. If a patient has 1.50D to 2.50D of astigmatism, use a 9.5mm diameter lens and for astigmatism greater than 2.50D, use a 10.0mm lens. Changing the base curve and adding the appropriate power can compensate for problems with distance or near vision. If the patient has distance visual inadequacies, then choose a steeper base curve and add 0.25D for every 0.1mm. You don't need to center the Lifestyle Gp lens, and you can create a translating bifocal design to take advantage of the concentric design on the front of the lens.
The Boston Multivision back aspheric lens fits near alignment and produces a multifocal add up to +1.75D during lens translation. The multiple aspheric curves on its back surface cause less corneal topographic change than steeper-fitting designs.
The Boston Multivision's distance curve is elliptical, whereas the near power is created by a hyperbolic curve. A fillet curve forms a transition zone that blends into an inverse geometry elliptical curve, which smoothes out to control tear flow and provides edge lift to inhibit lens binding.
Tangent Streak No-Line is a back aspheric bifocal lens design with add power up to +1.75D. This center distance aspheric bifocal uses a fitting base curve for an initial central curve selection. If the corneal cylinder is 1.00D or less, use a fitting base curve 0.50 diopters flatter than the steep K. If the corneal cylinder is greater than 1.00D and less than 3.75D, use a fitting base curve that is steeper than flat K by one third of the corneal cylinder. Use the true base curve, which is 0.16mm (about 0.93 diopters) steeper than the fitting base curve, to calculate the lens power.
Configure lens diameter to the fissure size. When the fissure size is 8mm to 11mm, use a 9.5mm diameter. When the fissure size is greater than 11mm, use a 10mm diameter. If the fissure size is less than 8mm, then a 9.0mm diameter is ideal.
Troubleshoot the design when the lens positions off center. An off-center lens usually provides adequate near vision but under-minused distance vision. Select a steeper fitting base curve to adjust a superior-riding lens. Adjust an inferior-riding lens by flattening the fitting base curve to resume a more normal central superior position.
|
|
|
|
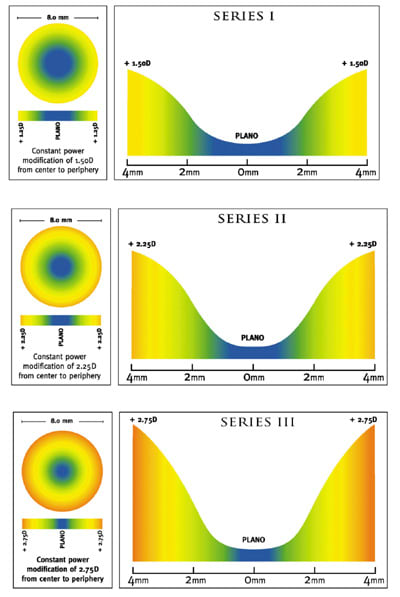
Figure 4. The Essential GP multifocal lens is available in three different near lens power
curves. |
|
The Essential GP Multifocal is a translating aspheric lens with low eccentricity to prevent corneal molding. The Essential GP Multifocal offers a series of three near lens power curves, each with a greater amount of add correction contained within a 4.0mm radius located centrally on the posterior surface (Figure 4). Series 1 incorporates a +1.25D power curve for near point work and is ideal for early to intermediate presbyopes. The distance portion of the optic zone is largest in this design. The Series 2 add is located closer to the distance zone and creates more power from greater eccentricity. Its power curves generate +1.50D to +2.25D for near work. The Series 3 add is located closer to the center of the lens and contains +2.50D of add power. The distance portion of the optic zone is smallest in this design.
The spherical central curve of the Essential GP Multifocal provides the distance correction. As the add increases, the near portion of the lens encroaches further into the central area of the lens. This provides more precise near acuity, but adversely affects distance vision. The S curve technology produces a flattening effect for greater posterior power gradient and a greater near point power effect. This design decreases sagittal depth to create the near power effect. Each lens series has a lower sagittal depth or greater eccentricity, which in turn creates a higher multifocal effect.
Fit the Essential GP Multifocal with lid attachment or intrapalpebral design philosophy with the goal of achieving an alignment fit. Select the diameter using the small/steep and large/flat paradigm. For lenses with base curves 7.30mm and steeper, use a 9.0mm diameter. Use the 9.5mm diameter lens for lenses with a base curve 7.4mm and flatter.
Configure the initial base curve by the amount of corneal cylinder and the flat corneal meridian. Fit the lens 0.50 diopters steeper than flat K for patients who have less than 0.75D of corneal cylinder. For patients with 0.75D to 1.75D of corneal cylinder, fit the lens 1.00 diopter steeper than flat K. For patients who have 1.87D or greater of corneal cylinder, use an initial lens 1.50 diopters steeper than the flat meridian.
Problems with this lens design result from inappropriate lens position. A high-riding lens will provide good near vision, but will over minus distance vision. In this case use a steeper base curve or a larger diameter to position the lens correctly. A lens that rides low will create good distance vision, but poor near vision. Flatten the base curve, use a minus carrier or increase overall lens diameter to position the lens more superior. A lens that rides nasal will generate poor distance and near vision. Increasing the lens diameter and/or adding a lens carrier to the lens design will solve this position problem.
High Eccentric Aspheric Lenses fit greater than 1.75 diopters steeper than K. The rate of flattening or eccentricity provides an alignment fit in the periphery that increases the add power for near vision.
The Metro Progressive (Metro Optics) features a 2mm central zone for distance vision. This zone also defines the base curve. The aspheric back curve begins at 2mm and continues to the periphery, increasing the add effect. The front curve geometry increases the near power by adding to the aspheric zone.
Depending on the amount of astigmatism, fit the lenses 1.75 diopters to 2.25 diopters steeper than flat K. The aspheric optics quickly flatten the lens fit away from the central 2mm zone. Strive for an alignment fitting relationship in the mid-periphery. In fitting the Metro Progressive lens steeper than K, you need to add minus to the patient's prescription because of the apical steepness.
Select lens diameter by the small/steep and large/flat rule. Select the 9.8mm lens for patients who have K readings flatter than 42.00 diopters. For patients who have K readings from 42.00 diopters to 46.00 diopters, use the 9.5mm diameter. Select the 9.2mm diameter for patients who have K readings steeper than 46.00 diopters.
If a patient develops corneal distortion-induced spectacle blur with this lens design, then try steepening the base curve by 0.50 diopters. A low-riding lens will blur distance vision, so select a flatter base curve radius and/or lenticular to improve lens position. When the lens moves excessively, increase the lens diameter or steepen the base curve radius.
Fit the VFL 3 High Aspheric multifocal lens (Conforma Contact Lenses) 2.00 diopters to 3.00 diopters steeper than flat K to create alignment in the intermediate and peripheral zones. The steeper-than-K base curve creates a small area of central clearance, which forms a plus tear layer that you can neutralize by adding an identical amount of minus power. Patients who have astigmatism greater than 2.00D and/or tight or narrow lid apertures may require a base curve steeper than that suggested.
Use the VFL Super Add design for presbyopes who require more than +2.00D of add power. This lens design incorporates the traditional VFL posterior surface with an annular progressive front zone. The Super Add VFL aspheric lens design is also pupil-size dependent, similar to an annular design. Make the front zone size 25 percent smaller than the pupil size in normal illumination for the best visual outcome. The average front optic zone size ranges from 3.0mm to 3.5mm.
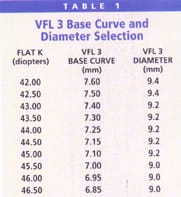
The VFL 3 lens, with or without the additional near power on the front surface, needs to center well for optimal distance vision. When the lens does not center well, translation occurs with each blink. Table 1 shows recommended base curves and diameters for this lens based on K readings. These lenses will ride high when they fit flat, have a thick minus edge or large diameter or if the patient has a small aperture. When the lens positions too high, poor distance vision results. To drop down a high-riding lens, you can steepen the base curve; use a lenticular plus carrier or apply a CN bevel to the edge; reduce the diameter or add prism base down. Lenses that ride inferior also result in poor distance vision. To raise a low-riding lens, you can flatten the base curve, use a minus-carrier lenticular or increase the diameter. Against-the-rule astigmatism or a too-narrow aperture may cause a lens to decenter laterally. To improve lens centration in this case, steepen the base curve and increase the diameter. If the lens positions in an oblique orientation, then steepen the base curve and increase the diameter.
Low Eccentric Aspheric Lenses all have similar fitting characteristics. Strive for apical clearance with intermediate alignment and moderate edge lift when fitting these lenses. The degree of eccentricity and steepness of the base curve creates the add power. Lenses fit steeper than K will display higher add powers, but they also have a greater tendency to mold the cornea. The material also influences the final add power because as the index of refraction increases, so does the effective add power.
Annular GP Designs
Annular GP lenses feature concentric areas of distance, intermediate or near powers. Concentric designs allow for greater add powers than the aspheric GP lenses. Annular designs may not cause the molding effect and ensuing specular blur often experienced with aspheric GP lenses. However, the concentric lens design can cause flare and glare if you don't optimize the annular zone size for the patient's pupil. The zone size is, in fact, the key for success in annular GP multifocal lens designs. A larger central distance zone provides better distance vision but degrades near vision quality. Conversely, increasing the size of the near zone in the periphery improves reading vision while degrading distance vision quality. The balance of the zone sizes determines success.
The Mandell Seamless Bifocal (Con-Cise) lens is a front surface, alternating, center distance concentric design. The distance and near annular lens zones are spherical, whereas the transition between the two zones is aspheric. The upper lid controls lens translation from distance to near vision.
Fit this lens with a base curve 0.25D flatter than flat K when the patient has no astigmatism. Fit the lens on K if the patient has 0.25D to 0.50D of astigmatism. For patients who have astigmatism greater than 0.75D, make the fitting base curve flat K plus one third of the difference between the principal meridians.
Lens diameter for the Mandell Seamless Bifocal depends on the lens position in relation to the pupil. For a large eye with an average pupil, use a 3.4mm distance zone in a 10.2mm overall diameter design. For patients who have a large pupil, use a 3.8mm distance zone with a 10.2mm diameter. For patients who have an average eye size or an eye with a small pupil, use a 3.4mm distance zone with a 9.8mm diameter lens. For a high-riding lens, the pupil requires a 3.8mm distance zone with a 10.2mm diameter.
If a lens rides high and the distance zone is above the pupil, then steepen the base curve or increase the diameter by 0.4mm to move the lens down. Adjust the distance zone to 3.0mm if the lens design provides good distance vision and poor near vision. If the lens design provides good near vision and poor distance vision, then check that the lens is centered properly. Order the lens larger and steeper if it decenters. If the lens centers properly, then order a lens with a larger distance zone.
|
|
|
|
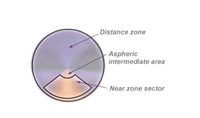
Figure 5. Newview 2 has a concentric
design and progressive add powers. |
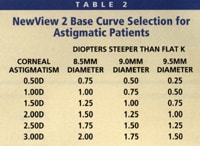
Newview 2 (Hydrokinetics) progressive additions lenses feature a front surface annular design with spherical distance and near zones separated by an aspheric intermediate zone (Figure 5). You can order the distance zone from four to six degrees in 0.5 degree increments, the near zone from 15 degrees to 22 degrees and the intermediate zone in aspheric step widths of three, six or twelve degrees.
The desired fluorescein pattern is central pooling with a bright outer circle. For patients who have flat corneas and against-the-rule astigmatism, add an additional 25 percent to the amount fit steeper than the flattest corneal meridian. Configure base curve selection according to Table 1.
The success of this lens design depends on the width of the power zones and the lens position on the cornea. The average lens has a five degree distance zone and a 17 degree near zone. If vision is variable, then increase the distance zone 0.5 degrees to one degree. If the patient has good distance and poor near vision, then move the near zone inward 2 degrees to three degrees, reduce the distance zone width and/or increase the add power. The patient experiences poor distance and near vision when the lens decenters. Bells Phenomenon may cause the lens to ride temporally. When the lens decenters, order the lens 0.50 diopters steeper or increase lens diameter.
The MagniClear Plus (Art Optical) lens is a front surface annular design with a 7mm distance zone, 0.5mm intermediate aspheric zone and a 1mm near spherical zone. It features a low eccentricity fitting curve on the back surface with an e-value of 0.5.
Fit this lens to result in a superior to central lens position. You should fit the lens slightly steeper than flat K. For patients who have corneal cylinder up to 1.25D, fit the lens 0.50 diopters steeper than flat K. For corneal cylinders from 1.50D to 2.25D, fit 0.75 diopters steeper than flat K. For patients who have greater than 2.50D of corneal cylinder, fit the lens 1.00 diopter steeper than flat K.
Diameter selection can range from 9.0mm to 10.5mm for optimal lens position. For corneas that are flatter than 45.00 diopters, use a 9.5mm lens. For corneas steeper than 45.00 diopters, use a 9.2mm lens. The distance zone needs to position centrally, in front of the pupil. Flatter corneas require larger lenses and steeper corneas require smaller lenses.
Translating GP Designs
Alternating, or translating, GP lenses typically feature a distance portion at the top and center of the lens and a near (and in some designs intermediate) segment in the lower portion of the lens. The segment line should position near the lower edge of the pupil in the straight-ahead gaze, so that the near segment does not interfere with distance vision. Translating designs need to move up, or translate, during downgaze to position the near segment in front of the pupil. They also need to drop down into correct position following the blink. For these reasons, fit the lens flatter for ease of movement and add prism ballast to the lens to help it drop down and to keep the near segment positioned at the bottom portion of the lens.
The most important ocular characteristics when fitting translating lenses are lower lid position and pupil size. Optimally, a translating lens should come to rest within 1mm of the lower limbus. Use the horizontal visible iris diameter to approximate lens diameter. If the lower lid is above the limbus, make the diameter smaller for proper near segment translation. If the lower lid falls below the limbus, then increase the overall diameter to help position the bifocal segment for reading. The segment must position high enough so that minimal translation in the vertical meridian provides patient satisfaction while reading. You can measure the segment line with a pen light. Observe the distance from the reflex to the lower lid and subtract l.3mm.
The lids play an important role in lens positioning and rotation. The upper lid helps rotate the prism on the eye. The lower lid stabilizes the translating bifocal and holds the lens in place as the eye looks down. Head position can also influence the position of the lens segment. If a patient normally positions his head with his chin elevated, then position the bifocal segment lower in the lens configuration.
You can configure translating lenses with a front or back toric design. These lenses perform best on with-the-rule eyes because the lens will follow the path of least resistance along the steeper vertical meridian. Patients who have against-the-rule corneas have a path of least resistance in the horizontal meridian, which causes the lens to decenter temporally or nasally.
The Tangent Streak (Fused Kontacts) is an executive bifocal with add powers from +0.75D to +3.50D. Position the segment height at 1.3mm from the lower lid to the visual axis. Fit the base curve 0.75 diopters flatter than K when the corneal toricity is less than 0.50D. When the corneal toricity is 0.50D to 1.00D, fit the lens 0.50 diopters flatter than K. If the corneal toricity is greater than 1.00D, then fit the lens one quarter the total toricity flatter than K. Choose the vertical lens diameter so that after truncation the distance between the top of the lens and the superior limbus is 2mm. Make the optic zone of this lens 75 percent of the horizontal dimension.
An important element of the Tangent Streak lens design is its truncation component. Use a 0.2mm truncation when the lower lid rests below the limbus. When the lower lid is tangent to or rests above the lower limbus, incorporate a 0.4mm truncation. Higher plus power requires less prism because of the center of gravity. More prism is necessary with higher minus power. If the prismatic lens rotates off the 90-degree alignment, then incorporate RALS (right add, left subtract): when the lens rotates to the practitioner's right, add the rotation amount to the 90-degree position. If it rotates to the practitioner's left, subtract the rotation amount from the 90-degree position for proper segment axis alignment.
If the patient complains of blurring at near, it could be because the segment is too low, the lens does not translate, the patient drops his head instead of his eyes or excessive lens rotation. If patients experience distance blur, then the lens is positioned too high, the bifocal segment is high or the lens moves excessively. If you observe excessive rotation, then you should flatten the base curve 0.50 diopter or increase the prism 0.50 diopter. When the lenses position too high, increase the prism 0.50 diopter or flatten the base curve 0.50 diopter. When the lens exhibits no translation, flatten the base curve 0.75 diopter, increase the prism or order the lens with a flatter peripheral curve radius.
|
|
|
|
Figure 6. The Presbylite lens uses three lens zones to
correct near, intermediate and distance vision. |
|
The Presbylite (Lens Dynamics) lens is a monocentric lens design with the optical zones cut on the front of the lens. It is a non-truncated lens design with 1.5 diopters of prism ballast. Its design incorporates a spherical distance zone, spherical near zone and a triangle-shaped aspheric intermediate zone (Figure 6).
Fit Presbylite on alignment with moderate peripheral clearance. Practitioners commonly make the mistake of designing Presbylite too flat for proper lens movement. A flat-fitting lens in this design causes the lens to position too high, resulting in blurred distance vision through the intermediate portion of the lens.
Choose lens diameter based on vertical iris diameter. Select the largest lens diameter that positions the segment below the limits of the pupil. The 9.6mm diameter allows the best translation for all visual ranges.
The Solitaire II (Tru-Form) is a translating GP contact lens design stabilized with non-truncated prism ballast. This monocentric design is cut with a prism in the near portion. The lens design is bottom heavy because weight is removed from the superior part of the lens. It incorporates a small aspheric zone for intermediate viewing on the front of the lens between the distance and near zones. Adds are available up to +3.75D.
|
|
|
|
Figure 7. The
Metro-Seg allows for 30
degrees of rotation. |
The Metro-Seg (Metro Optics) is an upsweep, translating, prism ballast bifocal lens (Figure 7). The back surface lens design features a well-blended aspheric secondary and peripheral curve, designed to fit on alignment. It allows for up to 30 degrees of rotation without affecting vision.
Position the segment 0.8mm below the geometric center or below the pupil margin for minus lenses. When the lower lid is at the limbus, place the bifocal segment 0.5mm below the geometric center for plus lenses. When the lower lid rests above the limbus, use a lower segment height. A segment 0.4mm below the pupil margin usually translates into success. Fit the Metro-Seg lens on K when the corneal toricity is 1.00D to 2.50D. With less than 1.00D of corneal toricity, fit this lens 0.25 diopters flatter than K.
When the lens and segment ride too high and distance vision is blurred, reduce the lens diameter, order a lower segment or truncate the lens. When the segment or lens rides too low, flatten the base curve and order a larger lens or order a higher bifocal segment. If the contact lens rotates more than 20 degrees, then reduce the lens diameter or truncate the lens. When the lens exhibits a slow lag time, order a steeper base curve, add prism or reduce the lens diameter. If the Metro-Seg lens moves excessively, then order a steeper base curve or increase the lens diameter. Fit a flatter base curve and a larger diameter if 3 o'clock and 9 o'clock staining develops. If a lens exhibits poor translation, truncate it to enhance contact lens movement.
Summary
Success with rigid multifocal lenses depends on choosing the appropriate lens design for the patient. Monovision lenses and aspheric GP multifocal designs are a good place to start for early presbyopes, and annular and translating designs allow you to boost patients' add power.
Remember to remove barriers from multifocal fitting. Patients want a seamless transition from their old lenses into their multifocal lenses. Use trial lenses to zero in on a patient's prescription as well as to allow the patient to experience different lens designs. Don't limit your multifocal contact lens selection. Finalize your lens design selection and manage a patient's expectations by learning how his visual system processes information. And finally, make sure you under sell and over deliver.
References are available upon request. To receive references via fax, call (800) 239-4684 and request document #98. (Have a fax number ready.)