OCULAR ALLERGY
Ocular Allergies: Reviewing Etiologies and Treatment Options
Allergy season is a perfect time to review the etiologies, signs and symptoms of ocular allergies and how to help your patients find relief.
By David A. Berntsen, OD
Spring is upon us, and as Mother Nature begins to bloom, allergy season raises its itchy head. An estimated 25 percent of Americans suffer from allergies, with 60 percent of this group experiencing some level of ocular symptoms. This represents a population of 60 million patients who would benefit from ocular allergy treatment, including many of your contact lens patients.
With the vast number of prescription treatment options available, you're doing your patients a disservice if you let them choose "any old" over-the-counter (OTC) allergy drop. I'll discuss different treatment options later on, but to best manage patients who have ocular allergies, you must first understand the potential etiologies and underlying mechanisms.
What Causes Ocular Allergies?
Ocular allergies result from the immune response triggered by a previously encountered antigen. A multitude of antigens can trigger an allergic response, including seasonal culprits such as pollen and perennial agents such as dust, mold and animal dander. Type I and Type IV hypersensitivity responses account for the majority of ocular allergic reactions.
Type I Hypersensitivity Type I responses are associated with perennial and seasonal allergic conjunctivitis (SAC) and atopy, the genetic predisposition to environmental allergies.
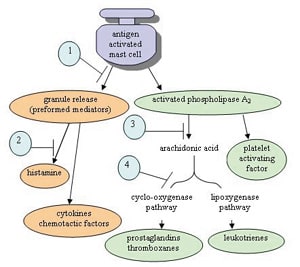
Immunoglobulin E (IgE) mediates Type I responses, which are immediate. When an antigen binds to an IgE receptor on the surface of a mast cell, it triggers a cascade that causes the mast cell to degranulate and release preformed inflammatory mediators such as histamine (Figure 1). Histamine increases vascular permeability, which causes edema in the surrounding tissue and yields the puffy, itchy, red eyes that signify ocular allergies.
The cascade that causes mast cell degranulation also activates the enzyme phospholipase A2, resulting in arachidonic acid release. This branch of the response results in the formation of newly synthesized inflammatory mediators, such as prostaglandins (via the cyclo-oxygenase pathway) and leukotrienes (via the lipoxygenase pathway).
Type IV Hypersensitivity T cells mediate these delayed responses, which can take days to reach full intensity. Exposure to an antigen initially results in differentiation of naïve T cells. Upon the second presentation of the antigen to now sensitized T cells, a cytokine-mediated inflammatory response initiates that results in macrophage migration and activation.
Allergy Treatment Basics
For patients suffering from a mild allergic response, cold compresses and artificial tears can help alleviate symptoms. However, if you ignore the underlying causative mechanism, then your patients may self-medicate with OTC products. Most OTC drops contain vasoconstrictors that can result in rebound hyperemia once discontinued and can cause toxicity if patients use these products long term. If you choose to not prescribe medication for a patient experiencing allergy symptoms, then you may inadvertently be encouraging the purchase of OTC "get the red out" drops that can do more harm than good.
Two OTC products that you can consider for treating mild ocular allergies short term are Naphcon A (Alcon) and Opcon A (Bausch & Lomb). Both contain an antihistamine (phen-iramine maleate) to help alleviate itching; however, both also contain the vasoconstrictor naphazoline hydrochloride to reduce redness. Because of the potential for OTC allergy drop abuse that results from their short duration of action, I recommend that you use one or more of the options in Table 1 to treat ocular allergies.
The most obvious way to treat any allergy is to remove the allergen. Because this isn't always easy or possible, you should use your arsenal of allergy medications along with artificial tears to help wash away potential culprits.
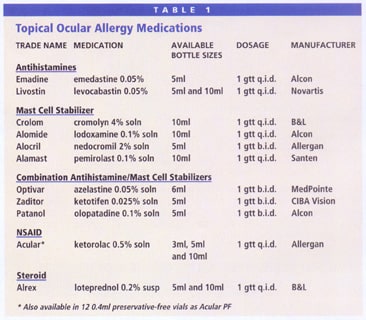
Antihistamines Patients who experience itching from ocular allergies may benefit from antihistamine drops. Emadine (Alcon) and Livostin (Novartis) are both H1 blockers that help alleviate histamine-induced itching. However, antihistamines won't block the synthesis of other inflammatory mediators formed from arachidonic acid, such as prostaglandins and leukotrienes. Thus, these drops aren't as beneficial for patients who have chronic or severe acute allergies. Also, their short duration of action makes other drops more beneficial for chronic sufferers.
Mast Cell Stabilizers By helping stabilize mast cell membranes, these drugs help prevent mast cell degranulation and thus prevent the release of preformed and the formation of new inflammatory mediators. For this reason, drops such as Crolom (B&L), Alomide (Alcon), Alocril (Allergan) and Alamast (Santen) are more useful for prophylaxis.
Because mast cell stabilizers only prevent the release of new inflammatory mediators, they can do nothing for existing symptoms. But for patients who have a known history of SAC, you can prescribe mast cell stabilizers before the onset of allergy season to help prevent the initial onset of the allergic response.
Combination Drugs Fortunately, combination drugs that contain antihistamine and mast cell stabilizing medications are available. Combining the two medications can simultaneously treat the symptoms and help deter future hypersensitivity responses.
The three combination drops currently available are Patanol (Alcon), Zaditor (CIBA Vision) and Optivar (MedPointe). All three offer b.i.d. dosing, so they may allow for continued lens wear in patients who experience mild ocular allergies. However, note that these drops aren't approved for use during lens wear, so advise patients to instill the first drop 15 minutes before contact lens wear and the second drop after they remove their lenses for the day.
A once-a-day formulation of Patanol may soon be available. Clinicians have presented research examining the performance of olopatadine 0.2% (vs. the 0.1% concentration of regular b.i.d. Patanol) at several eyecare meetings. Studies have shown that olopatadine 0.2% when used q.d. effectively prevented allergy symptoms for up to 16 hours after instillation when subjected to an allergen challenge test.
NSAIDs You could also try a nonsteroidal anti-inflammatory drug (NSAID). Acular (Allergan) is the main drug available in this class. It blocks the cyclo-oxygenase pathway, thus preventing inflammatory mediators, such as prostaglandins, from forming. NSAIDs also increase the threshold of nerve endings to help alleviate itching.
If a patient is sensitive to benzalkonium chloride (BAK), the preservative in most ophthalmic drops, then consider preservative-free Acular PF.
Steroids Steroids block the inflammatory pathway further upstream by preventing the formation of arachidonic acid, stopping new inflammatory mediators from forming (Figure 1). Because of potential side effects of long-term steroid use, many practitioners use them only for more severe allergic reactions and only temporarily until the reaction is under control. Alrex (B&L) is the first steroid indicated specifically for allergy treatment. It's a 0.2% formulation of loteprednol, which is also marketed as Lotemax at a 0.5% concentration. Alrex doesn't increase IOP or cause posterior subcapsular cataract formation like more potent steroids do long term.
Allergies and Contact Lens Wear
Contact lens patients who have SAC will present with itchy, watery eyes. You'll often see a papillary conjunctival reaction along with conjunctival hyperemia and chemosis. Patients typically experience a more rapid resolution if they discontinue lens wear; allergens can bind to the surface of hydrogel lenses and cause a more severe allergic response because of the increased allergen concentration on the eye.
For patients who have chronic allergies, more frequent lens replacement and more aggressive cleaning regimens will help prevent allergen buildup on their contact lenses. Instruct such patients to use a daily cleaner or add a daily enzyme such as SupraClens (Alcon) to help improve lens tolerance. Daily disposable hydrogel contact lenses offer the greatest benefit because they minimize lens surface allergen buildup. Combine daily disposable lenses with b.i.d. use of an antihistamine/mast cell stabilizer to help patients who have milder symptoms or chronic allergies to continue wearing lenses.
Differentiating Solution-induced Allergies
Contact lens patients who use chemical disinfection systems may experience a Type IV delayed hypersensitivity reaction resulting from the preservative in their lens solution. For this reason, specify and document the solution that each patient should use and ask patients what solution brand they use at every office visit. Inform patients about why they should stick to one solution rather than buying whatever is cheapest. If a patient experiences a reaction following a recent solution change, then consider switching back to the original solution. If you suspect solution sensitivity and choose to switch the care system, then ensure that the system you recommend contains a different preservative. Remember that many multipurpose solutions contain similar preservatives.
A better option when you suspect solution hypersensitivity may be to switch the patient to a peroxide-based system. Peroxide solutions neutralize into saline, so you avoid the problem of chemical preservatives. Traditional multi-step peroxide-based care systems such as AOSept (CIBA) and Ultracare (AMO) include a separate daily cleaner. A more convenient option is ClearCare (CIBA), a peroxide-based one-bottle cleaner. Make sure patients and your staff understand that lenses cleaned with peroxide-based systems must neutralize for at least six hours before they're safe to apply and that patients should place only neutralized solution in their eyes.
|
|
|
|
Figure 1. Mast cell activation and action of pharmaceuticals 1. Mast Cell Stabilizer, 2. Antihistamine, 3. Steroid,
4. NSAID (modified from Stapleton, 2003). |
|
A final allergy-related lens problem is giant papillary conjunctivitis (GPC), or contact lens papillary conjunctivitis (CLPC). Clinicians suspect that the inflammatory mechanism behind GPC involves both Type I and Type IV responses. Among its potential causes are mechanical irritation and deposited lenses.
Patients who have GPC typically present with ocular itching that becomes worse when they remove the lens. With severe GPC, the lens fit often looks sloppy. Everting the superior eyelid reveals a severe papillary conjunctival reaction over the tarsal plate.
Instruct patients who have GPC to initially discontinue contact lens wear and prescribe a combination drop such as Patanol, Zaditor or Optivar. The steroid Lotemax also has approval for treating GPC. Once the condition resolves, switch patients into the most frequent replacement schedule available to help prevent the buildup of surface deposits. GP lenses are also an option because of their deposit resistance.
Benefitting Patients and Your Practice
Many options exist for treating patients who suffer from ocular allergies. Understanding the etiologies of potential allergic conditions that patients may encounter will help you isolate causative agents and effectively treat their condition. This translates into great benefits for your patients and practice.