contact lens case reports
Analyzing
Unilateral Complications
Patient GS is a 23-year-old male with a four-year history of uneventful soft contact lens wear. He presented to our clinic with symptoms of foreign body sensation OS, burning, itching, mild photophobia and overall lens intolerance. He was compliant with his two-week planned replacement lens schedule, and his lens care regimen consisted of nightly disinfection with a multipurpose lens disinfection system. He denied the use of any other lens care products or supplemental lubricating drops.
|
|
|
|
Figure 1. GS's left eye with mild bulbar injection. |
|
|
|
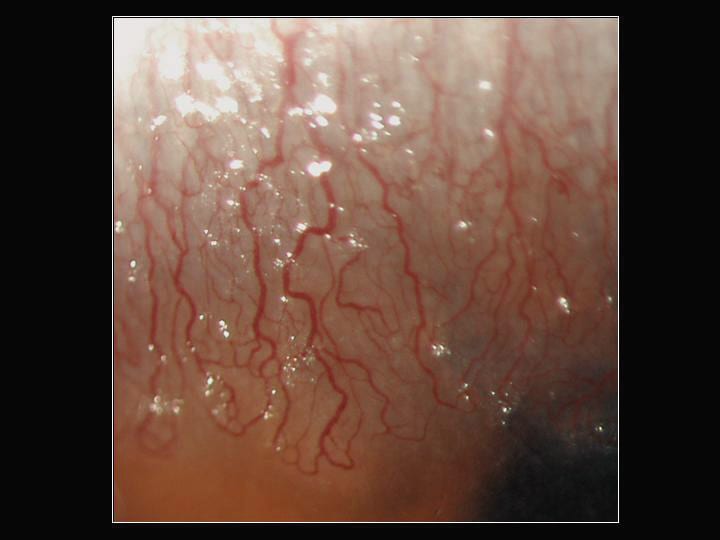
| Figure 2. Location and extent of the neovascularization. | |

|
|
| Figure 3. Elevated nodules just anterior to the neovascularization. |
Slit lamp examination of the symptomatic left eye showed mild superior bulbar inflammation as well as significant superior neovascularization with lipid leakage (Figures 1 and 2). The superior corneal epithelium was irregular with small, elevated gelatinous nodules adjacent to the areas of neovascularization (Figure 3). We also noted significant punctuate staining confined to the superior one-third of the cornea.
Bilateral vs. Unilateral
The etiology of a bilateral adverse event is often easy to explain. It may relate to an underlying problem such as dry eyes, allergies or a solution sensitivity. Or it may be secondary to a lens material and/or design limitation resulting in hypoxia or an improper lens fit. More often than not, these anomalies present bilaterally and may or may not be symmetric.
However, when a non-infectious, adverse event is completely unilateral, determining the cause of the condition and providing the correct diagnosis becomes significantly more difficult.
Treating Unilateral Conditions
In recent years, the eyecare community has identified a number of contact lens-related conditions that can result in significant superior conjunctival and/or corneal involvement, including lens-induced superior limbic keratoconjunctivitis, advancing wave-like epitheliopathy and lens-induced epithelial dysplasia. While some experts suggest more invasive treatments such as silver nitrate or conjunctival scraping or resection, we've found that it's best to discontinue lens wear completely and prepare the patient for a three- to six-month course of preservative-free lens lubricants. This simple therapy is slow, yet has proven successful in managing many superior limbal complications of obscure etiology.
Patrick Caroline is an associate professor of optometry at Pacific University and is an assistant professor of ophthalmology at the Oregon Health Sciences University. He is also a consultant to Paragon Vision Sciences and SynergEyes, Inc. Mark André is director of contact lens services at the Oregon Health Sciences University and serves as an assistant professor of optometry at Pacific University. He is also a consultant for Alcon Labs, CooperVision and SynergEyes, Inc.




