contact lens case reports
Trantas Dots
or Solution Sensitivity?
BY PATRICK J. CAROLINE, FAAO, & MARK P. ANDRE, FAAO
|
|
|
|
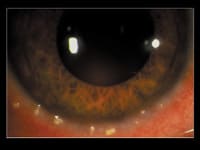
Figure 1. Trantas dots as they appear in vernal
conjunctivitis. |
|
Conjunctival erythema, excessive mucus production, severe itching and cobblestone papillae on the upper tarsal plate characterize vernal conjunctivitis. A limbal form of the condition also exists and manifests itself as discreet lumps of gelatinous excrescences with whitish superficial spots known as Trantas dots (Figure 1). Trantas dots, are often transient and last for only one week. However, Meisler et al (1980) reported bilateral lesions resembling Trantas dots in association with soft contact lens wear, and Frantz et al reported a unilateral case in 1987.
Trantas Dots or Not?
JM is a 28-year-old female with a six-year history of uneventful soft lens daily wear. Her monthly replacement lenses were three weeks old, and she used a multipurpose lens care regimen nightly. For three months, she'd experienced increased ocular irritation, redness and itching in the right eye only. JM denied any history of allergy or atopic disease.
|
|
|
|
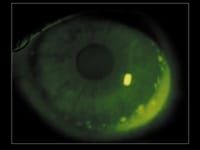
Figure 2. Patient's right eye. Note the Trantas dot-like limbal
lesions. |
Slit lamp examination showed mild inflammation of the right tarsal plate with no giant papillae. The right bulbar conjunctiva was slightly edematous with marked per-limbal injection, but the cornea was clear. We noted numerous raised nodules inferiorly and nasally along the limbus (Figure 2). The left eye was normal. Both lenses were free of deposits and exhibited good centration and movement OU.
We had JM discontinue lens wear for one week and treated her mild discomfort with preservative-free artificial tears p.r.n. At the one week visit, the conjunctival edema and inflammation had significantly improved and the nodules had melted away. We eventually fit her into daily disposable lenses, and she's had no recurrence of the problem.
Determining the Cause
|
|
|
|
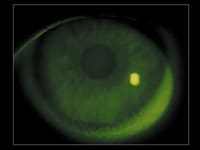
Figure 3. Patient's normal left eye. |
|
Our case was similar to those reported by Meisler and Frantz. We doubt JM had vernal disease because she had no history of allergy or atopic disease. Her age and that she's remained symptom free after six months of daily disposable lens wear appear to rule out underlying vernal disease.
Could the problem have been related to her lens care system? While solution sensitivities are usually bilateral, we've seen cases where sensitivity was unilateral. Therefore, unilateral solution sensitivity remains high on our list of probable causes for these peculiar limbal lesions.
To obtain references, visit www.clspectrum.com/references.asp and click on document #108.
Patrick Caroline is an associate professor of optometry at Pacific University and is an assistant professor of ophthalmology at the Oregon Health Sciences University. Mark André is director of contact lens services at the Oregon Health Sciences University and serves as an assistant professor of optometry at Pacific University.