FUTURE OF CONTACT LENSES
2004: What's Next in Contact Lenses?
The future is a promising place -- especially for contact lenses. Just check out this overview.
By Brien A. Holden, PhD, DSc, OAM and Kylie Evans, BA
The revolutions in contact lens development and practice in the last 60 or so years have included hard lenses, hydrogels, rigid gas permeable (GP) lenses, daily disposables and now silicone hydrogels. Each development has advanced the quality and convenience of the vision correction we provide to wearers. So how far are we on the way to the ideal lens? Where are we now with the various technologies, and where are we going?
Daily Disposables: the Strategy, the Reality
When daily disposable contact lenses first appeared, they were marketed by manufacturers as a safe, convenient alternative to the lens and case cleaning regimen. "Wear for a day and throw away" attracts many patients and captures major market share, especially in Europe and Japan. But while the daily convenience is there, problems remain.
The daily disposable strategy was that regular lens replacement would eradicate causes of infection (lens handling, deposit build-up and contaminants). However, unauthorized overnight wear with materials not designed for extended wear (EW) and multiple use with inadequate disinfection make the opposite true. One study (Radford 1998) shows that the infection risk with disposable soft contact lenses is 3.5 times greater during daily wear and 4.8 times greater during EW compared to equivalent nondisposable lens wear. Specific risk factors include occasional overnight use, which according to a Bausch & Lomb Survey occurs in 10 percent of wearers, irregular disinfection and the use of chlorine-release systems with poor case hygiene.
Daily disposable lenses represent an incredible manufacturing advance, but we believe two improvements could make them even better:
1. Better materials to improve end-of-day comfort.
2. Higher oxygen transmissibility (Dk) to avoid the hypoxic risks of overnight use.
|
|
|
|
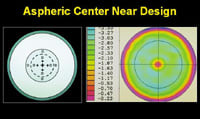
Figure 1. An aspheric center near design. (Courtesy of Pat
Caroline) |
|
Silicone Hydrogels: Gaining Worldwide Acceptance
Silicone hydrogels are breakthrough products that deliver ocular health advances, patient convenience and market growth. Silicone hydrogel use has doubled in the past year, and more than one million high-Dk wearers exist around the world.
Practitioners are seeing high levels of patient satisfaction and good corneal health with these lenses. The convenience of EW is one of the key drivers behind the growth in silicone hydrogel wear, and myopic patients comprise the main market segment.
However, practitioners recognizing silicone hydrogels' value for a wider range of patients is what fuels the most recent market growth and market expansion. Many practitioners are now choosing high-Dk silicone hydrogel lenses first -- regardless of prescription and wear schedule -- because these lenses offer the potential for superior metabolic health. Practitioners increasingly use silicone hydrogels for all modes of wear, from continuous to daily. The lenses also often provide better comfort than conventional daily lenses and can prove beneficial for dry eye patients.
Silicone hydrogels also have found a place as a therapeutic lens for a range of conditions. Again, the ocular health benefits of high Dk combined with the comfort of a soft lens make silicone hydrogels an excellent choice as a bandage lens.
Some Problems Solved, Some Linger
Some practitioners remain wary about the safety of EW. However, various worldwide studies on silicone hydrogel performance demonstrate that the lenses have solved the problem of hypoxia with EW (Keay et al, 2000; Covey et al, 2001; Brennan et al, 2002). These results and positive experiences of colleagues are convincing practitioners that silicone hydrogels are a valuable option for all contact lens patients.
Clinicians believe that a healthy epithelium will maintain a strong barrier to infection and should reduce the incidence of microbial keratitis (MK) with EW lenses. Unfortunately, we continue to see cases of MK with EW of silicone hydrogels.
Anecdotal reports indicate that poor compliance and inadequate lens hygiene remain major risk factors for infection. In 24 of the cases in which we have details of a patient's wear schedule, 10 were noncompliant with their wear schedule; practitioners fit three of these patients with lenses despite existing lid margin disease or dry eye, and one continued lens wear against medical advice. In addition, where patients reported hygiene practices, one stored lenses in tap water, one rinsed lenses in tap water, one stored lenses in unit-dose saline, one rinsed in homemade saline and one reapplied lenses without disinfection.
For EW with both conventional and disposable low-Dk soft contact lenses, researchers found an annualized MK incidence of one in 500 patient-years in the retrospective studies of both Poggio et al (1989) and Cheng et al (1999). We still don't know the rate of MK in silicone hydrogels. In our own prospective studies in Sydney, we've had one MK in 724 patient-years with 30-night continuous wear, which is 3.4 times less than our one in 210 MK rate with six-night low-Dk EW. These numbers are too small for an accurate or statistically valid idea of the real annualized incidence, but we hope current studies in Australia, New Zealand, the United Kingdom and the United States will provide more information on the absolute rate and the risk factors associated with MK and silicone hydrogels.
Researchers continue to work on the next generation of silicone hydrogels. Key areas include optimizing lens designs and surfaces to improve comfort and to reduce mechanical adverse events to an absolute minimum, and anti-bacterial surfaces or materials to try to eliminate microbial-driven adverse events and MK. It's critical that the industry maintain its investment in these areas, as the resulting innovations will undoubtedly take contact lenses to the next level.
Ortho-k: Interesting Possibilities
Orthokeratology hasn't yet reached its potential. The following few areas need work:
- Practitioners need to understand its limitations and manage the rare but important risks.
- Practitioners need to more widely use the designs and materials that we have to gain the next level of experience.
- New designs and materials, which can make an immense difference.
Ortho-k uses the same optical principle to restore eyesight as laser surgery -- central corneal flattening -- but it's reversible and noninvasive through the programmed use of specially designed, GP, contact lenses. First used in the early 1960s, practitioners have refined the technique over the years, resulting in faster and more predictable outcomes. It's now possible to achieve myopia reduction in days, especially with corneas that are flatter in the periphery. At present the procedure can 'reduce' up to 4.00D of myopia and 1.00D of astigmatism.
However, practitioners can't guarantee success. It doesn't work as effectively on very steep, very flat or very low asphericity corneas. Also, unknown factors exist that may affect outcomes. These vary with each patient and include the rigidity of the cornea and the degree of interaction of the eyelid.
The other concern with ortho-k is ocular health, because the procedure may entail overnight wear of contact lenses. Overnight ortho-k is the clinical protocol of choice in Australia, the United Kingdom and Asia. Overnight ortho-k means that patients are free of glasses or contact lenses for most of their waking hours (Jackson 2001) and don't normally have to use open-eye GP lens wear.
Unfortunately, a relatively high number of MK reports have surfaced with the normally safe high-Dk GP lenses when used for overnight ortho-k. Most of originate from Asia and disturbingly involve children under 12 (for example, two cases of Pseudomonas keratitis in two 11-year-old girls from Taiwan [Lau et al 2003]). Even "best practice" practitioners have reported MK with high-Dk GP overnight ortho-k (Mountford, personal communication).
The two main risk factors for MK are overnight wear and the quality of lens storage hygiene. Given the outstanding safety of high-Dk GP lenses for both daily and EW as demonstrated by the studies of Cornish, Sulaiman (unpublished) and others at the Cornea and Contact Lens Research Unit over the years, it's hard to escape the conclusion that the culprit in MK with ortho-k overnight wear is contaminated storage during the day. The MK reports emphasize the overwhelming importance -- with any type of lens wear -- of safe lens cleaning and storage.
Work by Caroline and colleagues at Pacific University and Tahhan and colleagues at the Institute for Eye Research in Sydney show early promise for the possible use of silicone hydrogels for ortho-k, which brings a new level of excitement to this field.
|
|
|
|
Figure 2. A trifocal contact lens design. (Courtesy of Pat
Caroline) |
Succeeding with Torics
Significant astigmatism affects 30 percent of the world population. Contact lenses for correcting astigmatism have been available for many years, but practitioners often regard them as troublesome to fit and variable in performance. Their biggest problem is balancing stable lens orientation and comfort.
However, a new generation of disposable toric lenses has made an immense difference in the performance of contact lenses to correct astigmatism. These lenses aim to provide both consistent high quality vision and comfort. Leading this race are the Biomedics Toric (Ocular Sciences, Inc.), Preference Toric (CooperVision) and Soflens 66 toric (Bausch & Lomb). We should note that the Institute for Eye Research in Sydney has a commercial interest in the Biomedics Toric, having designed and worked with OSI to bring this product to market.
The exciting news is that this generation of disposable torics aims to make correcting astigmatism using contact lenses as automatic as it is with spectacles. Judging from practitioner acceptance, this is starting to happen. High-Dk materials would clearly provide a huge physiological advantage for these modern designs.
Bifocals: Not there yet
The number of presbyopes worldwide is rising at a staggering rate and is expected to reach 2.3 billion by the year 2020. A survey by Edmunds and Reindel (2003) showed 91 percent of current contact lens wearers aged 35 to 55 years are committed to continuing with contact lens wear. However, among the U.S. population age 55 or older who require vision correction, only five percent wears contact lenses.
One reason for this decline in contact lens use with age may be the lack of satisfactory bifocal or multifocal products. Current contact lens options for correcting presbyopia include:
Simultaneous vision designs. The lenses correct each eye for distance and near simultaneously. The brain perceives two images at once from each eye; therefore, to see clearly, the presbyope learns to automatically process the image that's in focus for the particular viewing distance. Patients wearing simultaneous vision design contact lenses often complain of haloes, ghosting and night vision difficulty.
Alternating vision designs. These use two distinct zones similar to "bifocal" spectacle lenses. One zone is devoted to the distance prescription and one to the near. Contact lenses must move upward on the eye during downgaze while viewing close distances so that the correction zone over the eye changes from the distance prescription to the near. Patients wearing alternating vision design contact lenses often complain of discomfort, as the majority of translating contact lenses are GPs.
Researchers are working on new designs, but we haven't seen anything yet that provides both superb vision and comfort. In addition, new designs may need to recognize our changing vision needs. Some bifocal lenses provide near vision during downgaze for reading or other such "downward-looking" tasks. However, many people use their near vision most while looking at a computer screen. The ideal design should provide clear vision for any eye position and for distance -- but this is proving a difficult task.
However, a good case exists for really testing the full potential of translating soft bifocals to provide good, comfortable binocular vision for presbyopes. As with the contrast in performance among new and old generations of toric lenses, we believe that translating soft bifocal lenses haven't received enough attention from the industry.
Monovision: The Best Option?
Monovision always amazes the layperson. The concept of lenses correcting one eye for the distance prescription and the other eye for near -- and the brain's visual system automatically selecting the in-focus image to provide relatively normal continuous vision -- is intriguing. It compromises depth perception somewhat, but wearers usually adapt and learn to use alternate visual cues when judging distances.
Monovision is the most successful correction option for presbyopes to date, with a fitting success rate of 60 percent to 80 percent, depending on the type of study. Monovision was the preferred mode of correction compared to bifocal contact lenses for subjects participating in a one-year clinical trial by du Toit et al (2002), and practitioners also selected it as their first preference for fitting presbyopic corrections (Edmunds and Reindel 2003).
Silicone hydrogels may help boost the monovision market by providing patients with the convenience and comfort they want. The convenience of EW is particularly useful for patients who have difficulty seeing to apply and remove their lenses and who may find daily handling of contact lenses problematic.
High-Dk silicone hydrogels also may offer ocular health benefits for older lens wearers. In particular, silicone hydrogels minimize the risk of neovascularization and corneal edema associated with conventional hydrogel contact lens wear that results from the corneal endothelial pump losing its efficiency with age.
Solutions and Solutions
As you can surmise from what you've read, providing contact lenses that are suitable for all ages and all prescriptions requires new developments from fundamental material changes for improved biocompatibility and comfort to surfaces that avoid microbial contamination.
We also need new lens care solutions. Solutions form an essential adjunct to lens wear, and we need to offer our patients solutions that maximize the performance of all lens types and that provide better and more convenient lens hygiene and care. A key area is conditioning and in-eye drops for silicone hydrogels worn on a continuous wear basis.
The Bottom Line
The most important factor for contact lens success is still the practitioner. A number of components contribute to this role:
The skill and confidence with which the practitioner chooses and fits lenses. Matching the patient's needs with the optimum lens correction is an art and a skill. Ideally, practitioners should choose lenses for the excellence of their performance, not for the marketing skill and efficiency of the companies that supply them. In reality, it's the combination of these factors that determines a practitioner's choice. Practitioners should always choose the "best" lenses -- those that maximize long-term patient satisfaction and optimize vision, comfort, ocular health and, lastly, practitioner income.
The support and management that he provides to contact lens patients. These days, the practitioner who creates a bond with his patients based on care, concern, efficiency and personal service prospers. Follow-up visits, particularly with continuous wear, are important not only to ensure ocular health, but also to build patient loyalty. Providing after-hours contact for patients is also important to ensure prompt assistance in the event of an adverse response.
The education he provides to patients. Patient education helps build a relationship and encourages safe and happy lens wear. Compliance to hygiene and wearing instructions is essential for all modes of lens wear. Practitioners should take time to teach new lens wearers the key concepts of lens and eye care, and reiterate this information at every visit. Patients should understand:
- Basic management: Appropriate lens wear times and appropriate lens and case cleaning regimes.
- Monitoring: Every day patients should check whether their eyes look good, feel good and see well.
- Minimizing risks: Such as wearing goggles when swimming, cleaning or replacing lenses after exposure to contaminants and not sleeping in lenses when they're sick.
- Handling Problems: Patients should remove their lenses as soon as they detect a problem and contact the practitioner immediately.
Take a Proactive Approach
The good news is that taking a proactive approach to fitting contact lenses can significantly increase practice revenue, as Hanks pointed out 20 years ago. A recent pilot project study conducted by the Vision Cooperative Research Centre (Vision CRC) and the Institute for Eye Research (IER) and funded by the Contact Lens Industry Council of Australia provided training and support to 20 optometric practices in the Sydney area in an effort to increase their contact lens activities and their profitability.
The average contact lens business growth resulting from the program was 21 percent during the course of the 12 months of the study. Six practices achieved more than 40 percent growth and one achieved 68 percent growth.
The European Federation of National Associations of Contact Lens Manufacturers (EUROMCONTACT) Initiative 2001 found that contact lenses are on average 44 percent more profitable than spectacles. At the local level, an Australian optical industry reference guide, "Eyetalk," estimated in its 1999 survey that the average spending per patient per year on spectacles is $69, while the annual spending per year on contact lenses is $223. During the 1980s, Tony Hanks compared 50 contact lens patients and 50 spectacles patients over two years. He found that contact lens patients brought in 2.2 times more fees, three times more new patient referrals and had four times less attrition.
Many practitioners continue to see contact lenses as an alternative to spectacles rather than dispensing both to their patients both. The Association of Contact Lens Manufacturers (ACLM) in the UK 2000 Survey also showed that 19 percent of practitioners discussed contact lenses only if the patient asked about them, and 74 percent discussed contact lenses only with patients whom they considered suitable.
The Vision CRC/IER program encouraged practitioners to see more of their patients as potential contact lenses wearers and also to seek opportunities for patients who may want to wear lenses only occasionally for specific purposes (for sport or for cosmetic reasons or social events). The program taught staff how to effectively manage the contact lens business. The aim of the Vision CRC/IER program was to bring about maximum results with minimum practitioner efforts. In fact, one advantage to increasing contact lens business is that practices can make the same or even increase income in shorter hours.
Successful practices were proactive and multi-tasking -- they offered patients a range of vision options and used staff effectively to enhance their productivity. The key factor was the practice's willingness to change -- to try new approaches and techniques and to see how they worked.
Looking into the Future
To really compete with spectacles, patients need to find contact lenses simpler, convenient and comfortable. Patients are looking for safe, long-term elimination of the need for vision correction. Many turn to refractive surgery for a permanent answer to their vision correction needs, but the number willing to try refractive surgery is flattening or decreasing each year. Surveys consistently show that a large majority of contact lens wearers would prefer continuous wear contact lenses over refractive surgery as long as the lenses are safe, effective and comfortable.
The future promises to yield an enormous increase in the global contact lens market through three main influences:
1. Product innovation.
2. The number of people who have myopia and presbyopia (rising to an estimated 5.3 billion by 2020, which will represent more than 60 percent of the world's population at that time).
3. The demand from emerging markets such as China and India. The potential contact lens market in these two countries alone will include at least 800 million myopes and 500 million presbyopes.
The quality, scope and cost of the contact lens products that we develop now will govern the number of contact lens wearers we see in 2020.

Ms. Evans is communications manager at the Vision Cooperative Research Centre, Sydney, Australia.