discovering dry eye
Understanding
Tear Film Stability
BY JASON J. NICHOLS, OD, MPH, PHD
A major goal of clinicians and scientists over the past 10 to 15 years has been to develop the holy grail of clinical tests for dry eye disease. Indeed, we've made significant progress in understanding dry eye symptoms, and several validated survey instruments are available to assess not only dry eye symptoms, but also the impact of dry eye disease on a patient's quality of life. We've also made strides in understanding some of the "basic" etiologies of dry eye disease.
However, there's somewhat of a paucity in the development of new clinical tests for dry eye. Although it seems reasonable to diagnose dry eye based on symp toms alone (as is usually the case in clinical practice), "symptoms of ocular discomfort" represent only one aspect of dry eye disease (as defined by the National Eye Institute/industry workshop report from 1995). Symptoms aren't traditionally associated with tear deficiency or excessive tear evapor ation and damage to the exposed surface of the eye.
|
|
|
|
Figure 1. |
Testing Tear Film Function
Historically, tests of tear film function fall into two categories. The first group relates to tear film production (do the appropriate glands produce adequate quantities of the various tear film components). The second relates to tear film stability (does the tear film form a stable, uniform layer that resists breakup and dry spot formation). If a patient holds his eyes open long enough, the tear film will start to destabilize and a dry spot will form on the ocular surface. At some point in this process, the eye might start to feel uncomfortable.
While tremendous variability exists in this process, we generally measure tear film stability through tear film breakup times (TBUTs). You can measure TBUTs with fluorescein (invasive) or without fluorescein (noninvasive); typical cutoff values for these tests are 10 seconds and up to 15 seconds, respectively. You should take and average three TBUT measurements to reduce random noise associated with tear film stability and to derive a more precise estimate. While TBUT tests are useful in clinical practice, again, the measurements are variable and subjective.
New Methods Provide Insight
More recently, noninvasive optical techniques such as interferometric systems and optical coherence tomography have allowed for a more quantitative insight into tear film thinning and have furthered our understanding of the tears in a physical sense. Such new methods provide valuable information regarding tear film flow, decay and stability.
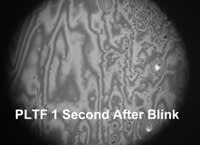
One such method, based on an interferometric principle known as "thickness-dependent fringes," is helping researchers to understand the wettability of contact lens materials, solutions and rewetting drops in-vivo. Figure 1 shows an individual's pre-lens tear film. As you can see, the tear film of a "normal" subject becomes significantly altered (dewetted) just eight seconds following the blink. It's likely that such tear film de-stabilization occurs more quickly in patients who have contact lens-related dry eye. Future studies will yield progress and insight into these important issues.
Dr. Nichols is assistant professor of optometry and vision science at The Ohio State University College of Optometry.