contact lens case reports
Correcting Human Error
BY PATRICK J. CAROLINE, FAAO, & MARK P. ANDRÉ, FAAO
When prescribing any form of vision correction, mathematical errors can occur. In the case of eyeglasses, we can easily correct our errors by a simple remake of the prescription. Contact lens prescribing errors can result in optical or physical discomfort for patients, but we can easily remedy this by removing the offending lenses.
In the case of refractive surgery, the ramifications of mathematical errors may be more devastating and difficult to surgically reverse.
A Typo's Ramifications
A 46-year-old male underwent LASIK in June 2001. His preoperative refractive error was OD 5.75 4.00 x 005 and OS 6.00 3.75 x 010. The surgery was uneventful, but the patient quickly noted that the vision in his left eye was significantly worse than that in his right.
At follow up, the patient's objective findings were within normal limits, but his uncorrected visual acuities were OD 20/25 and OS 20/400. A manifest refraction measured OD 0.25 0.50 x 015 20/20 and OS +2.75 5.50 x 007 20/30.
|
|
|
|
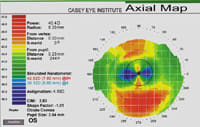
Figure 1. Postoperative map of the patient's left eye. Note the high with-the-rule astigmatism present over the
pupil. |
|
The left eye refraction revealed that the patient's corneal cylinder had significantly increased along the 180 degree meridian. We suspected that someone had entered an axis of 100 degrees into the laser rather than the appropriate axis of 10 degrees. Corneal mapping OS showed simulated Ks of 38.12 @ 004/42.62 @ 94 (Figure 1).
We performed confocal microscopy OS, revealing a total corneal thickness of 495µm. The flap thickness was 116µm, leaving a residual stromal bed of 379µm. The confocal measurement indicated that enough stromal tissue remained to permit a corrective LASIK procedure, but additional surgery would probably leave the patient hyperopic and approach the 250µm residual bed limit for the remaining cornea.
|
|
|
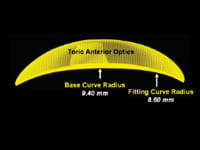
| Figure 2. Diagram of the custom reverse geometry toric soft lens. | Figure 3. The custom soft lens on the patient's left eye. |
Correcting the Mistake
For many reasons, the patient elected to forgo additional surgery and pursue a more conservative contact lens option. We fit him with a custom reverse geometry toric soft lens with a 9.4mm central base curve, an 8.6mm fitting curve, +1.25 5.50 x 10 power and 14.8mm diameter (Figures 2 and 3). His visual acuity with the lens was stable at 20/30.
Our patient has worn the custom soft lens for more than one year and recently returned for routine follow up. He remains content with the comfort and vision that his lens provides, and we hope he'll continue to do well until a more viable option becomes available.
Patrick Caroline is an associate professor of optometry at Pacific University and is an assistant professor of ophthalmology at the Oregon Health Sciences University.
Mark André is director of contact lens services at the Oregon Health Sciences University and serves as an adjunct assistant professor of optometry at Pacific University.