BANDAGE LENSES
Bandage Lenses: New Opportunities in Practice
Silicone hydrogels allow practitioners to successfully fit more patients who have compromised corneas.
By Gregg Eric Russell, OD, FAAO
Gasset and Kaufman first described the use of hydrogel contact lenses as bandage lenses in 1970. Their concepts were simple. The lenses helped protect fragile epithelium and improved comfort, and the end result was a new treatment modality for patients who had bullous keratopathy.
Since these early uses, practitioners have used bandage lenses to treat patients who have corneal abrasions, recurrent erosions, filamentary keratitis, bullous keratopathy, corneal perforations, wound leakage, entropion, trichiasis and lagopthalmus. They're excellent for modulating pain, and they assist in visual improvement.
HEMA-Based Bandage Limits
Clinicians have tried using bandage lenses to treat exposure keratitis with limited success. The negative effects of HEMA-based lenses on the tear film may offset their positive benefits. Some hydrogel wearers develop corneal desiccation inferiorly, which incomplete blinking and lens water loss may worsen. HEMA-based contact lenses may also have a negative effect on tear break-up time by causing it to shorten. This water loss may contribute to further epithelial damage. Patients who experience this require a low-water lens that they can wear on a continuous basis.
Patients generally have better comfort while wearing thin and soft contact lenses, but the materials don't always mask the impact of irregular astigmatism that's common with corneal surface anamolies. It's also clinically important to control bandage lens movement to minimize the potential shearing forces on the epithelium. When you factor in the importance of oxygen availability (which affects healing), it's easy to understand why you'd want a bandage that has the highest possible Dk/t value.
|
|
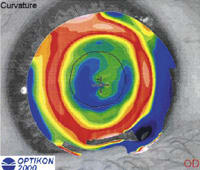
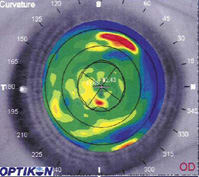
| Figure 1. (left) Topography without lens, Figure 2. (right) Topography over lens. Note the improvement of central symmetry near the central 3.0mm characterized by the visible dark ring near the line of sight. | |
New Lenses, New Opportunities
Silicone hydrogel lenses such as CIBA Vision's Focus Night & Day have made new uses for bandage contact lenses possible. Following are some case reports that show some of these new opportunities.
Healing Abrasions and Post-Surgery Corneas
The literature has described how bandage contact lenses can reduce pain in conjunction with a cycloplegic agent for patients who have severe abrasions and pain. However, healing issues remained as the lenses dried out and became bothersome -- particularly in overnight wear situations. This is most notable for refractive surgery patients -- especially those who may have incurred an abrasion during microkeratome translation or who underwent primary PRK or LASEK.
The breathability and low water content of the Night & Day lens may help promote more rapid healing when patients wear it as a bandage lens. Patients can often tell the difference with the Night & Day lens in place because it may considerably lessen foreign body sensation and light sensitivity.
|
|
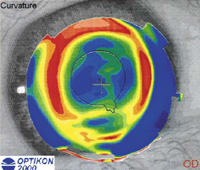
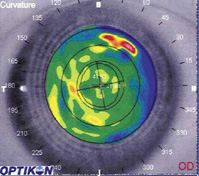
| Figure 3. (left) Topography OD, Figure 4. (right) Topography OD over Focus Night and Day. Note the reduction or increased corneal steepening in the right picture as the contact lens is fit over the apex. In Figure 4, also note the red ring that surrounds the optical zone in the contact lens. | |
Case Report Patient #1 is a 37-year-old male who underwent primary LASEK in his right eye and postoperatively wore an 8.7mm base curve Acuvue (Vistakon) lens with a sphere power of 0.50D. Six days after the original surgery, we noted a small epithelial defect near the patient's line of sight. Corrected vision with the lens was less than 20/40, and the patient still experienced discomfort.
Four weeks after the original surgery, the patient proceeded with LASEK surgery OS. Postoperatively, we fit the patient with an 8.4mm base curve Night & Day lens with a sphere power of 0.50D. Three days after surgery, the patient was completely comfortable and we removed the lens. His uncorrected visual acuity OS was 20/25.
Correcting Irregular Astigmatism
Irregular astigmatism occurs when the axes of the planes of refraction differ by something other than 90 degrees. The presence of irregular astigmatism, particularly when located near the patient's central cornea, is often associated with decreased optical performance. Causes for irregular astigmatism vary, but they can include excessive dry eye, refractive and cataract surgery and injury. Clinicians have suggested a number of ways to resolve this entity, including soft or GP lenses or additional refractive surgery.
Using soft lenses to neutralize irregular astigmatism after LASIK isn't a new idea. Chou et al (2001) showed that a soft lens can reduce the effect of irregular astigmatism and improve vision for such patients after LASIK. However, their study covered one-time testing only and didn't provide any long-term follow up or suggestions for improvement. The increased modulus of Night & Day neutralizes the optical impact of irregular astigmatism in some patients.
Case Report Patient #2 is a 25-year-old female who had undergone primary LASIK for the elimination of 6.50D of myopia. Unfortunately for her, she developed striae that remained untreated until five months after the surgery and ultimately became permanent. As a result of the induced irregular astigmatism, her best corrected visual acuity (BCVA) became fixed at 20/50.
We fit her with an 8.4mm base curve, 0.50D Night & Day lens, and her vision improved immediately to 20/25 with the lens in place. We also noted improvements in her corneal topography with the lens in place as determined by Maloney Indices (Figures 1 and 2). Simply stated, a Maloney topographic irregularity score is a reflection of the smoothness of the corneal surface and tear film. Perfect spheres often have a score of 0.1D. Healthy human corneal surfaces are approximately 0.4D. Surgical procedures such as RK and LASIK increase the score and provide doctors with a quantitative measure. The higher the number, the more irregular the surface.
Case Report Patient #3 is a 47-year-old female who presented for evaluation of blurred vision. Another practitioner had previously diagnosed her with keratoconus in her left eye, but she hadn't been able to wear a lens. She was wearing a pair of 5.50D, 8.3mm base curve Acuvue 2 lenses OU, which gave her BCVA of 20/25 OD and 20/200 OS. Topography confirmed the presence of keratoconus OD (Figure 3) and a significant cone OS.
We fit her with 8.4mm base curve, 6.50D Focus Night & Day lenses OU, which improved vision to 20/20 OD and the quality of the topographic surface (Figure 4). We fit a piggybacked GP lens OS.
Using Silicone Hydrogels for Piggyback Fits
The literature has described the benefits of fitting Night & Day lenses as the base lens in piggyback systems. We've found that you can fit the lens steep, but make sure that minimal, if any, edge lift occurs. With Night & Day, you can use fluorescein to deter-mine the fit of the soft lens and the overlying GP lens -- a tremendous advantage over other lenses in which you need a high molecular weight fluorescein.
Case report Patient #4 is a 52-year-old white male who underwent primary LASIK surgery to eliminate spectacle use. His preoperative myopia was 9.00D OU. Six years after his first surgery, he developed ectasia in his right eye and couldn't comfortably tolerate eyeglasses or GP lenses.
We attempted to fit him in a large diameter GP lens, but had limited success. We also attempted to fit him in a Rose K (Lens Dynamics) cone lens, but the patient still experienced persistent discomfort.
Finally, we fit him in a piggyback design using Night & Day as a base lens. The patient noticed immediate improvement in his ocular comfort and was able to wear the lens without incident for eight hours or more each day.
Relieving Dry Eye and Exposure Problems
For patients who need to continually instill lubricating drops in their eyes, particularly after refractive surgery, the benefits of using a bandage lens can prove dramatic. Thin, high-water lenses tend to draw fluid from the anterior surface of the cornea, but the different properties of the Night & Day lens can help patients who have exposure problems.
We found that silicone hydrogels can benefit patients who have significant lagophthalmus and exposure issues. Low-water lenses are typically the go-to option for fitting patients who exhibit dry eye symptoms. Less explored is the use of silicone hydrogel lenses to treat severe dry eye. Not all patients will benefit from this strategy, but it's an option. Maintain contact with patients on whom you try this option to ensure that they can wear the lenses comfortably and that they can apply and remove them.
|
|
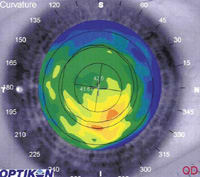
| Figures 5 and 6. Topography OD before epithelial debridement (left) and three weeks later (right). Note the improvement of the central corneal regularity. | |
Managing Basement Membrane Dystrophy
Basement membrane dystrophy development isn't well understood. While many patients don't experience significant problems resulting from an uneven epithelium, it can be particularly bothersome if the disruptions occur within the central 3mm of the cornea (Figures 5 and 6). Degradation in optical images as a result of tear film disruption from the underlying epithelium can result in devastating visual consequences.
Practitioners usually treat such patients with hyperosmotic drops and ointments, or the patient may undergo PTK treatment. Debridement of the area and bandage lens application with a Night & Day lens helps reduce the pain associated with the procedure and may help promote more active healing with improved oxygenation.
|
|
|
|
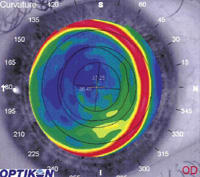
Figure 7. Appearance of lipid on the outer surface of Focus Night & Day lens after four days of extended
wear. |
Watch for Deposits
Silicone contact lenses have shown great promise as a material dating back to the early 80s, principally because of their exceptionally high Dk/t value. Unfortunately, the pure silicone lenses at that time were hydrophobic, absorbed lipids quickly and were also known to tighten up with wear time.
The silicone hydrogel lenses now available use surface and internal treatments that make the lenses hydrophilic. These treatments help to reduce protein deposition on the lenses.
While Night & Day has proven to be relatively free of protein adherence, some deposition may occur when it's worn in a healing eye. Figure 7 shows such deposition in a patient who wore the lenses overnight for a period of four days. We prescribed the lens to protect the cornea after the patient developed significant corneal dryness following LASEK. I've found that patients who have severe dry eye have additional proteins and debris in their tear films that might explain such surface deposition.
If the Lens Fits...
Night & Day offers technological improvements that allow us to incorporate more sophisticated treatments for clinically challenging patients. But it's certainly prudent for clinicians to view each case on its own merits and proceed accordingly. In some cases, particularly for patients who have significant corneal abrasions, practitioners should consider concurrent use of antibiotics as well as cycloplegia.
Keeping in mind the new opportunities in patient care that silicone hydrogels provide, practitioners now have even greater chances for improving vision and general comfort for patients who require a bandage contact lens.
The author has no proprietary interest in any of the products mentioned in this article.
To obtain references for this article, please visit http://www.clspectrum.com/references.asp and click on document #106.





