COMPLICATIONS AND
CODING
Complications, Care and Coding
See case by case how to diagnose, manage
and code contact lens complications.
There are many reasons for anterior segment complications including trauma, inflammation, infection, allergic response, poor contact lens-to-cornea fitting relationship and, of course, patient noncompliance. Listening to your patients' needs and providing continuous patient education can help create a relationship that will benefit both the patient and your practice. Yet, despite our best efforts, complications are sure to arise, and knowing how to manage and code properly will make your chair time both efficient and profitable.
|
|
|
|
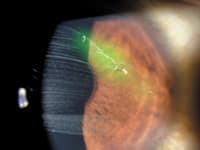
Figure 1. A corneal infiltrate resulting from GP-induced VLK. |
|

|
|
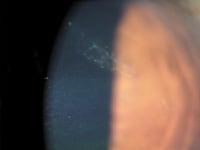
| Figure 2. VLK resolution and small intracorneal hemorrhage. | |

|
|
| Figure 3. Fluorescein reveals an imprint of a contact lens. | |

|
|
| Figure 4. Superior-central infiltrate with overlying stain. | |
|
|
| Figure 5. Superficial corneal abrasion consistent with a paper cut. | |
|
|
|
Figure 6. Resolution of paper cut following treatment with topical fluoroquinolone. |
Case 1
Because of our large university-based location, we frequently see corneal complications secondary to contact lens wear and ocular trauma. A 29-year-old college student presented with left eye complaints of nasal conjunctival redness, mild eye irritation and a "white spot" that she'd had on her cornea for two days. She reported no pain, photophobia or discharge. She had felt a
"bump-like sensation" and an overall increase in GP lens awareness of the left eye for the previous two weeks, but continued to wear her contact lenses 16 hours each day. She discontinued contact lens wear after observing the white spot on her cornea and subsequently noticed minimal improvement in symptoms.
She reported a history of corneal ulcers in both eyes and giant papillary conjunctivitis while wearing monthly replacement soft contact lenses and two-week disposable contact lenses. She was a college student who majored in dance and instructed yoga. Our records indicated that she was a successful daily disposable lens wearer, but found them cost prohibitive. She had successfully worn aspheric GP lenses for several years. She reported no allergies and her health history was unremarkable.
Slit lamp biomicroscopy OD revealed faint midperipheral corneal scars at 10 o'clock and four o'clock from previous corneal ulcers. The left conjunctiva had moderate injection adjacent to the nasal limbus with overlying fluorescein stain. A corneal infiltrate was present from eight o'clock to 10 o'clock with elevated, staining, hyperplastic epithelium and vascularization throughout (Figure 1).
The right GP lens lid-attached, centered and showed slight central pooling and adequate edge lift around all 360 degrees. The left GP lens lid-attached, but centered nasally with the blink, with the nasal lens edge overlying the corneal desiccation. We noted slight central pooling, midperipheral bearing and minimal nasal lens edge lift with adequate edge lift elsewhere.
We diagnosed vascularized limbal keratitis (VLK) OS. Grohe and Lebow first described VLK in 1989. It's a peripheral corneal disorder induced by GP daily or extended wear and associated with large overall lens diameters, minimal edge lift designs and steep base curve-to-cornea fitting relationships. Signs and symptoms include peripheral corneal desiccation, infiltration and inflammation as well as surface erosion, discomfort and decreased wearing time.
The treatment goal is to alleviate the mechanical irritation with ocular lubricants and GP lens design changes such as decreasing the overall lens diameter, flattening the base curve and creating a wider, flatter peripheral curve. Other fitting options include a large-diameter GP lens with increased edge lift or a soft contact lens that covers the area.
We advised our patient to discontinue contact lens wear and prescribed a nonpreserved artificial tear and a steroid suspension. We scheduled a return visit in one week or sooner should signs/symptoms increase. The etiology appeared both mechanical and inflammatory.
Evaluation and Management (E/M) Coding Accurate E/M coding consists of three key components:
1. History
2. Examination
3. Medical decision making
With an easy-to-use coding guide sheet, coding for this patient is easy to determine. Many practitioners would bill this first visit as a level 2 (99212) established E/M visit and undercharge for their services. A level 4 (99214) is really more appropriate. My records indicated a detailed history, expanded problem-focused examination and moderate-complexity decision making. A 99214 established E/M code requires that you have two of the following three items:
1. Detailed history
2. Detailed examination
3. Moderate-complexity decision making
It's important to code other procedures performed when medically necessary as well, such as external ocular photography (92285), which in this case included interpretation and report for documentation of medical progress.
Case 1, Visit 2 Our patient cancelled her first appointment and returned two weeks later, reporting less redness and no irritation OS. The large corneal infiltrate showed significant improvement, was mildly elevated, had trace staining and was vascularized throughout. We noted a small intracorneal hemorrhage at this visit (Figure 2). We instructed the patient to continue the ocular lubricant and to discontinue the steroid. We advised her to return in one week for a comprehensive examination and contact lens fitting.
My records indicated a level 3 E/M code (99213), in which practitioners must document two of the following three components:
1. Expanded problem-focused history
2. Expanded problem-focused examination
3. Low-complexity decision making
We also billed external ocular photography, 92285 to show resolution of the VLK and to document the intracorneal hemorrhage.
Case 1, Visit 3 We successfully fit our patient into a daily wear silicone hydrogel contact lens because of her concerns of recurrence of VLK, history of corneal ulcers associated with other soft lens options and financial issues associated with soft daily disposable lenses. The soft lens covered the affected peripheral cornea, eliminating any mechanical sheering forces.
We coded and billed the following:
• Comprehensive eye examination (92014)
• Contact lens fitting (92310)
Case 2
A 20-year-old college student first presented to our clinic noticing redness and complaining of a foreign body sensation OD for two days after a weekend getaway in Canada. He had removed his soft contact lens, cleaned it with an unknown multipurpose solution and reapplied it. The irritation persisted.
He was unsure what brand of contact lens he was wearing and replaced them every three to four weeks with extended wear one night a week. He had no backup spectacles and wore his contact lenses 15 hours a day. His last full eye examination was three to four years ago, and he obtained his contact lenses via the Internet.
We noted circumlimbal injection on both eyes on gross examination. The contact lenses exhibited minimal to no movement. Slit lamp biomicroscopy revealed a small, superior-central foreign body on the right cornea as well as several small midperipheral infiltrates scattered from three o'clock to nine o'clock. An imprint of the contact lens appeared with fluorescein on both corneas (Figure 3). We noted corneal vascularization in all 360 degrees, as well as limbal irregularity highlighted by positive and negative staining on both eyes.
We removed the corneal foreign body with irrigation and prescribed fluoroquinolone drops qid to treat the residual abrasion. We advised him that his poor contact lens fit and poor compliance put him at risk for future inflammation, infection and possible vision loss. We advised him to get a full eye examination and have his contact lenses refit.
My records were consistent with a detailed history, expanded problem-focused examination and moderate-complexity decision making, indicating a new level 2 E/M code (99202), in which you must meet all of the following:
1. Expanded problem-focused history
2. Expanded problem-focused examination
3. Straightforward decision making
You can code this visit in several ways. You could bill the office visit alone, 99202. You could also add a –25 modifier to the 99202 and then, as a separate line item, bill for the corneal foreign body removal without slit lamp (65220). Each procedure code in this case should have a separate diagnosis code. A third option is to bill for the corneal foreign body removal alone. Coupling the office visit with a surgical code often results in denials. For this case, I also billed a 92285.
Case 2, Visit 2 Our patient returned the following day as advised, wearing no lens OD and wearing the soft contact lens OS. The small corneal abrasion had healed, but the infiltrates remained OD. Both eyes still demonstrated circumlimbal injection. We performed a manifest refraction and a gave him a spectacle prescription.
My records showed a problem-focused history, expanded problem-focused examination and low-complexity decision making consistent with a 99212. In addition, the refraction, CPT 92015, was a separate billable procedure that we performed that day.
This patient returned for one more follow-up visit in which we discontinued all medications and advised him to not wear his poor-fitting contact lenses and to return for a comprehensive eye examination. It probably comes as no surprise that he didn't return for more than a year when he came in with a black eye after being struck on the left eyelid with a water ski. The patient was still wearing the same type of contact lenses, replacing them after several months with several days of overnight wear a week. He had several corneal infiltrates. He even mentioned modifying his own contact lens powers online to improve his vision.
This patient had two annual visits to our practice, both for ocular injury and not for routine eye care or even for symptoms related to poor contact lens compliance. However, no eyecare practitioner could have ignored the obvious signs of contact lens abuse and contact lens-related acute red eye. It's extremely important to document such events, as well as how you educate the patient, in the medical record.
Case #3
A 19-year-old college student first presented to our practice with complaints of left eye blur, photophobia and irritation of four-days duration. He discontinued GP contact lens wear with the onset of symptoms. He hadn't seen his previous eyecare practitioner in four years. The right GP contact lens was four years old, and he'd replaced the left GP lens three months prior after breaking it. The original practitioner hadn't evaluated the contact lens fit or ocular health in four years and sent the new GP lens without a health assessment. The patient had worn the contact lenses on an overnight bus trip five days earlier and experienced some irritation the following day. Slit lamp examination revealed a 0.5mm superior-central infiltrate with overlying stain on the left cornea (Figure 4). Visual acuity with spectacles was 20/15 OD and 20/50 OS. Pinhole acuity was 20/30 OS. We presumed that the infiltrate was a sterile corneal ulcer because of the lack of anterior chamber reaction, significant pain or photophobia after four to five days of onset. We prescribed a fourth-generation fluoroquinolone and instructed the patient to return the following day.
My records indicated a detailed history, expanded problem-focused examination and moderate-complexity decision making, consistent with a 99202. We also billed a 99285.
The patient returned for two visits over the next seven days. The corneal ulcer healed, forming a scar, and the visual acuity improved to 20/25+. We advised the patient about the importance of comprehensive vision care, and he chose to resume care with his previous eyecare practitioner. We don't know to what extent patient noncompliance or practitioner negligence played in the development of this GP-induced central corneal ulcer. The incidence of infectious ulcerative keratitis with GP wear is rare, but you should never overlook the importance of comprehensive eye examinations and corneal health evaluations with contact lens wear.
Case 4
A 20-year-old college student presented with a 30-minute history of mild pain and mild blur of the left eye. He expressed concern that he had given himself a paper cut on his eye. Visual acuity OS was 20/25 and the pain was a 4 on a scale of 1 to 10. Slit lamp biomicroscopy revealed a superficial abrasion over the left pupil with a jagged diagonal epithelial defect consistent with a paper cut (Figure 5). We applied a bandage contact lens to reduce the pain and to protect the corneal epithelial cells from the eyelid. We also prescribed a topical fluoroquinolone.
We billed a 99202 and a 92285. In addition, we also billed for fitting of a contact lens for the treatment of a disease (92070). This included the supply of the contact lens.
The following day the patient's visual acuity had returned to 20/20 and only trace corneal staining remained (Figure 6).
Completing the Care Circle
Patient care doesn't end with the assessment and plan. The complete circle of patient care consists of patient history, patient examination, thought process and decision making, medical record documentation and coding and billing for your services.
Ongoing care, recall and regular re-education about proper lens care, hygiene and preventive eye care may prevent these complications in the future. To make sure you're compensated for your thinking, medically necessary care and documentation and to make your chair time worthwhile, code these visits properly.
Click here for a copy of the code sheet that we use for billing.
To obtain references, visit http://www.clspectrum.com/references.asp and click on document #115.

|
Dr. Mack is the clinic director and a clinical associate professor at The Ohio State University College of Optometry. |

|
Dr. Curtis is a clinical assistant professor at The Ohio State University College of Optometry. |




