ALLERGY
Stopping the Itch: Relief for Ocular Allergies
Once you understand the allergic process and how to differentiate among ocular allergy conditions, you can relieve your patients' ocular itch.
By William Townsend, OD
Allergy is one of the most commonly encountered ocular immunologic disorders, and it's frequently associated with non-ocular allergic disease. To properly diagnose and manage the various forms of ocular allergy, we must first have a basic understanding of the immune cells, mediators and processes involved.
|
|
|
|
Figure 1. Vernal keratoconjunctivitis. |
|
|
|
|
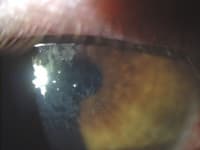
Figure 2. Atopic keratoconjunctivitis. |
|

|
|
| Figure 3. Giant papillary conjunctivitis. | |

|
|
| Figure 4. AKC four days after initiating treatment with cyclosporine. |
Understanding Allergy Basics
Austrian pediatrician Clemens von Pirquet coined the term "allergy" in 1906 from the Greek words "allos" (meaning "changed or altered state") and "ergon" (meaning "reaction or reactivity") to describe the unusually intense reactions some patients developed when injected with a second dose of horse serum antitoxin.
The terms "allergy" and "atopy" aren't interchangeable. Atopy is the hereditary tendency to develop immediate allergic reactions to innocuous substances such as pollen, food, dander and insect venoms. It manifests as hay fever, asthma or similar allergic conditions.
An estimated 60 percent of the 20 million to 40 million people in the United States who have allergic rhinitis (AR), the most common form of allergic disease, also suffer from allergic eye disease. Itchy, red edematous eyes and a stuffy, itchy nose characterize AR, or hay fever. Because of its close association with allergic eye disease, eyecare professionals should have working knowledge about AR.
Allergic Rhinitis Specifics
AR subdivides into seasonal allergic rhinitis (SAR), which occurs during pollen release from trees, grasses, weeds, etc., and perennial allergic rhinitis (PAR), which occurs during at least nine months of the year. SAR causes a rapid onset of symptoms such as itchy, runny nose; sneezing; and congestion. It presents after pollen exposure, occurs most commonly in the spring and fall and usually resolves after pollen exposure ends. PAR results from exposure to dust mite droppings, animal dander and molds and other environmental allergens that are continuously present. It's often difficult to diagnose because it may be masked by concurrent symptoms of sinusitis, respiratory infections and vasomotor rhinitis. Common symptoms of PAR include sneezing, a runny nose producing large amounts of clear fluid and nasal congestion. Itching is less prominent in PAR than in SAR. An estimated 20 percent of AR cases are SAR, 40 percent are PAR and 40 percent are mixed. PAR is less likely to cause the ocular symptoms of itching and irritation common with SAR.
How Ocular Allergies Occur
Sensitization begins when antigen-presenting cells (APC) such as those in the conjunctival mucosa become exposed to a specific antigen. Dendritic cells (Langerhans cells) are the principle APCs involved in primary immune responses; they obtain and process antigens in tissues, migrate to lymphoid organs and activate T cells. Macrophages are also APCs in the conjunctiva. APCs fragment allergen particles, which then present to B-cells, which become plasma cells that produce Immunoglobulin E (IgE) specific to the antigen. The Fc portion of the IgE molecules attaches to the surface of conjunctival mast cells.
The early-phase allergic response initiates when antigens bridge the gap between the Fab portions of the IgE molecules on a mast cell, causing granules of preformed mediators in the mast cell to fuse with the cell membrane; the mast cell then releases the granules into the surrounding tissue. Mast cells are the central figure in the early-phase allergic response. Two types of human mast cells exist based on the presence of the enzymes tryptase and chymase. The difference in these two mast cell types is vital in designing drugs for specific tissue such as conjunctiva.
Mucosal mast cells (MCT) contain tryptase, an enzyme specific to mast cells. Scientists haven't established its role in ocular allergy. Connective type mast cells (MCTC) contain both tryptase and chymase. Research has found only MCTC type mast cells in allergic conjunctivitis and giant papillary conjunctivitis (GPC); the majority of mast cells in vernal keratoconjunctivitis (VKC) are also of the MCTC variety. It's significant that MCTC cells are prevalent in skin, but of minimal importance in the lungs, suggesting that skin and eye allergy share many similarities.
The release of histamine into ocular tissue causes most of the symptoms classically associated with allergy. Within minutes, histamine binds to H1 receptors on blood vessels, inducing vasodilatation and thereby increasing vascular permeability. This results in conjunctival edema (chemosis). Histamine also binds to H1 receptors on nociceptive type-C nerves in the mucosa, leading to the release of neuropeptides such as substance P. The resultant itching and discomfort causes tearing that ultimately flushes allergens out of the eye.
Many inflammatory cells (including mast cells) release platelet activating factor (PAF), which increases platelet aggregation and vascular permeability and is chemotactic for eosinophils and neutrophils. In allergy, it causes increased hyperemia and chemosis and leads to migration of inflammatory cells into the affected tissue.
A relatively new finding is the contribution of conjunctival epithelial cells to the allergic reaction. The release of histamine stimulates these cells to release IL-6 and IL-8, two inflammatory cytokines with the potential for promoting the late-phase allergic response.
Early- and Late-Phase Allergic Responses
Mast cells solely moderate early-phase response, which occurs within minutes of exposure to the allergen and tends to produce sneezing, itching, clear rhinorrhea, conjunctival edema and injection. Most Type I hypersensitivity resolves after a few hours.
When the late phase occurs, it usually presents four to eight hours after allergen exposure and manifests as congestion, fatigue, malaise and irritability. Late-phase allergic reactions are considerably more serious and of higher morbidity than early-phase reactions. During the late phase, leukocytes (that mast cells initially stimulate or recruit) contribute significantly to the present signs and symptoms.
Eosinophils are motile and capable of phagocytosis, although this isn't their primary function. They're crucial in ridding the body of parasites, especially worms. Their presence in the eye during simple allergy results from mast cell-released chemotactic factors. Eosinophils, like mast cells, are granulocytes: Their cytoplasm contains granules whose contents include eosinophil major basic protein (MBP), eosinophil major cationic protein (ECP), eosinophil-derived neurotoxin (EPX) and eosinophil peroxidase (EPO). ECP and MBP are toxic to the epithelium and contribute to corneal damage that occurs in severe chronic allergic conditions. When released, they're destructive to parasites, cancer cells and, unfortunately, human tissue. Eosinophils are also an important source of leukotrienes, prostaglandins, cytokines and chemokines. Late-phase reactions play an important role in the pathophysiology of VKC and atopic keratoconjunctivitis (AKC).
Recognizing Ocular Allergic Conjunctivitis
Patients who have allergic conjunctivitis present with symptoms of ocular itching, conjunctival redness, chemosis, lid swelling and tearing that result from the early-phase reaction. The most consistent and prominent feature of allergic conjunctivitis is itching. The absence of itching suggests a causative factor other than allergy. Slit lamp examination frequently reveals papillae on the inferior and superior tarsal conjunctiva.
Allergic conjunctivitis is usually bilateral. One exception is the presentation of increased signs and symptoms on the side on which a patient sleeps. This phenomenon results from exposure to antigens deposited from the patient's hair onto his pillow during sleep. Another cause for unilateral presentation is manual introduction of an allergen to one eye, as in pet dander after a sensitized individual has handled a cat or other animal.
Chemosis is a frequent sign in allergic conjunctivitis. It's usually more dramatic in cases of acute allergy. Lid edema, which may result from H2 receptor site activation, also accompanies ocular allergic conjunctivitis.
Vernal and Atopic Keratoconjunctivitis
VKC and AKC are extreme expressions of atopy in the eye and adnexae. Both cause severe itching, mucous discharge, corneal involvement and, in some cases, visual loss. Base differential diagnosis between the two on age of onset, seasonal vs. perennial occurrence and, to a lesser extent, symptoms.
VKC tends to affect children and young adults. It's significantly more common in males until puberty, when the percentage of affected females increases until the ratio reaches 1:1 by the late teens. VKC tends to occur in the spring, hence the term vernal. Its incidence is higher in hot, dry climates, and it may involve Type I and Type IV hypersensitivity reactions. Mast cells, typical in Type I reactions, are present, but eosinophils are the prevalent inflammatory cell. CD4 T cells also appear in this condition.
Clinical features of VKC include bilateral, large upper tarsal (giant) papillae (Figure 1). Giant papillae at the corneoscleral limbus (Horner-Trantas dots), composed of degenerated epithelial cells and eosinophils, may occur with bulbar conjunctival involvement. Horner-Trantas dots are transient, with each manifestation rarely lasting more than one week. Corneal changes ranging from superficial punctuate keratopathy to sterile shield ulcer formation result from degranulation of eosinophils and subsequent release of MBP, ECP, EPX and EPO.
Approximately three percent of the population suffers from atopic dermatitis, and of these, approximately 25 percent have ocular involvement. The ocular manifestation of this condition is AKC (Figure 2). The clinical features of AKC are virtually identical to those of VKC, but two differentiating features are age of onset and patterns of occurrence. Age of onset ranges from 30 to 50 years, and unlike VKC, AKC is perennial. Atopic dermatitis manifests as intensely itchy red areas that appear on the eyelids and at the popliteal and antecubital flexures. Skin lesions show scales and crusts and are often macerated from repeated scratching by the affected individual.
Release of highly basic proteins can result in superficial punctuate keratitis, corneal neovascularization or a sterile shield ulcer. These lesions are susceptible to secondary bacterial infection including haemophilus influenza. Horner-Trantas dots may occur with AKC, but not as frequently as they occur in VKC. Long-term inflammation can result in significant vision loss. In advanced disease, patients may also develop anterior and posterior shield cataracts.
Giant Papillary Conjunctivitis
GPC is a common complication of lens wear and may result, to a lesser extent, from loose sutures, extruding scleral buckles and coated prostheses. In lens wearers, the presenting complaints are increased lens awareness, excessive lens movement and copious mucus production. GPC is more common in hydrogel wearers than in GP wearers. Experts have long considered it a Type 1 hypersensitivity reaction, but the finding of CD4 T lymphocytes suggests that a delayed hypersensitivity (Type IV) process may occur.
GPC patients frequently present with coated lenses that position under the lid and move with every blink. Lid eversion typically reveals papillae covering the tarsal surface (Figure 3). In long-standing GPC, scarring of the tops of the lesions appears clinically as white, rough aspices. GPC may present as bilateral, unilateral or asymmetrical.
Disposable and planned replacement contact lenses have significantly reduced the incidence of GPC, but recently, a resurgence has occurred with the use of 30-day silicone hydrogel lenses. GPC associated with these lenses tends to present as more localized in nature and is often less symptomatic than the GPC that develops from hydrogel lens wear.
One theory regarding the pathogenesis of GPC suggests that the accumulation of mucus, protein and other substances on the lens surface causes a Type I reaction to the denatured organic materials. Another theory suggests that chronic rubbing of the roughened surface of coated contact lenses results in mast cell degranulation and GPC development.
Treatment Options for Ocular Allergy
Many individuals suffering from ocular allergy never consult an eyecare provider because available over-the-counter medications permit self-treatment. Visine-A (Pfizer), Opcon-A (Bausch & Lomb) and Naphcon-A (Alcon Laboratories) contain naphazoline HCl, a direct-acting sympathomimetic agent that produces vasoconstriction (resulting in decreased conjunctival congestion) and pheniramine maleate, an antihistamine that acts directly on receptors. They effectively reduce itching and congestion caused by allergic conjunctivitis, but their effects may last only two hours. These drops have little effect on long-term swelling and injection, and because they're preserved with benzalkonium chloride (BAK), their continual, frequent use may be toxic to the ocular surface.
Prescription drugs for allergy fall into one of five categories:
1. Antihistamines
2. Mast cell stabilizers
3. Combined antihistaminic and mast cell agents
4. Steroids
5. Immunomodulators
Antihistamines Levocabastine HCl ophthalmic suspension 0.05% (Livostin, Novartis Ophthalmics) and emedastine difumarate ophthalmic 0.05% (Emadine Alcon) are H1-selective new-generation antihistamines that have greater potency and longer duration of action (six hours) than phenirimine. Patients must use them qid. Both medications contain BAK. The greatest drawbacks to antihistamines are their need for frequent dosing and their inability to prevent further mast cell degranulation.
Mast Cell Stabilizers These drugs aim to prevent the degranulation and release of mediators. Drugs in this class include cromolyn (Crolom, B&L and Opticrom, Allergan), lodoxamide (Alomide, Alcon) and pemirolast (Alamast, Santen). The manufacturers recommend all of these products for qid dosing. Nedocromil (Alocril, Allergan) has an indication for bid dosing.
Because of the presence of histamine and other mediators in eyes that are already suffering from allergy, it may require days or weeks for mast cell stabilizers to achieve clinically significant reduction of symptoms. It's best to prescribe these agents before the onset of allergy symptoms. They also have a place in managing more severe forms of the late-phase allergic reaction.
A recent study has called into question the mechanism by which these drugs achieve clinical response. Yanni et al (1997) demonstrated little inhibition of human conjunctival mast cells by cromolyn, pemirolast or nedocromil, suggesting that the effect of these drugs may occur through another mechanism.
Combination Drugs The development of drugs that contain both antihistamines and mast cell stabilizers has become a significant advance in managing allergic eye disease. Medications with this designation include ketotifen fumarate ophthalmic solution, 0.025% (Zaditor, CIBA Vision), azelastine HCl ophthalmic solution 0.05% (Optivar, MedPointe Healthcare, Inc.), olopatadine HCl ophthalmic solution 0.1% (Patanol, Alcon) and epinastine HCl ophthalmic solution 0.05% (Elestat, Inspire Pharmaceuticals/Allergan). In addition to the anti-itch benefits of topical antihistamines, the mast cell-stabilizing properties of these medications help reduce long-term symptoms of ocular allergy. You can prescribe all of these drops bid, which is much more convenient than the qid dosing for most antihistamines.
Steroids These drugs interfere with protein synthesis and thus thwart many of the symptoms of allergic eye disease. Steroids are potent anti-inflammatory agents, but they cause numerous side effects that make their long-term use in non-sight-threatening disease questionable. Newer site-specific steroids have reduced -- but not eliminated -- complications such as intraocular pressure elevation, cataract formation, reduced immune response to pathogens and exacerbation of herpes simplex keratitis. Loteprednol etabonate 0.5% (Lotemax, B&L), loteprednol etabonate 0.2% (Alrex, B&L) and rimexolone 1% (Vexol, Alcon) are three site-specific steroids that you can administer for short-term treatment of allergic eye disease.
Immunomodulators Cyclosporine is an immunomodulator that has found great acceptance as a treatment for inflammatory dry eye syndrome. It works by specific, reversible inhibition of T1-helper lymphocytes. The exact mechanism of action of cyclosporine on eosinophil activation in allergic eye disease isn't well established, but cyclosporine has proven to effectively treat both AKC and VKC.
Specific Therapies for Allergic Eye Disease
Successful management of any disease depends on patient compliance with an effective treatment. Convenience can significantly improve compliance. Patients can improve any allergic condition by reducing their contact with the suspected allergen, but it's often difficult to actually accomplish this.
Seasonal and Perennial Allergic Conjunctivitis The primary difference between these two conditions is duration of symptoms. The bid dosing of combination antihistamine/mast cell stabilizers make them a convenient and effective treatment option. Cold compresses and frequent use of an eye wash/irrigation solution (without BAK) to reduce allergen-eye contact also help manage these conditions.
Using only oral antihistaminic agents for ocular allergy is of questionable value. These agents cause systemic effects including drowsiness, drying and difficulty with urination. The drying effects on the eye tend to concentrate allergens in the tear film, thus exacerbating ocular symptoms. If you must prescribe these agents, then also prescribe frequent irrigation or use of non-preserved rewetting drops.
AKC and VKC These conditions are far more complicated in etiology and severity than allergic conjunctivitis. The corneal complications and potential for vision loss secondary to release of basic proteins from eosinophils necessitates immediate and decisive intervention. AKC and VKC are two conditions that indicate topical steroid therapy every two to four hours. Rapidly taper the steroid as soon as you note improvement. Administering topical mast cell stabilizer/antihistamine drops bid can also help quell the extreme itching that accompanies these disorders. I typically prefer Patanol and Elestat.
A relatively new therapy in managing AKC and VKC is topical cyclosporine A (Restasis, Allergan) (q12h), which I've found has helped reduce or eliminate the signs and symptoms of these conditions. Figure 4 shows an AKC patient after four days of cyclosporine treatment. The literature now supports using this drug to manage AKC and VKC. Patients who have these conditions also benefit from mast cell stabilizers. The consistent benefit of these medications in such cases suggests anti-inflammatory action as a possible mechanism of action for these agents.
In patients who have severe atopic lid disease accompanying the eye signs, using topical tacrolimus (Protopic) ointment q12h is an excellent way to manage dermal manifestations of atopic disease. This immunomodulator is 100 times more efficacious than cyclosporine, but its use is currently limited to dermal application.
GPC Begin GPC therapy with cessation of all lens wear for one week or longer if possible. If the patient wears conventional lenses, then consider shifting to planned replacement or disposable lenses. Medical management includes using a short-time pulse dose of topical steroids. GPC patients also benefit from combination antihistamine/mast cell stabilizers. When the eye is quiet, consider tapering and eventually discontinuing the topical steroid. Long-term management of GPC may require ongoing treatment with pre- and post-lens wear dosing of the topical combination product. Careful patient education and instruction regarding the cause and nature of GPC can encourage the patient to comply and remain faithful to the recommended regimen.
Conclusion
Practitioners need to recognize the different types of ocular allergy conditions so they can treat them appropriately. The plethora of new information available on the ocular immune system can help us understand and evaluate these conditions with confidence and authority, and better, more effective treatment options are available to help manage these conditions.
To obtain references, please visit http://www.clspectrum.com/references.asp and click on document #114.





