contact lens case reports
Complex History Means No Easy Answers
BY PATRICK J. CAROLINE, FAAO, & MARK P. ANDRÉ, FAAO
|
|
|
|
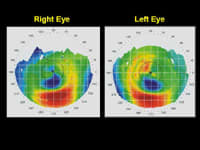
Figure 1. Corneal mapping before GP lens fitting. |
|
|
|
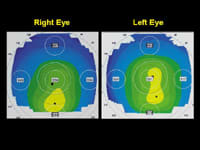
| Figure 2. Orbscan pachymetry maps. | |
|
|
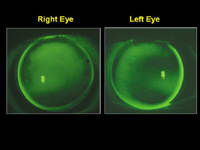
| Figure 3. GP fluorescein patterns. |
JW is a 38-year-old male physician who was referred to our practice for a contact lens fitting. He has a complex ocular history of having undergone daily atropine therapy for myopia correction from ages 9 to 15. JW reported no refractive surgery history, however, he'd worn toric soft contact lenses intermittently from ages 24 to 36. He hasn't worn contact lenses for two years, electing to wear glasses only.
An Unknown Cause
Today, JW presents with peculiar corneal topographies exhibiting symmetrical paracentral zones of corneal flattening adjacent to zones of inferior steepening. His corneas are clear, free of corneal pathology, making the paracentral flattening a condition of unknown etiology.
Manifest right-eye refraction was +1.00 2.50 x 104 20/20; left eye +0.75 2.50 x 70 20/20. Despite his excellent end point acuities, JW reports significant symptoms of daytime ghosting and nighttime halos.
Corneal pachymetry with the Orbscan revealed right eye central corneal thickness of 559µm and 1.5mm inferior, 545µm. Left eye central corneal thickness was 551µm and 1.5mm inferior, 548µm.
We eventually fit JW with GP lenses with these specifications: right eye: 44.00 (7.65mm) 2.50D. 9.0mm, left eye: 43.75 (7.70mm) 1.50D. 9.0mm. Fluorescein patterns showed mild apical clearance OD, alignment OS with slight "touch" across the areas of inferior corneal steepening. In a week, he achieved a full-time wearing schedule with visual acuities of 20/20 OU. He reported significant improvement in subjective symptoms of ghosting and halos.
Time Will Tell
JW demonstrates a case of bilateral paracentral corneal flattening/thinning. Keratoconus or pellucid marginal degeneration may be the underlying cause. However, JW's topographical maps would represent extremely atypical forms of either condition. Might the peculiar corneal changes be related to JW's long-term use of topical atropine, or an atypical form of corneal warpage secondary to 12 years of toric soft contact lenses?
At this point, we classify JW's diagnosis as FLC (Funny Looking Corneas) of unknown etiology. Perhaps time will add more clarity to the true diagnosis.
Patrick Caroline is an associate professor of optometry at Pacific University and is an assistant professor of ophthalmology at the Oregon Health Sciences University. Mark André is director of contact lens services at the Oregon Health Sciences University and serves as an assistant professor of optometry at Pacific University.