therapeutic topics
Beyond the Branches: A Closer
Look at Ocular Herpes, Part 1
BY WILLIAM TOWNSEND, OD
Eyecare practitioners easily recognize the distinct branching pattern (dendrites) of epithelial herpes simplex keratitis (HSK), but we may fail to recognize other manifestations of ocular herpes simplex until significant and sometimes irreversible damage to the cornea occurs. We must be able to look "beyond the branches" and recognize non-epithelial manifestations of herpetic eye disease.
Distinguishing the Types
Physicians diagnose about 300,000 or more cases of ocular HSV disease in the United States annually. Serotype 1 causes ocular disease and labial "fever blisters." Patients usually contract it between ages one and five, typically though direct contact with infected tissue or secretions from an adult who has cold sores. Type 2 herpes is usually transmitted by genitourinary contact.
|
|
|
|
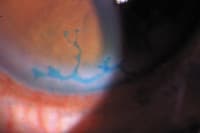
Figure 1. Lissamine green staining
reveals epithelial HSK. |
|
How Ocular HSV Presents
Ocular herpetic disease occurs in several forms, but more than one form may manifest concurrently.
Herpes simplex blepharoconjunctivitis is more common in children, but occasionally occurs in adults. It usually presents as an accumulation of small vesicles or pustules on the lid margin and/or periocular skin. These lesions have an inflamed, erythematous base and the vesicles may ulcerate or harden into crusts after the first week of infection.
Herpes simplex conjunctivitis can present in conjunction with dermal lesions or it may occur as an independent entity. You'll observe pre-auricular adenopathy on the affected side with follicles invariably present.
Epithelial HSK may initially present as discreet areas of punctuate keratitis that coalesce to form the typical dendritic presentation. Margins of epithelial lesions stain with rose bengal and, to a lesser extent, with lissamine green (Figure 1). The base of the ulcer stains with fluorescein. Epithelial cells containing live viral particles swell and rupture, releasing viral particles into surrounding tears and tissue. Virions then enter and infect adjacent cells. It's often self-limiting, but if untreated, may progress to map-shaped or geographic HSK. Differential diagnosis includes Acanthamoeba keratitis, herpes zoster keratitis and corneal abrasion. Acanthamoeba presents with severe pain out of proportion to the clinical picture whereas patients with HSK often report less discomfort than their presentation would suggest. Corneal hypoesthesia is common in HSK, and you can easily verify it with the cotton wisp test.
Treating Ocular HSK
The preferred topical medication is trifluridine 1% (Viroptic, King Pharmaceuticals, Inc.), one drop every two hours up to a maximum of nine drops per day until the ulcer re-epithelializes. After the cornea is intact, prescribe one drop every four hours for a week. Trifluridine is effective and cures most patients within two weeks, but the drug is toxic to human tissue, so taper and discontinue the drops as quickly as possible.
Ophthalmic acyclovir (GlaxoSmithKline) is not available in the United States, but reportedly has slightly greater penetration than trifluridine. Patients who cannot use drops can use oral acyclovir in 200mg, 400mg or 800mg tablets or as a 200mg/5ml elixir. Typical oral dosing is one tablet five times per day.
Dr. Townsend is in private practice in Canyon, Texas, and is an adjunct professor at UHCO. E-mail him at drbill1@cox.net.