TOPOGRAPHY & CLS
Mapping A Treatment Plan for Post-Surgical CRT Fittings
Corneal topography is a useful tool in post-surgical contact lens fitting with CRT and follow-up.
By Marjorie Rah, OD, PhD, FAAO
It's well accepted that refractive surgery is a mainstay in the ophthalmic field. Although the ever-changing techniques mean vast improvements in procedures, some patients experience complications such as undercorrection, overcorrection, irregular astigmatism and corneal ectasia following surgery. Although in some cases enhancement surgeries can help, in many cases, gas permeable (GP) contact lenses are the best treatment options. Although reports in the literature provide evidence for the successful use of PMMA, GP, hybrid and hydrogel lenses following refractive surgery, use of GP lenses is widely accepted as the standard of care.
As these cases are often challenging because of the cornea's irregular nature following surgery, corneal topography can serve as a useful tool in contact lens fitting and follow up. The following case report describes the contact lens fitting and topographical changes resulting from overnight contact lens corneal reshaping to enhance the treatment zone following photorefractive keratectomy (PRK).
|
|
|
|
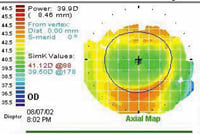
Figure 1. |
|
Case Report
A 31-year-old male artist presented to the clinic for a contact lens fitting. He had a history of photorefractive keratectomy (PRK) in his right eye approximately five years before the visit. He didn't elect to have refractive surgery on his left eye because of the persistent haze and glare he noticed in his right eye.
He was wearing a soft contact lens on the left eye with an average wearing time of approximately 16 hours each day and no lens on the right eye. He came to the clinic hoping for a contact lens treatment that could reduce the visual problems of haze and glare he was experiencing with his right eye.
Distance visual acuity was 20/20 in the right eye with no correction, 20/25 with a soft toric contact lens in the left eye and 20/20 OU. I noted the following manifest refraction: OD: 0.25 sphere with 20/15 acuity and OS: 5.25 2.50 x 180 with 20/15 acuity. Corneal topography revealed a well-centered oval treatment zone in the right eye. The horizontal treatment zone was approximately 5.5mm in diameter; however, the diameter of the treatment zone was only approximately 4 mm in the vertical meridian (Figure 1). The small diameter of the vertical treatment zone was likely the cause of some of the glare and halo problems the patient was experiencing.
Pupils were equal, round and reactive to light with no apparent afferent papillary defect. The lids/lashes, tarsal plates, bulbar and limbal conjunctiva, and iris were all clear of abnormalities in both eyes. I noted grade 1 stromal haze in the central cornea of the right eye. The cornea was clear in the left eye. I noted no fluorescein staining in either eye. The anterior chamber was clear and quiet with wide open angles OU. I also noted no opacities in the crystalline lens OU.
|
|
|
|
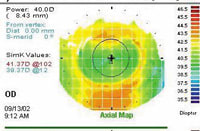
Figure 2. |
|
I discussed various contact lens options, including soft lenses, GPs and corneal refractive therapy with the patient and he expressed an interest in Paragon Corneal Refractive Therapy (CRT) lenses, hoping that the lenses would enhance the treatment zone and decrease the symptoms of glare and halos.
Preoperative corneal topography and refraction data weren't available for the right eye, but the patient believed that prescription was similar to the left eye before surgery. For this reason, I selected the initial diagnostic lens using the corneal topography map and refractive error of the left eye as a guide to determine the appropriate return zone depth (RZD) and landing zone angle (LZA). I selected the initial lens using the slide rule provided with the Paragon CRT fitting set. Using the fitting guide, I selected a diagnostic lens with a RZD = 550 µm and a LZA of -33 degrees.
Although this initial lens was too steep, only two additional trial lenses (changes in return zone depth from 550µm to 500µm in 25µm increments) were necessary to achieve an acceptable fit -- a bull's eye fluorescein pattern similar to that of normal contact lens corneal reshaping.
|
|
|
|
Figure 3. |
|
The patient wore the lens for one month with no significant improvement in vision or changes in the treatment zone diameter. I noted no significant changes in biomicroscopic findings. Figure 2 shows the corneal topography pattern after one month of lens wear. The diameter of the treatment zone is similar to pre-treatment, approximately 4 mm in vertical diameter. Although the lens was well centered on the eye with good movement, the fluorescein pattern evaluation of the lens showed inadequate central touch. I ordered a new lens with a shallower RZD.
After one week wearing the new lens, the patient reported that his vision wasn't as clear as it had been after wearing the previous lens. Unaided visual acuity remained 20/20 in the right eye. Even though he hadn't worn the lens the evening before the follow-up visit, the manifest refraction revealed that the patient was over-corrected at +0.75 0.25 x 005. Again, no changes in slit lamp findings were evident. Fluorescein evaluation of the lens showed an area of central touch approximately 4 mm in diameter with paracentral pooling and adequate edge clearance. The lens was well centered on the eye with good movement. Slit lamp findings remained unchanged from the previous visits.
Evaluation of corneal topography revealed an increase in the diameter of the vertical treatment zone of approximately 1 mm (Figure 3). Because it appeared we achieved the desired effect on the treatment zone diameter, we decided to continue treatment with overnight wear of Paragon's CRT lenses.To compensate for the over-correction of the refractive error, I ordered a new lens with a steeper base curve radius to decrease the magnitude of central corneal flattening by approximately 0.50D.
After wearing the new right contact lens for about three weeks, the patient reported improved vision. He was successfully wearing the lens every other night. The patient reported a reduction in glare and halos with the new contact lens. Unaided visual acuity in the right eye was 20/15. I recorded a manifest refraction of +0.25D with 20/15 visual acuity and noted no changes in slit lamp findings. The corneal topography pattern was similar to the previous visit, revealing a treatment zone that was more round with an enhanced vertical diameter compared to pre-lens wear.
|
|
PARAMETERS OF FINAL LENS: |
|
Paragon CRT BC: 8.6 mm Return zone depth: .475 mm Landing zone angle: -34 degrees Diameter: 10.5 mm Material: HDS-100 |
Because of the success we achieved with the right eye, the patient asked about contact lens corneal reshaping in the left eye. He was advised of the limited success in correcting moderate to high amounts of astigmatism and the potential for success with his refraction.
Conclusion
Although I didn't use a specific corneal topography contact lens fitting software to design the contact lens for this patient, corneal topography was beneficial in determining an initial diagnostic contact lens. In addition, I did find corneal topography essential in monitoring the changes in the contour of the treatment zone.
This case is a good example of how corneal topography can aid the practitioner in post-surgical contact lens fitting and follow up.