TORIC FITTING
Reassessing Toric Soft Lens Fitting
Forget earlier techniques -- this article reviews what you need to know to find success in toric soft lens fitting.
By Graeme Young, PhD, MPhil, FCOptom, DipCL, FAAO and Sheila Hickson-Curran, BSc (Hons), MCOptom, FAAO
Fitting toric soft contact lenses was once a specialist activity often only embarked on as a last resort. However, the proliferation of well-designed, accurately manufactured, molded soft torics has simplified the procedure and brought these lenses into mainstream contact lens practice. Fitting toric soft lenses is simpler and more predictable than we thought. It's therefore time to reassess our understanding of these lenses and how we fit them.
When to Correct Astigmatism
The decision to correct astigmatism involves weighing the disadvantage of compromised vision against the extra cost, chair time, effort and the risk of possible failure in fitting toric lenses. For with-the-rule (WTR) astigmats who have moderately high myopia, undemanding visual needs and require only part-time wear, little incentive exists to correct small amounts of astigmatism.
One traditional guideline suggests that we leave astigmatism equivalent to one-quarter of the sphere power uncorrected (1.50DC in the case of a 6.00D myope). Guidelines, however, are merely that and we should take a number of factors into account (Table 1).
|
|
|
|
Figure 1. Conflicting actions of the upper and lower lids during the blink. |
|
Improvements in toric soft lens design and manufacturing accuracy over the past few years have led to 0.75D cylinder powers becoming widely available; most monthly and two-week replacement torics are now available in this power. This has resulted in the reassessment of the rule of thumb that suggests considering correction for 1.00D or more of astigmatism. It still remains a matter of judgement, but the balance has shifted toward correcting lower levels of astigmatism.
Often we can demonstrate the improvement in vision to patients using a phoropter, although in other cases, patients can only appreciate this once they wear the lenses. Thus, a useful approach is to dispense trial lenses and to question the patient about his vision in challenging situations such as night driving whenever possible.
Understanding Stabilization
A well-designed toric soft lens will adopt a repeatable orientation position on a wide range of eyes. The lens settles and maintains a stable orientation position because of the influence of the lids. In the case of prism-ballasted lenses, gravity has some effect, but this is negligible when the prism base-apex line is close to the vertical (<30 degrees).
Both the upper and lower lids influence orientation. However, because the lids move in mutually perpendicular directions, they can influence orientation in different ways (Figure 1). In most cases, the downward force of the upper lid acts on asymmetric lens thickness profiles to force the lens into place. Research has shown that there is some correlation between the configuration of the upper lid and orientation for prism ballasted lenses: Eyes having an outer canthus higher than the inner canthus tend to show inferior-nasal rotation. Unfortunately, however, the correlation isn't strong enough to allow an accurate prediction of lens orientation on a given eye. Part of the reason for this is the conflicting influence of the upper and lower lids. As a consequence, we need to trial fit soft torics to determine the orientation on each individual patient's eyes.
Toric soft lenses rarely adopt a fixed position. Typically, their orientation position, when observed for a few minutes, varies by 5 degrees to 10 degrees. When fitting toric soft lenses, it's therefore better to note a range of orientation positions (zero degrees to 5 degrees inferior-temporal) rather than a single value. As well as being more precise, this measurement is helpful in deciding which cylinder axis to select when a lens is only available in limited parameters.
Another useful clinical technique is to observe the orientation position while the patient performs forced blinking and version movements. If the lens remains relatively stable during this simulation, then it should provide relatively stable vision.
Back Surface Toric Designs and Orientation
There is no evidence to suggest that back surface toricity encourages orientation stability. Toric soft lens pioneers in the 1970s tried toric lenses with no method of stabilization other than back surface toricity and quickly discovered that this wasn't enough to achieve stable orientation. Examining the geometry of toric soft lenses helps to explain this: For a 2.00DC back surface toric design (back optic zone diameter = 10mm), the difference in sagittal depth in the two major meridians is only 10µm.
No consensus exists in the literature as to whether front or back surface toric contact lenses give the best clinical performance. Most current molded toric soft lenses incorporate a toric back surface. Probably a more important factor governing whether a design shows good rotational orientation is the distribution of lens thickness in the blink zone (palpebral aperture) and how these areas of thickness interact with an individual's eyelids and blink dynamics.
|
|
|
|
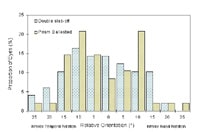
Figure 2. Frequency distribution graph of orientation for two soft toric contact lens designs. |
Direction of Rotation
Only a small proportion of lenses orientate in the zero rotation position and, contrary to the popular belief that lenses always rotate base nasally, a high proportion of toric soft lenses orientate inferior temporally (Figure 2). Most toric soft lens designs orientate, on average, within five degrees to 10 degrees of the zero position. However, because different designs interact with the lids in different ways, we can't expect all designs to orientate in the same position on a given eye.
When ordering a toric soft lens based on spectacle prescription alone, it's usually advisable to order the first lens assuming no rotation. If, as frequently happens, the spectacle cylinder axis falls between available axes, then with most designs, it's best to assume inferior-temporal rotation. Exceptions to this rule might occur with eye shapes that show a marked inclination in one direction or another.
Selecting Toric Soft Lenses
Our approach to fitting toric soft lenses has changed with the increasing use of disposable lenses. It's not so common to use trial fitting sets in a single power to select the first lens.
So-called empirical fitting involves ordering contact lenses based on the patient's refraction without applying lenses at the initial visit. When ordering empirically, therefore, the first lenses are essentially the diagnostic contact lenses. Selecting such lenses requires a number of adjustments:
- Correct for vertex distance
- Round down to the nearest available cylinder power
- Round to the nearest cylinder axis
A prudent measure when ordering diagnostic lenses is to order at least two lenses for each eye with different axes.
Studies have shown the empirical approach to be as effective as ordering from trial lenses. Some lenses show more predictability, sitting close to the zero position in a high proportion of eyes and rarely sitting obliquely, and this improves the chance of ordering the correct lens the first time. However, the ideal approach is to fit and dispense lenses at the initial visit from an extensive diagnostic kit (400 lenses). Such an approach is becoming standard practice with toric soft lenses as with spherical lenses. Clearly, this saves on administration and avoids at least one extra appointment.
Fitting Toric Soft Lenses: Loose or Tight?
Some practitioners advocate fitting toric soft lenses slightly loose to allow the lens to reorient more quickly when dislodged from its normal position. Others favor a tight fit to encourage stability. It's true that loosely fitting toric lenses tend to show poor stability, but on the other hand, tightly fitting lenses show poor reorientation. Ideally, toric lenses should show the same basic fitting characteristics as well-fitting spherical lenses.
Many current toric soft lenses are only available in one base curve, designed to fit the widest possible range of eyes. Inevitably though, one lens design doesn't fit all eyes and it's therefore necessary to use a range of toric lens designs.
Determining the Required Toric Power
Traditionally, selecting the appropriate power required a trial fitting and over-refraction to make allowances for unpredictable lens flexure and a possible tear lens. This practice may well have been necessary in the era of thick lenses.
Nowadays, the optimum lens power corresponds closely to the refraction and, with a correction for vertex distance and lens rotation, we can calculate it from the spectacle prescription. When a lens fails to provide good vision, it's unlikely the result of some unfathomable correction factor and is almost invariably because of an error in either refraction, orientation or lens manufacture.
One of the most common errors that occurs when determining a toric soft contact lens power is neglecting to compensate for back vertex cylindrical power, as well as for spherical power. A good rule of thumb to follow is to calculate the ocular refraction when the sphere power or the sphere plus cylinder power combined is >4.00D. With many prescriptions, the cylinder may decrease when corrected for vertex distance, although the cylinder will increase with some prescriptions (plus sphere and minus cylinder).
How Accurate are Toric Soft Lenses?
The recommended tolerances used for toric soft contact lenses are, in most cases, twice those for spectacle lenses. For lower-power lenses, the ISO tolerance is ±0.25D for both the sphere and cylinder power and ±5 degrees for axis. However, unlike spectacle lenses, soft toric contact lenses often fall outside of these recommended tolerances. The manufacturing accuracy of molded contact lenses is usually better than that of lathed toric contact lenses.
Interestingly, with cast-molded lenses, cylinder power is typically more accurate than sphere power. This is because with molded contact lenses, a number of factors govern the sphere power (front and back surface curvature as well as lens thickness), whereas only the curvature of one surface governs cylinder power. Clearly, using a brand of lens that has a good record of manufacturing quality and accuracy helps to simplify fitting.
How Helpful is Over-refraction?
When toric soft contact lenses fail to give the expected vision, one option is to reorder the lens based on a sphero-cylindrical over-refraction and the presumed power and orientation of the existing contact lens. Specially designed calculators and spreadsheet programs are available to help with the calculation. However, we should use these with caution, as the relatively wide manufacturing tolerances for toric soft contact lenses, coupled with the difficulties in measuring a varying refraction, can result in confusion. The manufacturing tolerances for toric soft contact lenses are such that a lens can occasionally produce sub-standard vision while still being within tolerance. Trying to over-refract and reorder based on an oblique cylinder calculation often only adds to the confusion.
A better approach to solving vision problems is to systematically check for possible errors (Table 2). Misorientation can explain most cases of poor vision with toric lenses. We can often confirm this by having the patient view a letter chart while manually rotating the lens to the intended orientation position. An improvement in vision indicates that we should replace the lens, taking into account the actual orientation position. Other factors to consider are whether the original refraction was correct or whether the lens power is correct.
Measuring Toric Soft Lenses In-office
With practice, we can make accurate measurements of soft lens power using a normal vertexometer. This is easier with a projection vertexometer on which we can rest the lens without support, although it's still possible with older types of instruments. The procedure is as follows:
1. Rest the lens on a tissue convex side down
2. Dab two or three times with another wipe
3. Carefully place on the vertexometer
4. Measure in the usual way
Occasionally, toric soft lens orientation marks don't correspond to the base-apex line. Check this by locating the marks at six o'clock and viewing the vertex mires. With the lens positioned on the vertexometer with the orientation marking in the six o'clock position, the mire image should show the prism at base down 90 degrees.

Sheila Hickson-Curran is principal research optometrist at Vistakon, a division of Johnson & Johnson Vision Care, Inc. She has conducted clinical and research work in the U.K. and in Australia. She has a special interest in contact lens design and the correction of astigmatism.
|
TABLE 1 Deciding Whether to Correct Astigmatism |
|
| FACTORS | ASTIGMATISM LESS IMPORTANT WHEN: |
| Sphere power | Higher sphere power |
| Axis of astigmatism | With the rule |
| Previous correction | Previously uncorrected w/o problems |
| Usage | Part-time wearer |
| Visual tasks | Undemanding |
| Eye dominance | Astigmatism lowest in dominant eye |
|
TABLE 2 Problem-Solving Checklist for Poor Vision |
|
|
Recheck the following in the order shown. |
|
| CHECK | ACTION IF INCORRECT: |
| 1. Lens orientation | Rotate lens on eye |
| 2. Lens stability | Try alternative toric design |
| 3. Spherical over-refraction | Replace with modified sphere |
| 4. Lens prescription | Reorder/replace |
| 5. Lens markings (prism) correctly positioned | Replace |
| 6. Sphero-cylindrical over-refraction | Replace based on results |
|
|
Top Tips for Fitting Toric Soft Contact Lenses |
|
|