CL CARE
Contact Lens Care Products: Problem or Solution?
When patients drop out of contact lens wear, the reason could lie with their care products -- but not always.
By Mark André, FAAO
Our contact lens patients are discontinuing lens wear at an alarming rate. The latest estimates (shared at the last American Academy of Optometry meeting) indicate that 2,700,000 soft contact lens wearers stopped wearing their contact lenses last year -- and half of these did so because of comfort issues. These same patients experienced less lens awareness on the initial fitting than they now experience after wearing their lenses for eight consecutive hours. What happened, and what could we have done to prevent this?
Dryness Drives Away Patients
The most common complaint from our contact lens patients is about dryness. Often times, this symptom leads to a decrease in wearing time and a discontinuation of contact lens wear. I find that the overwhelming majority of these patients have adequate tear volume and that few have a dry eye condition such as keratitis sicca. Relief of their symptoms with artificial tears can prove immediate, but is usually short-lived.
CooperVision recently conducted a focus group with patients in which some claimed that they're afraid to tell their practitioner that they're experiencing comfort problems for fear that their practitioner will take their contact lenses away from them.
Unfortunately, patients have a limited vocabulary for explaining their ocular symptoms to us. Complaints of scratchy, gritty or itchy eyes often lead to the conclusion of dry eye. Are these symptoms related to their tear film, lid condition, allergies, environment, medications -- or has contact lens wear induced them?
The Heart of the Matter
Determining the exact cause of a patient's symptoms and solving the problem requires that you investigate his contact lens-wearing practices.
First, it's important to determine how symptomatic the patient is while he's not wearing his contact lenses. If he experiences no discomfort when he's out of his contact lenses for a couple of days, then it's reasonable to assume that the problem is intolerance to contact lens wear and not dry eye. Lens materials, lens care products and noncompliance with these products may cause these symptoms.
One of the most revealing studies that I've ever taken part in was in conjunction with Casey Vision Correction Center at the Oregon Health and Sciences University. We were conducting an FDA investigation of a new excimer laser for correcting myopia. The protocol required at least a six-month waiting period between the surgeries for each eye. Assuming the operated eye was fully corrected, each patient wore a contact lens on his unoperated myopic eye for at least six months to avoid inducing symptoms from anisometropia. Patient prescriptions fell between 1.00D and 6.00D of myopia with little or no astigmatism. That being the case, we expected to fit the unoperated eye with a spherical soft lens.
During the interview with each patient, a common theme became apparent: Nearly every patient had worn contact lenses in the past and had either discontinued them or desperately wanted to because of discomfort. The most common complaint was dryness during contact lens wear. Several patients were concerned about their ability to wear contact lenses during the six-month study period, but were so anxious to proceed with refractive surgery that they were willing to take the chance. In the final analysis, 97 of the 100 patients could wear contact lenses full time throughout the entire study without any comfort issues. If we could refit 97 percent of these self-proclaimed dropouts into contact lenses that they could wear comfortably all day, then how many other contact lens dropouts could potentially wear lenses again?
|
|
|
|
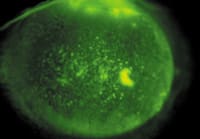
Figure 1. Punctate keratitis from
solution sensitivity. |
|
Identify the Exact Products
Assuming that we fit the contact lens properly, the first adjustment to make in an attempt to improve comfort is to change the care system. This simple change can often return a patient to full-time wear without symptoms. Because we've seen this transformation take place with regularity on hundreds of our patients, we've adopted the motto, "The solutions are guilty until proven innocent."
It's not fair to blame all contact lens-related dryness on the contact lens solutions. Even when a change in care products makes a significant difference in patient comfort, we still need to identify the cause. Many questions remain unanswered and we must develop a plan to avoid a recurrence of this problem for the patient.
When a contact lens wearer presents with a problem, it's important to know exactly what product(s) he's been using. In my experience with my patients, simply asking them this question usually garners the response, "the stuff you gave me." Instead of asking them outright, I now ask them to call or e-mail me when they get home and have the product in their hands so that we're certain of the brand and its contents. I've heard some creative stories about how a mystery solution appeared in a patient's bathroom or contact lens care area. The most disturbing thing about patients' answers is finding out how many unsuspecting individuals are using only saline solution to disinfect their lenses.
Getting the Scoop on Generics
Many of our patients have switched to a contact lens care product other than the one we recommended. If you think that your patients are different, then you're kidding yourself. About 70 percent of contact lens wearers are noncompliant. A study from a number of years ago in the cardiology department at the University of Wisconsin found that patients complied only 50 percent of the time when their lives depended on it.
Patients often base their decision on which contact lens solution to purchase solely on cost. In some cases, this can represent a significant savings of several dollars for a bottle. Today, nearly half of the soft contact lens solutions sold in the United States are generic brands. In the Portland area alone, we identified 19 different brands of generic multi-purpose solution. Although the major solution manufacturers supply most generic brands and the brand name of the generic solution stays the same, the formulation may change from year to year.
The three largest providers of generic contact lens solutions all changed the formula of their private label multi-purpose solutions at least two times in the past five years. According to an industry source, the five largest drug store chains and the three largest grocery store chains all changed the formula of their private label multi-purpose solutions at least two times in the past five years.
The patient doesn't realize what formulation he's purchasing of a generic/store brand unless he takes the time to compare the product ingredients listed in small print. The package graphics typically don't change even when the formulation does. And unless the patient experiences an acute reaction to the "cheaper" brand of solution, the savings are too good to pass up and it's easy to justify future purchases of low-cost solutions.
|
|
|
|
Figure 2. Inflammation of the upper tarsal
plate. |
Looking at Lens-Solution Compatibility
We're just beginning to discover that some contact lens solutions don't work as well as others on certain contact lens materials. A study at the University of Waterloo (Des Fonn et al, 2003) found that 37 percent of patients wearing silicone hydrogel contact lenses on a daily wear basis had significant corneal staining when using solutions preserved with PHMB compared to only two percent of those using Opti-Free Express (Alcon). Vistakon has reported that its new Acuvue Advance contact lens isn't compatible with Solo-care Plus multipurpose disinfecting solution (CIBA Vision).
Unfortunately, we know little about lens-solution compatibility and usually find out by trial and error on our unsuspecting patients. Several clinical trials underway around the world aim at helping us better understand the compatibility of certain lens materials with various solutions. Until this information is available, we must rely on our own clinical skills to determine compatibility between lens materials and care products.
Making a Positive ID
In the past, solution reactions were much easier to identify. When patients reacted to preservatives and/or disinfectants such as thimerosal or chlorhexidine, their eyes were red, light sensitive and discharge was apparent. Slip lamp findings usually revealed limbus-to-limbus superficial punctate keratitis (Figure 1). Symptoms subsided after a few days of lens discontinuation, then we dispensed new contact lenses and a preservative-free contact lens care system, which usually solved the problem.
The more contemporary multi-purpose contact lens care products rarely cause the same type of reaction as older care products. In fact, the only symptoms that most contact lens patients today experience are dryness and possibly mild discharge, which many often mistake for a mild seasonal allergy. Generally, these eyes aren't injected and don't exhibit any corneal slit lamp findings. In every case, you should invert the upper lid to check for inflammation or other papillary changes (Figure 2). Commonly, low-grade inflammation of the upper tarsal plate may be the only visible sign of a problem, and dryness may be the only subjective symptom.
It's sometimes difficult to convince a patient that the same contact lens care system he's used for months or even years is probably to blame. It requires an explanation on how our bodies can have a delayed allergic reaction and become hypersensitive. For example, some people have a delayed hypersensitivity response to bee stings, which can eventually be life threatening. Although solution reactions in no way compare in severity to bee sting allergies, this analogy allows patients to understand the cumulative effects of the solution reaction with long-term use.
Focusing on Patient Care Habits
Although it's easy to blame the lens care products alone for contact lens-induced dry eye, we can't exclude patient care as a possible cause. Most of the major lens care brands today have "no rub" labeling simply because patients prefer the convenience. The majority of our patients weren't rubbing their contact lenses clean before this labeling change, and for many, the no-rub philosophy alleviates any guilt issues they had from improperly caring for their contact lenses.
Passive cleaning of contact lenses is effective if done as instructed. The problem is that few patients use the no-rub products according to the manufacturers' guidelines. In fact, I've yet to find a single patient who follows the instructions, which are the basis for FDA approval of the "no rub" labeling. The directions for the care of a soft contact lens with a no-rub care product generally instructs the patient to thoroughly rinse each side of the contact lens (for five seconds) with the multi-purpose disinfecting solution before storing the contact lens. Most patients interpret "no rub" as: remove contact lenses and store in the lens case without cleaning or rinsing -- and sometimes without even changing the solution in the case.
The accumulation of deposits from improper use of contact lens care products is undoubtedly partly responsible for some of the end-of-the-day discomfort that our patients experience. Also, most patients wear their contact lenses longer than the manufacturers recommend. More than one year ago, CIBA Vision reported that on average, patients replace bi-weekly replacement lenses every 29 days instead of every other week. Collectively, we've done a poor job of educating our patients on the value of maintaining proper contact lens care that will ensure the health of their eyes.
Quality Time with Patients
The amount of time we're able to spend with each of our patients has dramatically decreased over the last two decades. In speaking directly to hundreds of practitioners over the last couple of years, I asked them how much time they spend with a new patient who's interested in contact lenses. I was shocked to find that the average time is between 10 and 15 minutes (not including the eye exam). During this time, the doctor must make several decisions and, in many cases, evaluate contact lenses.
If the patient has astigmatism, does the practitioner recommend a toric soft contact lens or does he use a GP lens to provide correction? Does the patient want daily or extended wear lenses? In the case of a prospective soft lens wearer, how often is he going to dispose of his lenses: daily, bi-weekly, monthly, quarterly or less often?
What about colors? How many times have you chosen the perfect contact lens in your mind, only for the patient to inform you that he wants his brown eyes to be blue? Now we're 10 minutes into the contact lens examination and we haven't even tried on a contact lens yet.
Contact lens care products and patient care often become an afterthought that the practitioner usually delegates to an office assistant or technician. As the time the practitioner spends with the patient decreases, the support staff's value increases. It becomes the responsibility of the staff to educate the patient on the importance of proper care and maintenance and to stress compliance.
Convincing the patient of the importance of proper lens care becomes more challenging, as patients view contact lenses more as commodities and less as a medical devices. The short time that we spend with patients on the initial visit sets the course for their contact lens wear for the rest of their lives. Their long-term success with contact lenses relies on the advice we give them in the early stages of their lens wear. Most of us take better care of an automobile that we won't be driving five years from now than we do with our eyes that need to last us a lifetime. Preparing the patient for continued success -- possibly 40 to 50 years in the future -- requires patient education.
Tips for Success
Because most of the contact lens problems we solve relate to lens care products and compliance, it's important to tell patients how critical it is to maintain their contact lenses properly with care products that will ensure years of safe and comfortable wear. Tell patients to watch for the earliest signs of allergies (redness, itching or discharge in their eyes) and to return to the clinic for evaluation when these symptoms present. Let them know that this isn't a normal part of wearing contact lenses, and that our goal is for them to wear their contact lenses comfortably for all waking hours. Inform them that the low cost generic solutions change formulas periodically and that their ability to wear their lenses may vary with these changes.
The support staff plays an important role in patient education. In most practices, the doctor doesn't have enough time during the fitting to establish safe guidelines for the wear and care of contact lenses. Continuing education for technicians and support staff is necessary to keep everyone in the office updated with changing technologies.
We should make every effort to provide safe and comfortable contact lens wear to patients who desires it and to reduce the number of contact lens dropouts. An integral part of a successful contact lens practice is a universal understanding of the important role of contact lens care products and their proper use.