prescribing for astigmatism
A Surgical Option for Correcting Irregular
Astigmatism
BY TIMOTHY B. EDRINGTON, OD, MS, FAAO
Additions Technology's Intacs intrastromal corneal rings recently received FDA Humanitarian Use Device Approval for correcting irregular corneal astigmatism. The implants previously had received FDA approval for correcting 1.00D to 3.00D of myopia.
Intacs are an option for keratoconus patients who can't tolerate lens wear and are considering penetrating keratoplasty. A central cornea with no excessive scarring is advised for Intacs surgery, which is an additive procedure that provides increased stability to a weakened cornea in much the same way that rebar strengthens the structure of concrete.
|
|
|
|
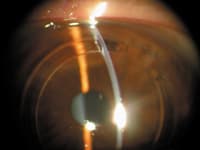
Figure 1. Keratoconus patient post-
Intacs surgery. |
|
Making the Irregular Regular
Intacs help the central cornea to flatten and become more regular in contour with decreased aberrations, enhancing unaided and aided vision. Patients often need spectacles or contact lenses post-surgically to obtain the best vision. If excessive corneal irregularity persists after surgery, then consider fitting GP lenses.
You should find it easier to fit contact lenses after Intacs because the cornea is flatter and more regular in shape. Generally, the corneal surface remains prolate after the surgery. The corneal surface and manifest refraction may take months to stabilize following the surgery.
Performing the Procedure
Intacs are PMMA segments that vary from 0.25mm to 0.45mm in width. The inner optic zone width between segments after surgery is about 6.8mm.
Surgeons may make the channel for segment insertion manually using a dissector or by using a laser (Intralase). Some feel that Intralase may weaken the cornea because it cuts the anterior lamellae. Others prefer Intralase because it creates precise channels.
The surgery takes about 10 minutes under local anesthesia. Surgeons insert two Intacs 150-degree arc segments at a corneal depth of approximately 70 percent (Figure 1). It's preferred if the pre-operative corneal thickness is 450µm or more in the segment area, but you can consider corneas as thin as 300µm. Swanson (2004) recommends inserting the segments on the flattest axis by making the incision on the steepest axis.
Use 1% pilocarpine post-operatively to reduce mydriasis in dark environs and 0.2% brimonidine tartrate ophthalmic solution (Alphagan, Allergan) to stabilize post-surgical intraocular pressure.
Promising Results
Lemp et al (2004) reported that 72 percent of keratoconus patients gained two or more lines of uncorrected visual acuity and 48 percent gained two or more lines of best-corrected visual acuity after Intacs surgery. They also reported a post-Intacs complication rate (including non-infectious lamellar keratitis, vision complaints and neovascularization) of only 4.9 percent.
If surgery is unsuccessful or corneal changes necessitate different segment sizes, surgeons can remove Intacs and if needed, perform penetrating keratoplasty after Intacs' explantation.
A Versatile Option
Intacs may also benefit undercorrected, myopic post-LASIK patients and patients who have pellucid marginal degeneration.
Dr. Edrington is a professor at the Southern California College of Optometry. E-mail him at tedrington@scco.edu.