CL TECHNOLOGY
Wavefront Technology and Contact Lenses
As wavefront technology advances, the debate on its potential for contact lenses gets under way.
By Jerome Legerton, OD, MS, MBA, FAAO
The speculation and debate is under way with regard to wavefront- guided contact lenses and the potential to provide visual acuity with contact lenses that meets or exceeds visual acuity provided by conventional best-spectacle correction.
Keep in mind that no controlled study has ever demonstrated that contact lenses provide better visual acuity than spectacle lenses. This may be because of the average amount of residual astigmatism with spherical rigid lenses (Javal's Rule) and the optics and limitations of spherical and toric correction in soft lenses.
But, with breakthroughs in technology is a new mega trend and opportunity on the horizon for wavefront-guided contact lenses and vision optimization? Ophthonix, Inc. of San Diego, recently launched the first of a number of low-cost aberrometers that will enable the modality. The new technology seems to resolve the heretofore limiting problems of calibration, alignment sensitivity and measurement variability. These instruments will allow for the measure of the total aberrations of the eye or of a diagnostic contact lens-eye system. Aberrometers are essential. It's impossible to correct the total eye aberrations using corneal topography estimated higher-order aberration (HOA).
Thibos and others have reported on the repeatability of aberrometers, the variation of HOA over time and the prevalence of HOA in various age groups and changes of the aberration structure of the human eye over time. As early as 10 years ago, Holden (1994) and Cox (1990) calculated induced aberrations in contact lenses as a function of base curve and power. Their data supported the importance of concern for the aberrations of the lens-eye system as opposed to the eye itself. Their work rendered obvious the ideal system for optimization: The measure of residual aberrations with precision diagnostic lenses in place.
|
|
|
|
PHOTO COURTESY OF
OPHTHONIX. |
|
A Precision Process
Legerton and co-workers (2003) have explicated the importance of measuring diagnostic lenses to know the "fingerprint" of the individual diagnostic lens. Given that every manufacturing process has variability in output, a diagnostic contact lens must be one for which the aberration structure is known for the individual lens.
The confluence of aberrometry with no-polish, vibration free, rotationally asymmetric lathe manufacturing is ushering in the potential to correct HOA. What is the basic requirement for HOA correcting contact lenses? (Consider that researchers have established that a clinically significant amount of HOA is of the order of 0.10µm or more over a 6mm diameter entrance pupil.)
1. Correction of all low-order aberrations
2. Optics manufactured to a precision of 0.05µm over 6mm
3. Freedom from environmentally induced dimensional instability
4. Freedom from on-eye flexure
5. Translational movement of less than 0.3mm
6. Rotational stability of +5°
7. Stable pre-lens tear film
8. Optics registered over the entrance pupil
Low-order aberrations dominate and contribute most to retinal defocus. The first step to vision optimization is to correct all low-order aberration. There is little value in correcting 0.20µm of coma if you're ignoring 0.50D of cylinder. Expect to see the leaders in this modality focus on correcting all low-order aberrations as a first step in vision optimization and bringing contact lenses to the full level of visual performance of spectacle lenses.
It's impossible for manufacturing systems that rely on polishing lenses or polishing pins for molds to demonstrate the precision required for correcting HOA. Further, it's improbable that the process limitations of soft lenses will allow a standard deviation of the process to be low enough to meet the level of clinical significance for correcting HOA.
The process limitations are the combination of (not limited to), pin manufacturing, pin-to-mold variation, mold-to-lens variation, polymerization variance and the variance in dry-to-wet radial and linear expansion. Young reported (2002) that the process variation in industry standard hydrogel toric lenses could be improved for frequent replacement toric lenses.
Add to this the dimensional changes of hydrogel lenses from change of hydration during wear, and the concern for success becomes even greater. Young also reported on the variation of on-eye lens positioning of industry standard hydrogel toric lenses. The rotational and translational predictability and stability would have to be improved for hydrogel lenses to become the standard for correcting HOA.
These factors point to the probable leadership of precision manufactured rigid materials for HOA correction. A hybrid lens platform is suggested with a soft skirt that provides the rotational and translational stability while supporting a precision manufactured rigid optical portion.
The subtle features for correcting HOA are sabotaged by wide variances in the pre-lens tear film. If the normal 4µm to 10µm pre-lens tear film gradually and irregularly thins between the blink, new and random aberrations would be induced. The optimum HOA correcting contact lens will need to be accompanied by strategies to facilitate uniform tear thickness. These include plasma or other surface treatments.
Finally, the optics must be registered over the entrance pupil. A registration system that will measure the translational and rotational deviation of the geometric center of the lens from that of the entrance pupil is needed. It's ideal if this measure is simultaneous to the aberrometry measure.
The second step is to decenter and rotate the HOA correction in the lens relative to the geometric center and the base of the lens, so the subtle features register with the entrance pupil when the lens is on eye. Such systems are developed and in use with an aberrometer. Further, computer numerical controlled lathes are in use with novel software that allows for the decentration of the optics as directed by the registration error measurement.
|
|
|
|
Figure 2. Light architecture engineering. (Photo courtesy of Paragon Vision
Sciences) |
Contact Lenses vs. Refractive Surgery
Refractive surgery leads the charge in the value of measuring HOA and incorporating measurements in the surgical plan. Even so, Applegate and Wilson (2003), along with many others, have warned that the biomechanical aspects of healing may wipe out the subtle features of the aberration correction. There is process variation in the creation of a flap alone, whether by microkeratome or by Intralase. The change in the aberration structure of the eye from these procedures in the absence of photo-decomposition confounds predictability. The good news is reports of a higher frequency of 20/20 or better for eyes post wavefront-guided refractive surgery.
Even with the improved surgical outcomes, many forecast that contact lenses can produce optimized visual acuity that will surpass refractive surgery. The ability to combine HOA correction with chromatic aberration reduction through the control of the bandwidth of the lens gives contact lenses an advantage. Technology is forecast to refine the process variations in contact lens manufacturing and fitting. Parallel refinement in refractive surgery may prove challenging with regard to the biomechanical variations in flap creation and healing.
Add to this that the aberration structure of the eye changes with age, so practitioners must regard a one-time surgical intervention as relatively temporary. An annual aberrometry assessment will allow for "perfect vision" tune-ups with contact lenses. Such adjustment with surgical procedures appears impractical or impossible. This is a blow to the benefit of refractive surgery because the primary competitive advantage of surgery is its claim to being permanent.
|
|
|
|
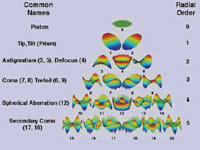
Figure 3. Three-dimensional optical path difference wave maps of the Zernike orders and
frequencies. |
|
Beware of Misleading Marketing
HOAs are unique to the individual eye. The term "fingerprint" or "snowflake" as a metaphor to HOA is appropriate. The combinations of aberrations allow for an infinite mathematical set of optical outcomes. For this reason, it's impossible for a one-size-fits-all lens to correct the aberrations of the human eye. Even so, manufacturers have begun making claims that their lenses correct the aberrations of the eye as well as of the lens.
It's possible to build in a correction for the induced spherical aberration of the lens based on its base curve and power. A nominal spherical aberration correction or, for that matter, a nominal coma correction may also be added. It's important for the practitioner to consider that these are standard values and the continuum of HOA measured in patients allows for wide variance from these standard values.
While the statements of correcting the aberrations of the eye make for nice marketing, the ultimate harnessing of wavefront technology is forecast to be in mass customization. In one form of mass customization, a measured diagnostic lens must be placed, an aberration measurement and simultaneous registration error assessment completed and the lens manufactured through incorporation of these data.
Let the Debate Begin
This article should stimulate speculation and debate. The movement has started. Technology is enabling a new modality. The future will reveal the data that is needed to encourage vision optimization with contact lenses.
At this point, it appears that we'll have the opportunity to apply the same precision, or greater, to prescribing contact lenses as we do to spectacle lenses and more importantly provide the equivalent (or greater) visual acuity with the advantages of freedom from spectacles.
To obtain references, visit www.clspectrum.com/references.asp and click on document #109.
Dr. Legerton practiced in San Diego for 26 years. He served as director of Clinical Research for Pilkington Barnes Hind and as a consultant to VISX and Paragon Vision Sciences. He has three patents issued for multifocal and aberration correcting contact lenses and two patents for excimer laser correction for presbyopia.