contact lens case reports
Fitting Corneal Reshaping
Post-LASIK
BY PATRICK J. CAROLINE, FAAO, & MARK P. ANDRÉ, FAAO
|
|
|
|
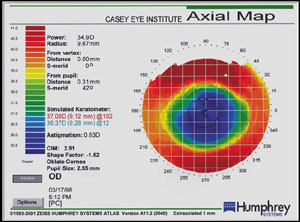
Figure 1. Corneal mapping
post-LASIK. |
|
The most common complication associated with modern refractive surgery is unplanned under- or overcorrection of the targeted refractive error. If the error is significant, then patients may undergo additional surgery such as laser re-treatment or conductive keratoplasty. However, if the residual refractive error is low, then additional surgery may not be in their best interest.
Considering Corneal Reshaping
Recent advances in GP corneal reshaping have shown that the procedure can safely and effectively remodel tissue in the central portion of the cornea to correct myopia (corneal flattening) and hyperopia (corneal steepening). For a number of years, anecdotal reports have indicated that effective corneal reshaping may be possible following refractive surgery.
|
|
|
|
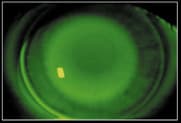
Figure 2. Reverse geometry lens
design with apical clearance. |
Patient DF, a 38-year-old male, underwent bilateral LASIK in February 1998. His preoperative refractive error was OD 5.50 1.25 x 010 and OS 5.00 1.00 x 180. Postoperatively, his manifest refraction was OD +2.75 0.75 x 005 20/20 and OS +0.50 0.25 x 180 20/20. Simulated keratometric readings on the right eye were 36.37 @ 012/37.00 @ 102 with a central apical radius of 35.00 diopters (Figure 1).
We fit DF's right eye with a reverse geometry GP lens with a central base curve radius of 37.00 diopters and the mid-peripheral fitting curve equal to the radius of curvature 4mm from center on the temporal side of the cornea (40.50 diopters). The combination of curvatures resulted in a lens that moved and positioned well on the cornea, and the fluorescein pattern revealed significant apical clearance (Figure 2). We dispensed the lens to DF and asked him to return in one week.
Lost and Found
|
|
|
|
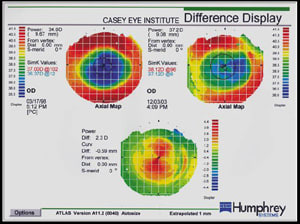
Figure 3. Difference display map showing 2.37D of corneal
steepening. |
|
We lost DF to follow up, but he reappeared in December 2003. He'd worn the lens on a daily wear basis for approximately two years, then discontinued wear because his unaided VA had significantly improved to 20/20.
Videokeratography revealed that his central cornea had steepened, with simulated Ks of 37.12 @ 006/38.12 @ 096 and an apical radius of 37.25 diopters. The difference display map shows the 2.37D of central steepening that occurred from 1998 to 2003 (Figure 3). Whether this resulted from normal post-LASIK regression or from the inadvertent apical clearance lens design, we'll never know.
Patrick Caroline is an associate professor of optometry at Pacific University and is an assistant professor of ophthalmology at the Oregon Health Sciences University. Mark André is director of contact lens services at the Oregon Health Sciences University and serves as an adjunct assistant professor of optometry at Pacific University.