the contact lens exam
What the Ocular Surface
Can Tell You if You Listen
BY RENEE REEDER, OD
Evaluating the ocular surface is critical for predicting contact lens success. Placing a contact lens on the eye may disrupt the anterior lipid layer of the tear film. Screening for potential and present problems will help better manage contact lens patients.
With white light, look for inflammation, tear debris and birefringence, and signs of punctate epithelial staining. Look at lid margins for inflammation, lash loss, and signs of meibomian gland dysfunction and blepharitis.
|
|
|
|
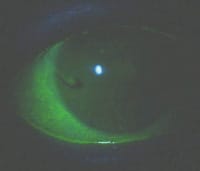
Figure 1: Lissamine of the conjunctiva and cornea. |
|
Helpful Dyes
Next, instill lissamine green and sodium fluorescein. Recent studies show lissamine green stains as well as Rose bengal with less stinging, and that instilling lissamine and fluorescein simultaneously doesn't influence results. Upon instillation, wait 10 to 15 seconds, then look with white light for corneal and conjunctival staining with lissamine. Next, switch to blue light and assess tear break up. Because placing a lens on the eye reduces tear break-up time (TBUT), we need to know our starting point.
After assessing TBUT, find a wratten filter. If you don't have one, use a No. 8 yellow camera filter. It's a slightly different wavelength, but an acceptable substitute. Continuing to evaluate the conjunctiva with cobalt blue light and a filter, you may appreciate subtle staining of the conjunctiva and limbus not previously seen. Check the cornea in all 5 zones, documenting extent and depth of staining in each area.
|
|
|
|
Figure 2: Tear film, cornea, and conjunctiva stain using fluorescein and wratten filter. |
What's Up with the Lids
Next flip the lids. In this age of allergy, asthma and pollution, baseline examination is critical and palpebral conjunctival changes can serve as a predictor of success. With fluorescein and your filter, look for papillae and note size and location. With white light also note redness, petechial hemorrhage and scarring or fibrosis. Patients who have significant allergic response have poorer tear quality because of inflammatory mediators as well as irregularities to their mucin layer. Addressing these underlying problems and choosing a daily disposable lens may improve your patient's chance of success.
Finally, look at the lid margins. Digital expression of the meibomian glands can tell you much about the patient's tear quality. Look for turbidity, viscosity and ease to which they're expressed. Thick, hazy expressions promote inflammatory factors. These patients may have a lower tear pH than patients who have open glands, which may affect how care products work for them. Start warm compresses for healthier tears and a more successful lens fit.
Putting it Into Practice
Thorough evaluation helps you choose the right lens and solution. Managing underlying conditions enhances patient and practice success.
Dr. Reeder is an Associate Professor and Chief of the Cornea Center for Clinical Excellence at the Illinois College of Optometry.