MEDICATION SIDE EFFECTS
Medication Effects on the Anterior Segment and Contact Lens Wear
Some popular systemic medications cause ocular side effects that can disrupt contact lens wear.
By William L. Miller, OD, PhD, FAAO
Eyecare practitioners have long known that some medications adversely affect the cornea. For example, topical medica tions that contain thimerosol initiate a hypersensitivity red eye reaction in susceptible individuals. Some ocular side effects of topical and systemic medications are benign, but some are detrimental to the ocular surface and the eye in general and may affect contact lens wear.
|
|
|
|
Figure 1. Tear break-up found in dry eye
syndrome. |
|
This article will focus on how systemic medications affect the anterior ocular surface including the conjunctivae, cornea or lacrimal apparatus. Effects can include irritation, redness, dry eye syndrome (or keratoconjunctivitis sicca [k. sicca]) (Figure 1), or corneal deposition. Some systemic medications may also discolor lenses.
A careful review of patients' medications may reveal causative agents for anterior segment signs and symptoms. In addition, certain medications may interfere with successful contact lens wear. Prudently educating patients about adverse reactions from systemic medications and openly communicating with patients' physicians may ameliorate concerns related to their ocular surface disorder. Of course the risk-to-benefit ratio may dictate continuing a medication regardless of its effect on the eye.
Reactions from the Top 25
Table 1 lists the top 25 medications prescribed in the United States in 2002. Of these 25 medications, nearly 70 percent are associated with some ocular adverse reaction. Granted, many of the reactions occur infrequently (0.01 percent to 0.001 percent) or rarely (<0.001 percent), but a select group of your patients may exhibit signs and/or symptoms related to their systemic medications.
Adverse reactions among the top 25 medications include lid and conjunctival hyperemia, blepharoconjunctivitis, allergic conjunctivitis, non-specific conjunctivitis, xerophthalmia, k. sicca, conjunctival edema, peripheral corneal edema, corneal steepening, lens intolerance, foreign body sensation, increased mucin production and decreased tear lysozyme.
What you may blame on contact lenses may instead result from an adverse reaction from a systemic medication. This may be more of an issue in older lens patients who are more likely to take a systemic medication or multiple medications.

Side Effects by Medication Class
Following are common medications that affect the ocular surface and are likely to influence contact lens wear. I address each individual medication in its particular class, although some medications may be cross-referenced to more than one class.
ACE inhibitors Physicians commonly prescribe angiotensin converting enzyme (ACE) inhibitors for cardiovascular diseases that include congestive heart failure and essential hypertension. As a whole, ACE inhibitors can cause non-specific conjunctivitis as well as dry eye in certain individuals.
Antianxiety Medications Benzodiazepam derivatives can cause an allergic conjunctivitis that can manifest within 30 minutes after patients take it. These medications can also cause a foreign body irritation that lens wearers may confuse with contact lens irritation. This could result in contact lens intolerance or misplaced blame on the lens fit. Patients have also reported dry eye when using these medications. The two medications in this class that physicians most commonly prescribe are alprazolam (Xanax) and lorazepam (Ativan).
Antiarrhythmic Medications Quinidine (Quinaglute and Quinidex) may be associated with k. sicca and one report also links it to fine gray epithelial opacities. However, the causal relationship between medication use and reported adverse reactions is weak. Other cases of conjunctival hyperemia have also occurred with quinidine.
|
|
|
|
Figure 2. Corneal verticillata from
Amiodarone. Courtesy of Dr. Sara Brown. |
Another classic medication from this class that affects the cornea is amiodarone (Cordarone). It causes a bilateral and at times asymmetric phenomenon that is dose dependent. Nearly every patient who takes 400mg/day to 1000mg/day will develop corneal verticillata (Figure 2), but this rarely appears in patients who take 100mg/day to 200 mg/day. The verticillata represent deposits that appear grayish or golden-brown just anterior to the anterior limiting lamina. Patients typically will not complain of any symptoms, but if the deposits affect vision you can reduce or discontinue the medication to resolve the deposits.
A staging criterion (grade 1 to 4) exists to chart deposit progress and resolution. Early grade 1 changes are similar in appearance to Hudson-Stahli lines. Grades 2 through 4 demonstrate the more characteristic lines and whorl-like patterns. Their location suggests that ultraviolet light may play a role in enhancing deposition, which has led some to suggest using ultraviolet filters and possibly ultraviolet-blocking lenses.
Antidepressants Medications in this group may cause keratoconjunctivitis and non-specific conjunctivitis, both of which are infrequent adverse reactions. Antidepressants more rarely cause xerophthalmia or decreased levels of lacrimation. Two well-known medications in this class are sertraline (Zoloft) and paroxetine (Paxil), which were the 12th and 13th most prescribed drugs in 2002 (Table 1). Tricyclic antidepressants such as amitriptyline (Elavil, Endep) and doxepin (Adapin, Sinequan) also cause dry eye syndrome through their antimuscarinic action. Fluoxetine (Prozac) can also elicit k. sicca-like symptoms.
Antihistamines Antihistamine medications cause ocular dryness and decreased lacrimal secretion. Their antimuscarinic activity may decrease the aqueous component of the tear film. These effects occur mostly with over-the-counter (OTC) preparations and in some that have been recently moved to the OTC segment such as loratadine (Claritin). Newer, more site-specific (H1 selective) antihistamines like cetirizine (Zyrtec), desloratadine (Clarinex) and fexofenadine (Allegra) are less likely to cause ocular dryness, but they may affect the tear film although the effect is not as profound as earlier generation antihistamines.
Antihyperlipidemic Medications An increasing number of patients will take statins and antihyperlipidemics to reduce their cholesterol and/or improve their lipid profile. Atorvastatin (Lipitor) and simvastatin (Zocor) were 2nd and 17th in our most-prescribed list. Both medications are associated with dry eye syndrome.
Anti-infective Medications Unlike the previously mentioned drug classes, anti-infective medications typically treat acute disease processes and are not part of a chronic treatment regimen. Exceptions do exist, for instance in certain dermatologic conditions, but most are transiently prescribed. Most antibiotics cause no ocular surface problems and should not interfere with contact lens wear. Amoxicillin (Amoxil, Biomox, Polymox, Trimox and Wymox) along with others in the penicillin class, may cause blepharoconjunctivitis and Stevens-Johnson Syndrome.
Tetracycline (Achromycin V, Sumycin), doxycycline (Doryx, Vibramycin, Vibra-Tabs) and minocycline (Minocin, Dynacin, Vectrin) all have great dermatologic use in cases of acne. All are released into the tear film and can cause conjunctival crystalline deposits and result in or exacerbate ocular irritation in k. sicca or contact lens patients. In addition, tetracycline can cause a grayish-brown discoloration in soft contact lenses. This discoloration is rare today because increased numbers of patients wear disposable and planned replacement lenses.
Another medication that finds its way into the tear film and causes soft contact lens discoloration is the antituberculocidal rifampin. It usually discolors soft contact lenses and the tear film orange, but it can also discolor them pink or red. The antimalarial drug chloroquine, in addition to its effects on the macula, may cause a vortex keratopathy similar to that seen with amiodarone. Corneal deposition with chloroquine may interfere with vision or cause haloes.
Antipsychotic Medications When physicians frequently prescribe chlorpromazine (Thorazine) in high doses and for long periods of time, it can induce corneal changes. While 12 percent of patients who take 2000 mg/day show corneal signs, only one percent experience this corneal toxicity when they take 300 mg/day. Resulting pigmentary deposits are generally irreversible and affect the deep stroma, posterior limiting lamina and the endothelium. The corneal deposit pigmentation can appear white, yellow-white, brown or black and mostly within the palpebral aperture. The deposits rarely affect vision. Patients occasionally can become symptomatic, which may necessitate a change in dosage. Chlorpromizine may also cause a slate blue discoloration on the conjunctiva. Both chlorpromazine and thioridazine (Mellaril) also decrease secretion of the aqueous tear film, which may result in dry eye complaints especially in lens wearers. Thioridazine may also cause retinitis pigmentosa. Lastly, as a group, phenothiazines may discolor soft lenses grayish-brown.
Chemotherapeutic Medications A major drug in this class is cyclophosphamide (Cytoxan), an alkylating agent used to treat malignant diseases. As many as 50 percent of patients taking cyclophosphamide have developed k. sicca. Conjunctivitis and blepharoconjunctivitis may also result from this medication.
Dermatologic Medications In addition to the previously mentioned tetracycline class, isotretinoin (Accutane) occupies a prominent role in controlling recalcitrant cystic acne. It suppresses sebaceous gland activity within the skin, so it simultaneously affects the meibomian glands (which represent modified sebaceous glands) and results in adverse reactions that may make lens wear difficult. These reactions include keratitis, subepithelial corneal opacities and possibly corneal neovascularization. The suppressed meibomian glands cause enhanced surface evaporation that results in dry eye syndrome. Dry eye complaints will disappear, but this may not occur for several months after discontinuing the medication. Lens wear is difficult while patients take this medication. They may find relief through tear supplements, especially those that contain oils such as Refresh Endura (Allergan).
Diuretic Medications This drug class primarily causes decreased lacrimation, which may induce dry eye syndrome and hinder lens wear. Cases of non-specific conjunctivitis may also occur in patients who take these medications. Furosamide, hydrochlorothiazide and HCTZ/Triamterene are common medications of this class.
Physicians typically administer diuretics as maintenance therapy for edema in cases of chronic congestive heart failure, essential hypertension, renal dysfunction and pregnancy. One study (Bergmann et al 1985) did show decreased Schirmer strip results in patients who were taking hydrochlorothiazide. But it remains unknown whether this resulted from dehydration secondary to diuresis or whether it was truly a decrease in basal lacrimal production.
Gastrointestinal Medications This medication class includes proton pump inhibitors such as lansoprazole (Prevacid), omeprazole (Prilosec) and esomeprazole magnesium (Nexium) and H2 receptor antagonists such as ranitidine (Zantac) and cimetidine (Tagamet). Patients rarely report ocular symptoms that may interfere with lens wear, but susceptible patients on these particular medications may manifest dry eye symptoms when they wear contact lenses. H2 receptor antagonists can cause non-specific conjunctivides and sicca-like conditions. Proton pump inhibitors have caused dry eye complaints, although this does not appear in their individual package inserts.
Hormone Medications (Estrogen Replacement, Contraceptive Agents) Implicated in many dry eye states, this medication class profoundly affects the tear film and, as a result, contact lens wear. A great deal of information has become available about hormone replacement therapy in postmenopausal women. Schaumberg et al (2001) reported a 69 percent increase in dry eye symptoms in women who were taking estrogen replacement when compared to those who were not taking estrogen.
Additionally they reported that women who were taking a progesterone/progesterone combination also experienced a 29 percent increase in dry eye symptoms over those women not on therapy. Clinicians have also discussed oral contraceptives as agents responsible for decreased tear production and lens intolerance despite the fact that little proof of a causal relationship exists in cited literature.
One reference (Brennan and Efron 1989) did show increased dryness and irritation in patients who wore lenses made of HEMA and took oral contraceptive medications when compared to non-contact lens wearing patients. However, cause and effect remains unproven.
Narcotics/Analgesic Medications Propoxyphene napsylate (Darvocet-N) reportedly decreases tear secretion, which results in soft contact lens dehydration and an ensuing corneal abrasion (Bergmanson and Rios 1981). Hydrocodone/acetominophen (Lortab) can also cause dry eye conditions.
NSAIDs Most nonsteroidal anti-inflammatory drugs (NSAIDs) do not cause any adverse ocular reactions. However, indomethacin can cause corneal opacity formation. The lesions appear in the stroma as fine, whorl-like opacities, which may appear in 11 percent to 16 percent of patients. For most patients these opacities are benign and require no intervention. Because of the position of the opacities, they pose no problems for contact lens wear.
Herbs Herb use occasionally may cause eye irritation or redness. Dimethyl sulfoxide (DMSO) may cause burning eyes, and cases of non-specific conjunctivitis are known to occur with lily-of-the-valley (Convallaria majalis) and strophanthus. Cypress spurge (E. cyparissias) can cause corneal defects.
Don't Blame the Contact Lenses
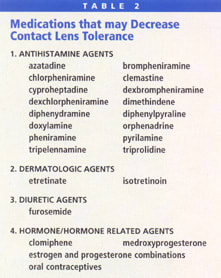
Many medications may play a role in adverse reactions in the conjunctiva, cornea and tear film. Some affect lacrimal secretion and the tear film, and may cause problems with lens wear. Other medications, cause a conjunctivitis response or conjunctival hyperemia that may prompt practitioners to blame the contact lenses rather than hold the systemic medication responsible. Table 2 lists other medications not covered in this article that may cause decreased lens tolerance. Practitioners should rule out all medication possibilities before concluding that contact lenses are the culprit of a patient's adverse reactions.
To receive references via fax, call (800) 239-4684 and request document #97. (Have a fax number ready.)






